MIO - Iliosacral screw navigation
1. Introduction
Note: This description focuses on the use of navigation to guide IS fixation. For detailed considerations of IS screw insertion, (safe channels, reduction etc.), please refer to the descriptions of the conventional IS screw techniques.
In most hospitals real time information regarding the exact position of instruments within bone and soft tissues is achieved using image intensifier fluoroscopy. This technique requires significant radiation exposure and is time consuming.
The aim of intraoperative navigation is to achieve the same while minimizing the radiation exposure.
Intraoperative navigation as presented in this text provides information on screw entry point and trajectory relative to the sacrum. It does not provide information about pelvic alignment and reduction.
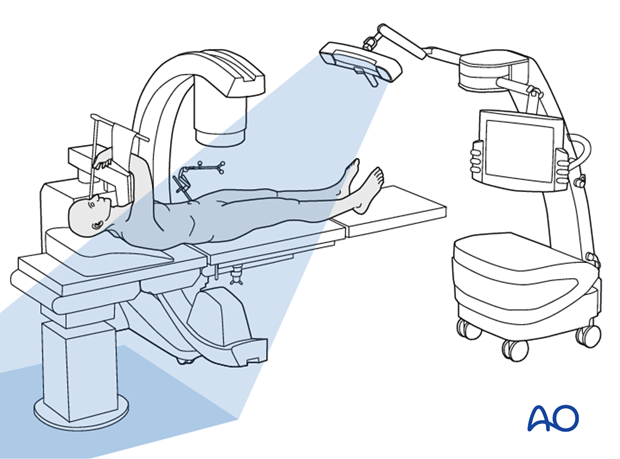
System components
The navigation system consists of the following three components.
- Computer unit with monitor
- Infrared camera (tracking unit)
- Infrared-emitting trackers attached to the surgical site, surgical instruments and the C-arm
For accurate navigation, it is essential that the trackers are rigidly fixed to the instrument or bone segment being tracked.
Registration
By attaching trackers to the C-arm and the iliac crest, their relative spatial position can be triangulated with the tracking camera.
This triangulation permits images to be recorded (inlet, outlet, lateral, and AP view) in the computer unit together with the exact location of the imaged structures in space.
Trackers attached to the drill sleeve allow the infrared camera to continuously feed the computer unit with its exact location and orientation in space.
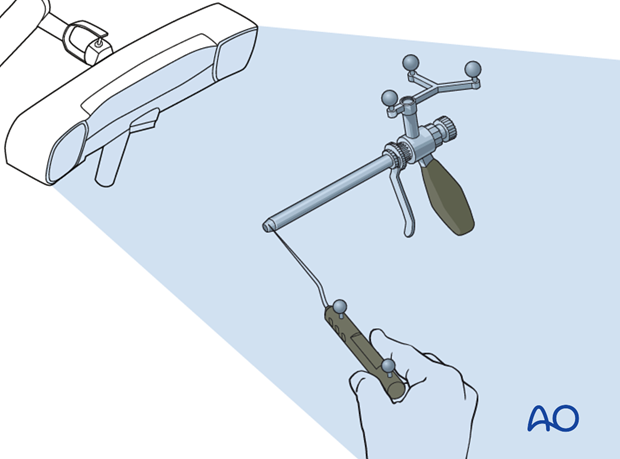
Tracking
The computer unit integrates the virtual image of the tracked instrument into the on screen X-ray.
