Circulation
1. Note!
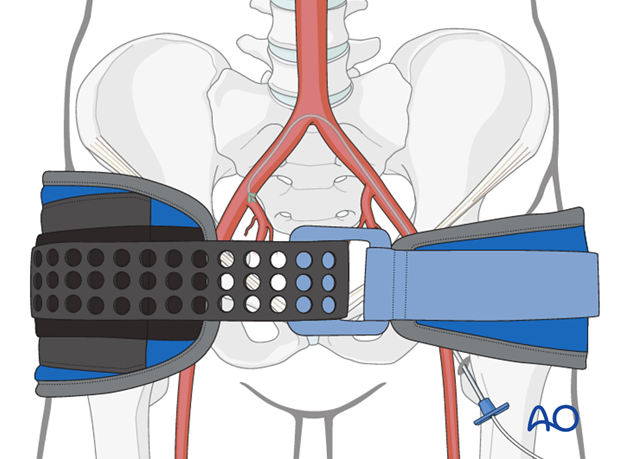
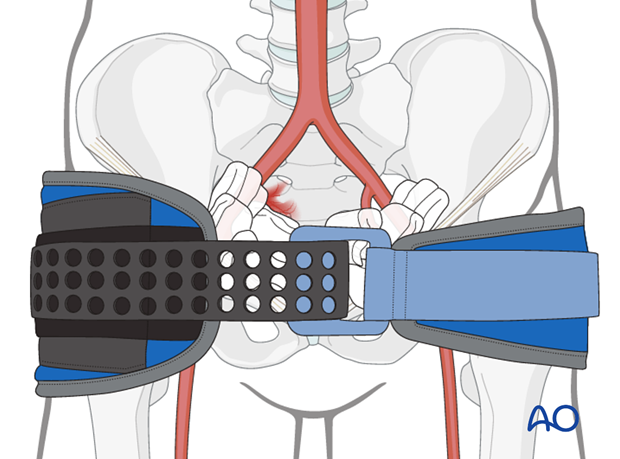
A pelvic binder should be applied for any blunt trauma patient.
Hypothermia should be prevented at all time during the assessment process.
2. Are there signs of inadequate circulation?
Circulation is inadequate if:
- The skin is cool, clammy, pale
- Presence of tachycardia
- Presence of tachypnea
- Disabled mental status
Hypotension is a sign of severe shock (Class III blood loss>1500cc).
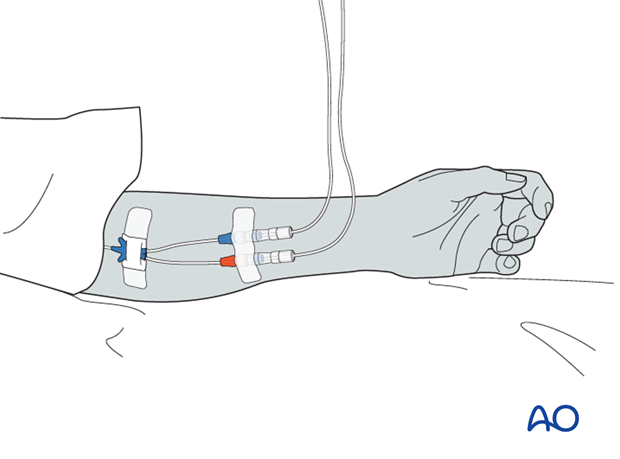
When circulation is inadequate, IV lines are inserted and appropriate IV fluid therapy is initiated.
The patient is re-examined for A and B again, and then the neurological state of the patient is examined.
3. Further actions if circulation is not adequate
Always check pelvis for signs of injury - tenderness and/or instability. If there is any reason to suspect an unstable pelvic injury, add a pelvic binder if not already present.
If circulation is inadequate, administer IV fluids, but rule out nonhemorrhagic shock:
- Tension pneumothorax
- Cardiac tamponade
- Cardiogenic shock
- Neurogenic shock
- Septic shock
Remember - more than one cause of shock may be present

If tension pneumothorax and cardiac tamponade can be ruled out, the cause is probably hypovolemic shock.
