Secondary survey
1. Introduction
After resuscitation and stabilization of the patient, a head-to-toe investigation is needed to ensure that all injuries are diagnosed.
In this phase, adjuncts like tubes, drains and diagnostic tools are used.
This text will focus on the pelvic area. For a complete overview of the secondary survey we direct you to the ATLS® courses and manual.
Emergency care for pelvic ring injuries should be available and preplanned at every trauma hospital. Patients with complex pelvic ring injuries may need to be referred to a specialized center.
2. Assessment of the pelvic area in patients with a pelvic fracture
Physical examination
If the patient is conscious, ask about discomfort or pain in the pelvic area.
The patient is visually inspected to identify:
- Wounds
- Deformity
- Swelling
- Bruising
In case of open fractures, antibiotic administration should begin immediately.
Posterior pelvic wounds in the perianal region may disrupt the sphincter and cause bleeding.

Apparent deformation might be seen in severe displaced pelvic fractures.
Wide displacement of the posterior pelvic arch (left) is associated with increased blood loss.

Swelling and bruising are typical signs of fracture seen in the scrotum/labia majora/perineum area.

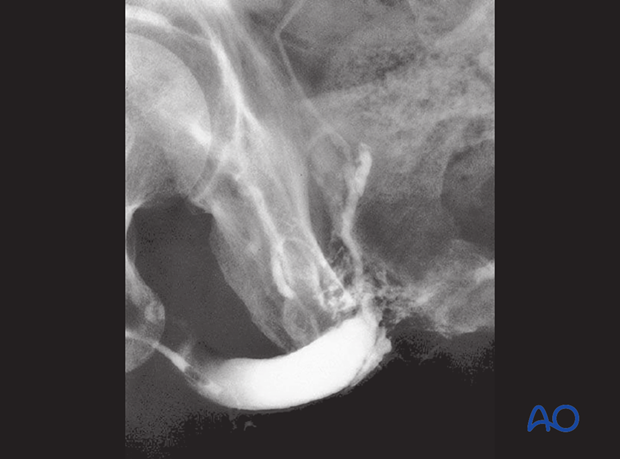
Urethral bleeding is a sign of a rupture of a urethra, mainly seen in men.
This should be identified before the insertion of a urethral catheter. Such bleeding suggests a disruption of the urethra. This must be assessed with a retrograde urethrogram.

Rectal examination must include assessment of prostate position. Cranial displacement of the prostate is another sign of urethral rupture.
Disruption of the anal sphincter or rectum should lead to consideration of a diverting colostomy.
Vaginal examination (speculum and digital) are necessary to look for open wounds, and/or displaced fractures.
Assessment of pelvic ring stability, after examination and initial AP X-ray
Occasionally a pelvic binder will reduce an open book type pelvic injury, so that the initial AP X-ray appears normal. If the pelvis is tender and the only X-ray was done with a binder in place, reassessment of pelvic stability is recommended.
Pelvic ring instability is strongly suggested by tenderness and abnormal mobility to manual examination, or abnormalities on an AP pelvis X-ray. If either is present, additional assessment is required (inlet outlet X-rays and/or CT scan).
If no sign of pelvic injury is evident on examination and initial X-ray, it may be appropriate to remove the pelvic binder at the end of resuscitation. If there is any reason to suspect that the pelvis is in fact unstable, additional imaging studies are necessary.
Examination of the pelvis
Ask the patient whether pain is present in the pelvic region. Palpate for tenderness of the pubis, iliac wings, and posterior pelvis. The latter is best assessed when the patient is logrolled.
Manual examination, with pelvic compression or external rotation of the iliac crests, is required to identify tenderness and/or bony instability.
If instable pelvic injuries are obviously present, no manipulation is advisable as it is painful and may increase bleeding.