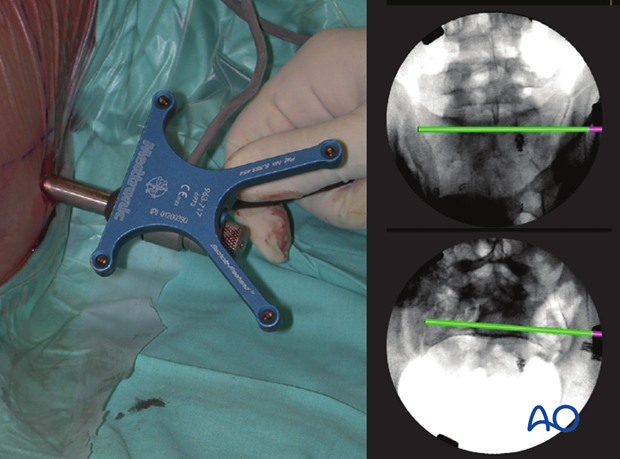
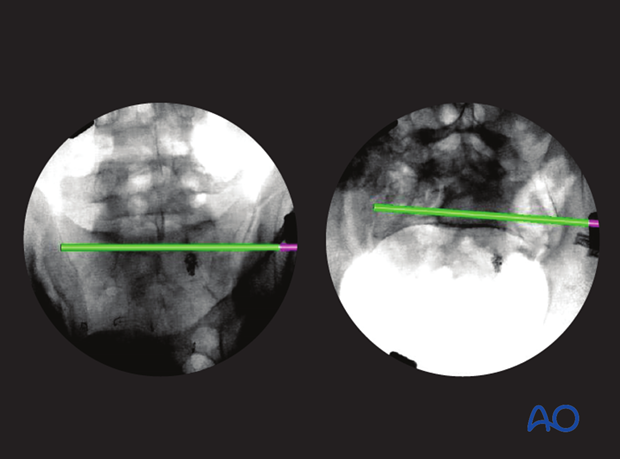
As the tracked components (pelvic ring and drill sleeve) move relative to each other (left), the computer unit will display on screen (right) how the drill sleeve (pink) and trajectory (green) move relative to the patients anatomy on X-rays in all views simultaneously (here only two views are show).
Validation
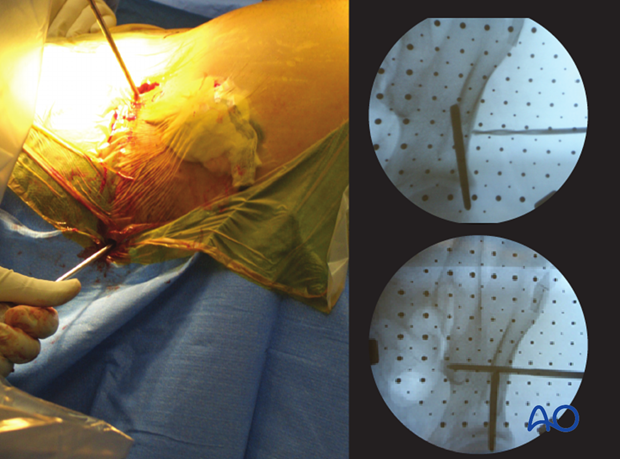
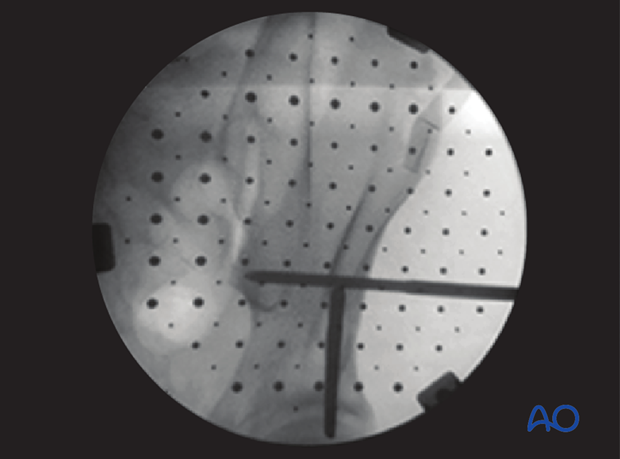
At regular intervals throughout the procedures a C-arm image is acquired to verify that the location of the actual guide correlates to the virtual guide wire.
2. Reduction
When intraoperative computerized navigation is used, it is essential to the accuracy of the procedure that the reduced segments of the pelvic ring do not move relative to each other during the procedure. Any movement will lead to inaccurate orientation of instrumentation.
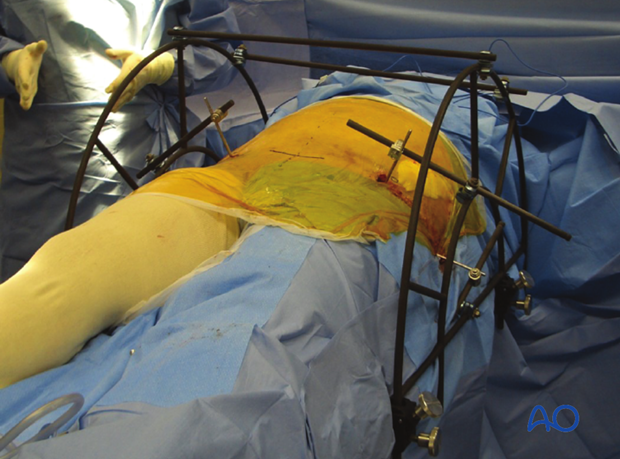
To achieve this, a table mounted skeletal pelvic fixation frame can be used. This combines external fixators with reduction possibilities in all 3 dimensions.