Look for sites of bleeding:
- Chest
- Abdomen
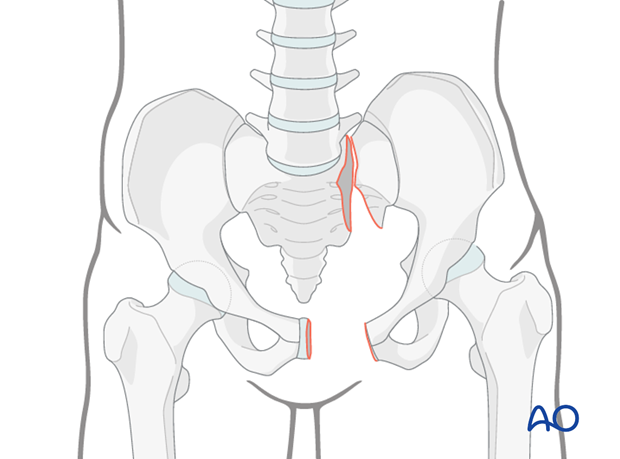
- Pelvis
- Proximal Extremities
- External bleeding
External bleeding
Stop external bleedings using pressure bandages or tourniquets.
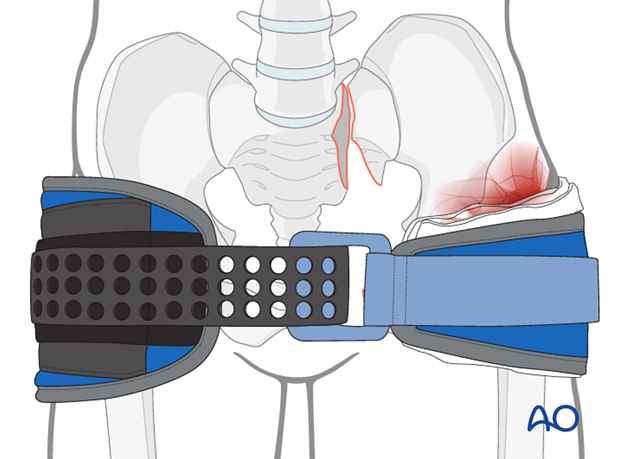
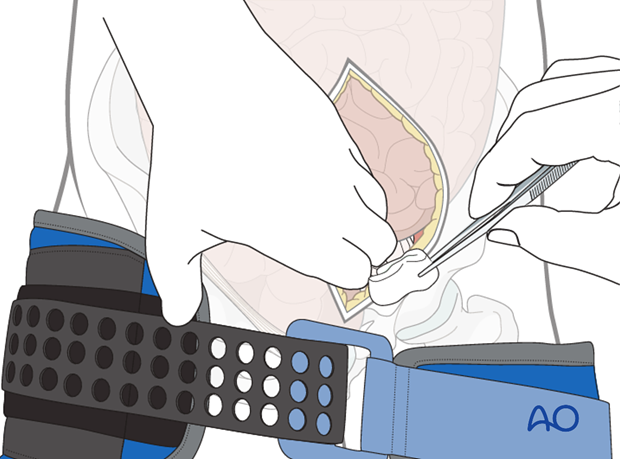
For open pelvic fractures, management should focus on reduction of the pelvic ring using a temporary pelvic binder plus packing of the perineal wound.
If treatment is successful and the bleeding has stopped, patient is re-examined for A and B again, and then the neurological state of the patient is examined.

Internal bleeding
Identify other potential sources of internal bleeding in trauma patients, even with an evident pelvic fracture.
In patients with a fracture of the pelvis, the source of bleeding may be the pelvic area itself and/or the abdomen, thorax, or even in areas with closed fractures (eg femur shaft).
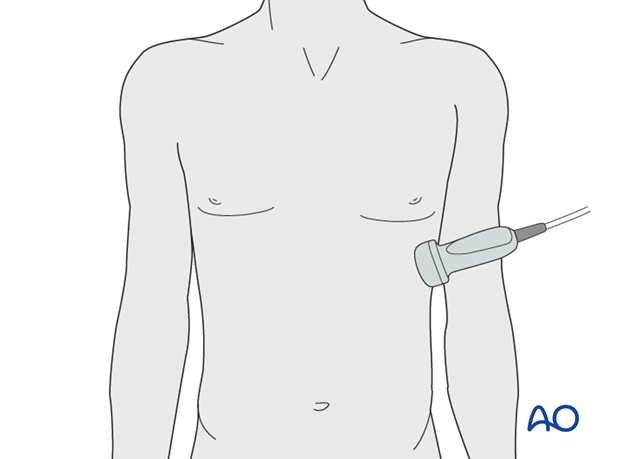
The abdomen is examined using ultrasound (FAST) to identify free fluid in the intraperitoneal space.