3. Imaging
In all patients sustaining a high energy injury, imaging of the axial skeleton is an important adjunct. Either X-rays and/or CT scans will be need for the thoracolumbar spine. For the head and cervical spine, a CT scan is more reliable.
Focused Assessment Sonography in Trauma (FAST) is part of the imaging of all blunt trauma patients, to rule out intra-abdominal fluid. FAST is not used to diagnose specific organ injuries.
When free fluid is identified on FAST, CT scan with contrast can provide a precise diagnosis and is indicated unless immediate surgery is necessary.
When extremity fractures are suspected, focused X-rays are made in two directions (AP and lateral) to assess bone and joint.
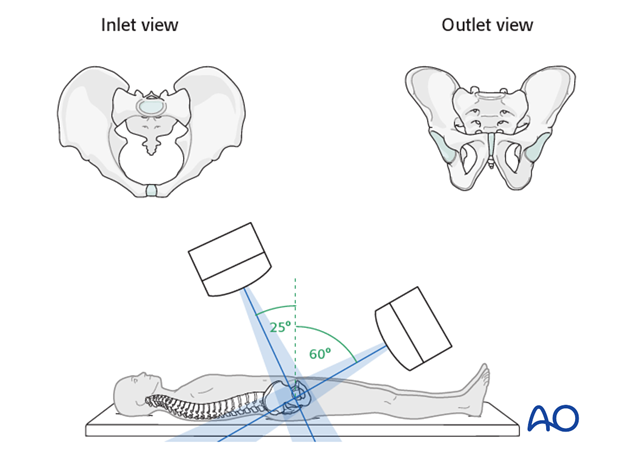
Pelvic ring injuries require either a CT scan with appropriate reconstructions and/or inlet and outlet views, and possibly internal and external oblique views.
Current data suggest that optimal angulation for an inlet view is 25° caudal tilt, and 60° cranial tilt for the outlet view.
In general, a CT scan of the pelvis is the next step to identify fracture type and position of fracture fragments.
This CT scan shows an external rotation (type B) injury of the right SI joint. The approximation of ilium to sacrum posteriorly suggests that the posterior sacroiliac ligament remains intact and that the joint is incompletely disrupted.
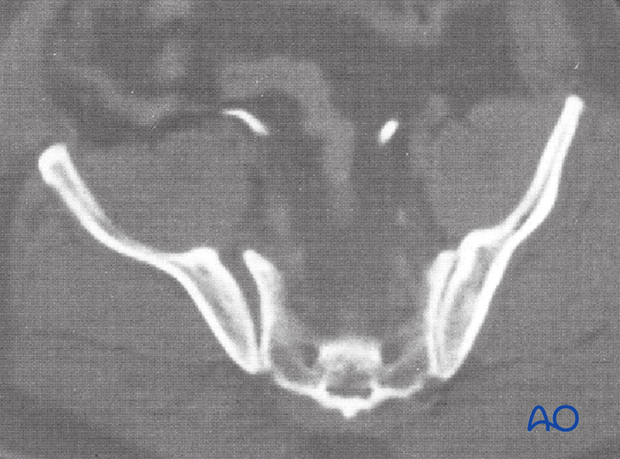
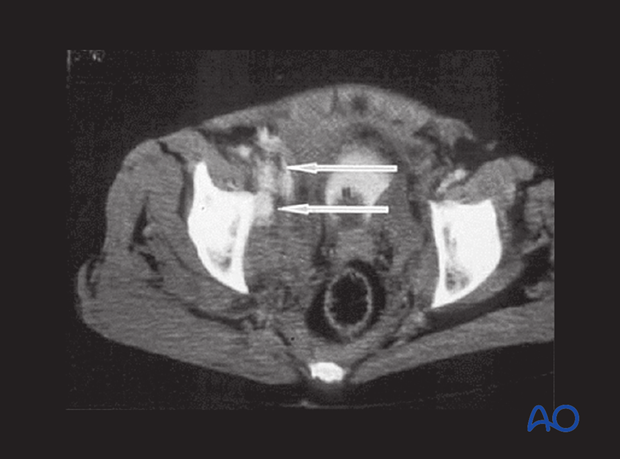
This CT scan shows a total disruption (type C) of the left SI joint. The joint is significantly widened from anterior through posterior portions, indicating that both anterior and posterior sacroiliac ligaments are disrupted.

Arterial bleeding, indicated by extravasated contrast material ("blush"). This usually indicates significant arterial blood loss and helps to identify bleeding for which with angio embolization is appropriate,
4. Additional action points
A urethral catheter is placed in all polytraumatized patients to judge fluid management.
Urethral tears may be incomplete, and placement of a catheter can cause additional damage. If a torn urethra is suspected, (meatal blood or high prostate on rectal examination, or difficulty passing the catheter), a retrograde urethrogram is indicated. This retrogram urethrogram shows contrast leaking into the surrounding tissues.