Such a frame will not be required for a minimally displaced stable SI disruption.
For open book (external rotation) fractures, it is advisable to fix both feet together in internal rotation, which usually produces a significant improvement of external rotation deformity, at least for type B injuries.
If acceptable reduction cannot be achieved by a closed technique, an open reduction technique should be performed.
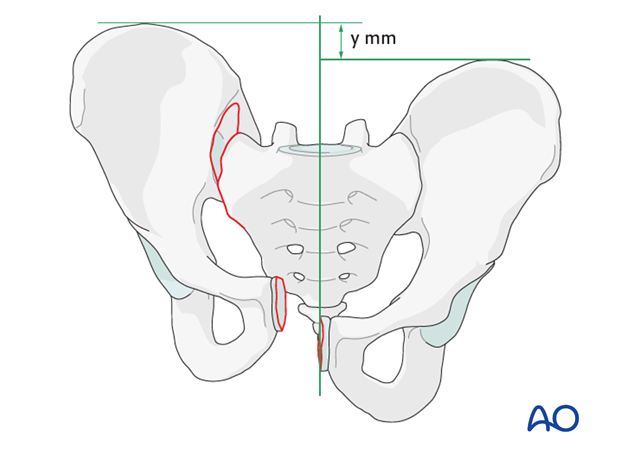
Correction of internal and external rotation
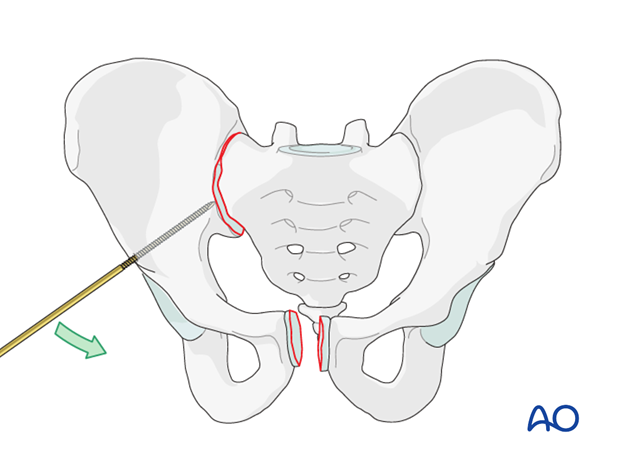
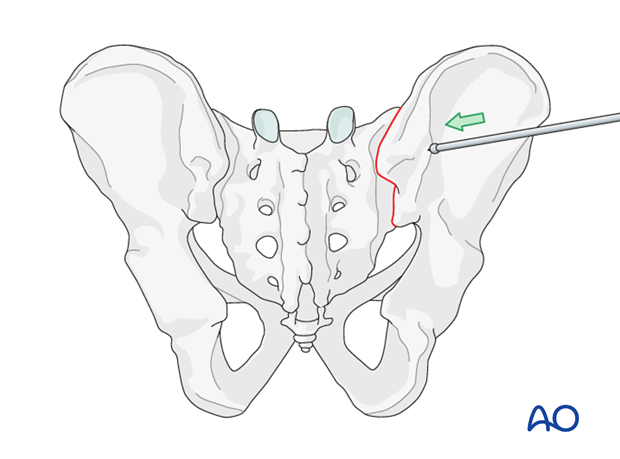
For internal and external rotation of the hemi pelvis, Schanz screws can be inserted in the supra acetabular area and/or ala. These are then used as joy sticks until reduction is achieved. The Schanz pins are held in place either manually or by attachment to an external frame (as an external fixator) until fixation is completed.
Correction of minor lateral displacement
If only a compression of the joint is necessary, a ball spike can be used through a separate incision to reduce the SI joint.
If acceptable reduction cannot be achieved by a closed technique, an open reduction should be performed.