If the patient is not in need of immediate surgery and free fluid is found in the abdomen, a CT scan with contrast should be performed to identify the cause of the fluid.
If the patient is in need of immediate surgery for control of hemorrhage, laparotomy with damage control packing is performed.
If the pelvis is unstable, ensure that the pelvic ring is stabilized during surgery.
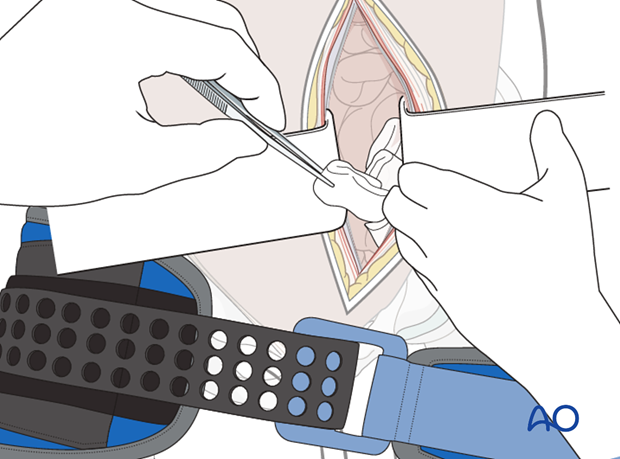
During the laparotomy, it may also be necessary to perform extraperitoneal pelvic packing to stop bleeding in that region (described below).
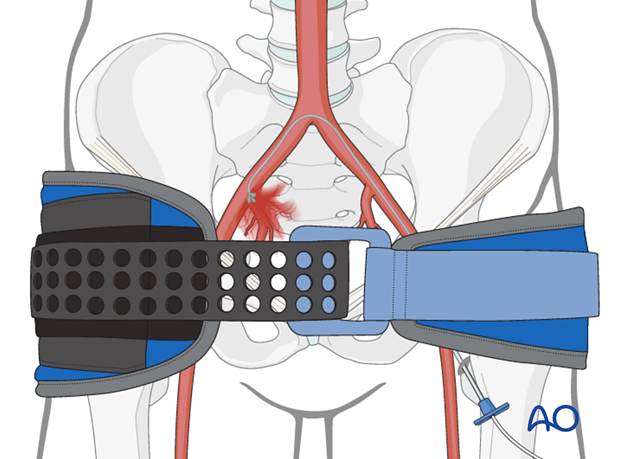
Another source of massive blood loss could be the pelvic area in patients with unstable pelvic fractures.
Clinical signs are: instability, bleeding wound, ecchymosis, or obvious deformity.
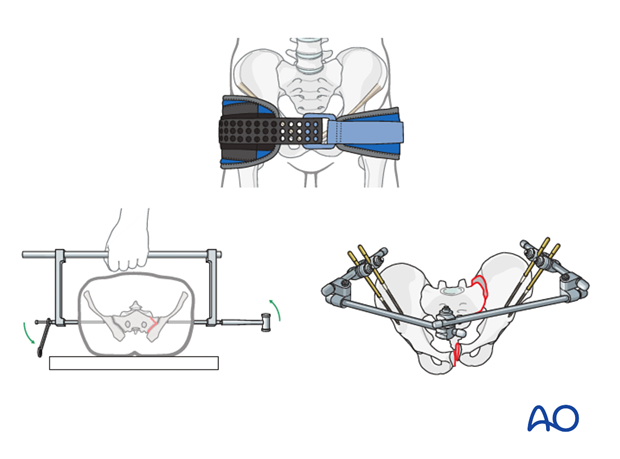
Pelvic instability is assessed by physical examination, compressing the iliac crest bilaterally towards the midline. If either side gives way to this pressure, if it produces pain, pelvic instability is likely to be present.
If instable pelvic injuries are obviously present, no manipulation is advisable as it is painful and may increase bleeding.

Ecchymosis in the perineal area /scrotum/pubis
Reduced bleeding after reduction of open book deformity by internal rotation of the legs, or the use of a pelvic binder, is an indirect sign of pelvic bleeding.