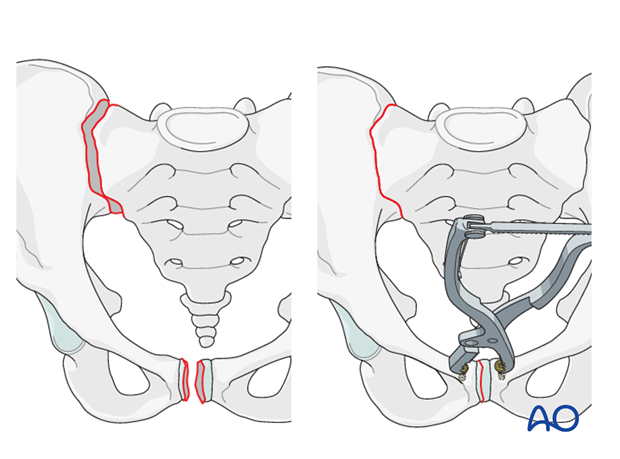
Correction of SI dislocation with associated disruption of the symphysis
If SI dislocation is associated with disruption of the symphysis, open reduction with temporary fixation of the symphysis is performed first.
This will partially reduce the SI joint.
If only a small widening of the SI joint remains in AP view with no vertical or horizontal displacement (inlet and outlet view in good position),then the iliosacral screw will compress the joint and complete the reduction.
Correction of vertical displacement
Correction of vertical displacement may be challenging to achieve.
In cases of vertical displacement where the contralateral hemipelvis is intact, the patient can be placed on a radiolucent traction table. Traction is applied until correct reduction can be seen on AP outlet and inlet projections. The traction is then maintained until fixation is completed.
Temporary fixation
When reduction is completed, it needs to be secured to ensure accuracy of the computerized navigation.
3. Insertion of SI screw using navigation
Registration
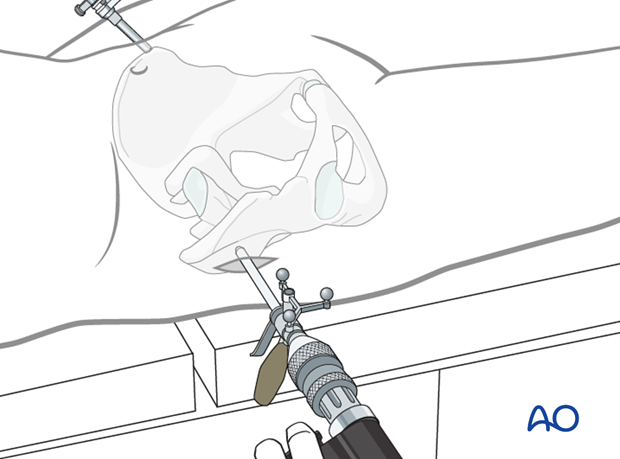
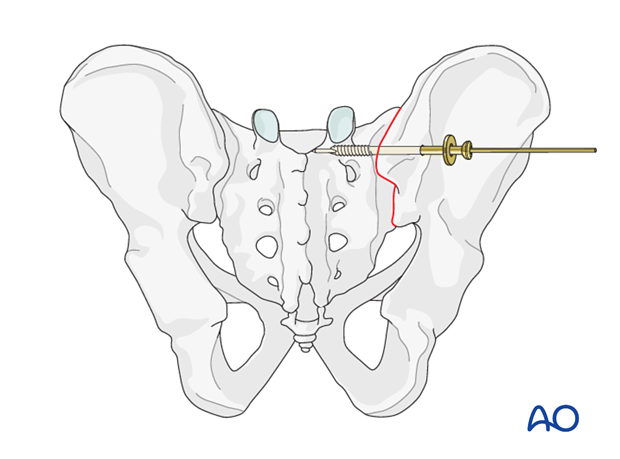
The reference frame is attached to the iliac crest and the pelvic ring is registered in inlet, outlet, lateral, and AP view with the registered C-arm.
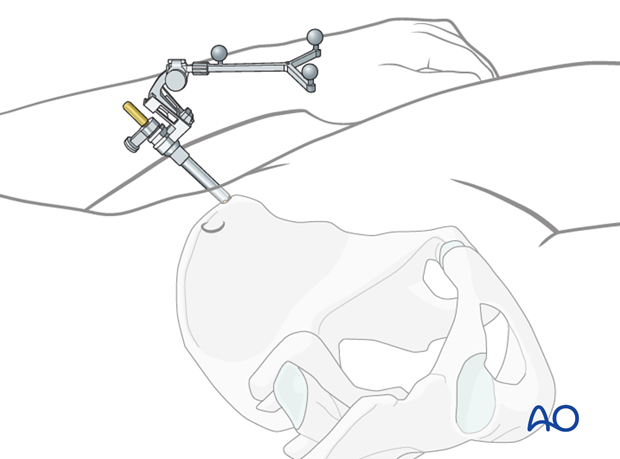
The drill sleeve is registered and will be tracked throughout the procedure.
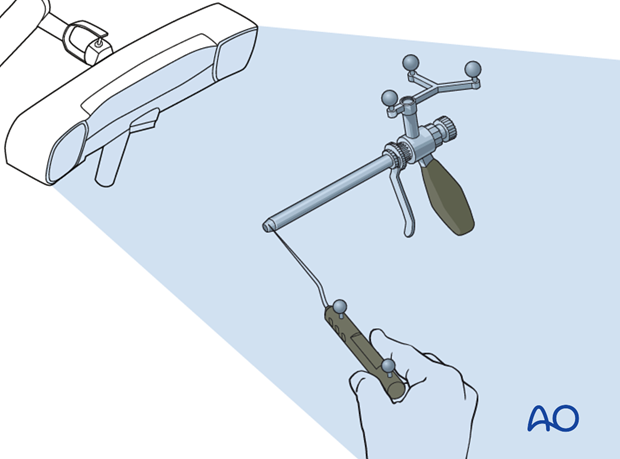
Correct patient registration is confirmed by placing a registered pointer onto an anatomical landmark of the pelvic ring. If the virtual pointer is not pointing to the corresponding landmark in the on-screen X-ray, the registration is incorrect and will need to be repeated.
Landmarks for stab incision
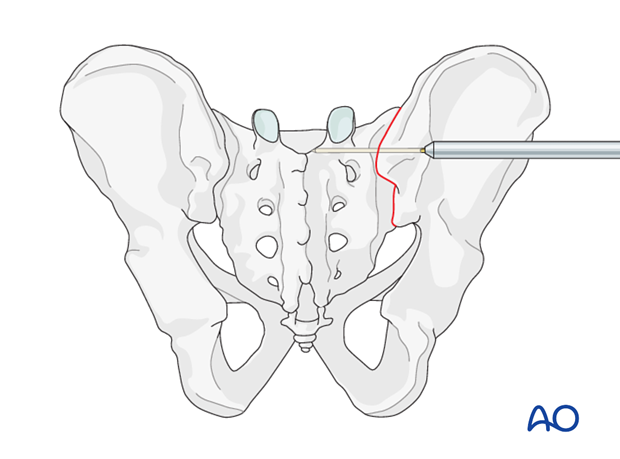
The virtual trajectory line originating from the tracked drill sleeve is used to determine the location of the stab incision.
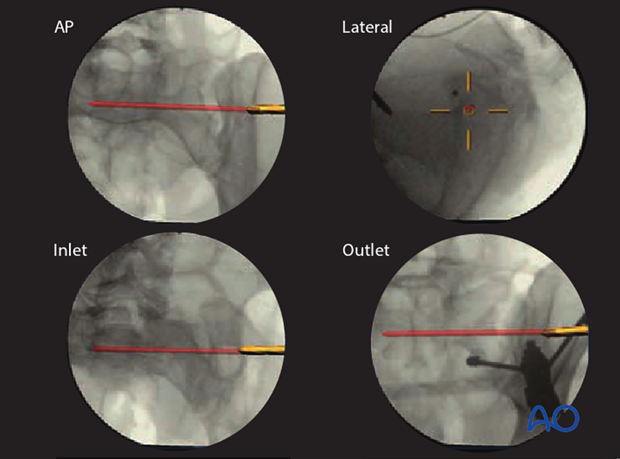
After the stab incision is made, the drill sleeve is inserted down to the ilium.
The position of the drill sleeve (pink) is adjusted until the virtual beam (green), which represents the guidewire, has an optimal entry point on the ilium and direction into the sacral vertebra (S1 or S2).
A safe zone for the screw insertion should be available.
The correct screw length and width can now be determined based on the virtual trajectory. The screw should reach well into the sacral vertebral body.
The guide wire is now inserted through the drill sleeve.
Validation
A C-arm image is recorded to validate that the virtual guide wire trajectory correlates to the actual guide wire direction.
If the validation fails, the equipment should be checked and the procedure restarted with new registration.
The screw is then inserted over the guide wire and the guide wire removed.
4. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