Hypotension associated with a pelvic ring injury raises the question of whether the source of bleeding is from the pelvic vessels or elsewhere (eg. abdominal cavity). In some patients, both sources may be present.

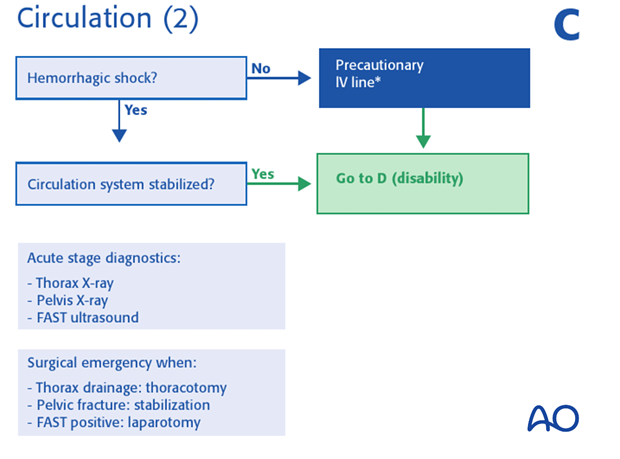
4. Evident shock with a pelvic ring injury
As for any patient with hemorrhagic shock, the following guidelines should be followed.
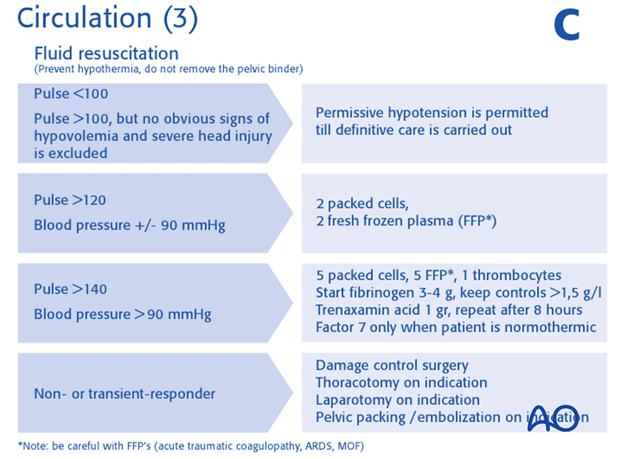
IV fluid replacement
Insert two large bore IV lines and start fluid management based on blood loss and response on therapy. Traditionally this begins with rapid infusion of 2L of warm balanced salt solution.
Further fluid replacement is based on the 1:1:1 rule. (1 fresh frozen plasma : 1 packed cells : 1 concentrated platelets).
In the absence of severe head injury, permissive hypotension can be accepted.
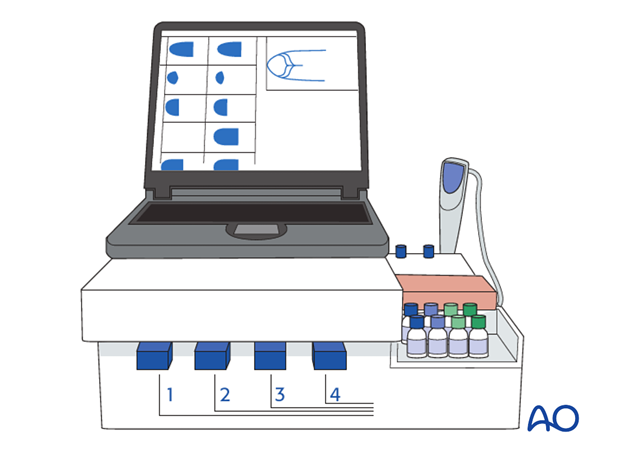
Early treatment of coagulation problems is indicated. This might be done preemptively without laboratory confirmation. Based on the clot elastogram, corrective medication can be administered (eg. fibrinogen, tranexamic acid, or cofactors).
When the patient is normothermic, factor 7a can be used if necessary.
Further actions depend on response to IV therapy
Further actions will depend on the physiological response of the patient.
If the patient fails to respond urgent action will be necessary.
If the patient responds to fluid replacement, there may be time for further diagnostic maneuvers before further treatment. Continued monitoring of the patient is necessary to avoid missing hemodynamic deterioration.
Urgent action if the patient fails to respond is:
- Mechanical stabilization is essential in all cases. The first option is a correctly applied pelvic binder (which should already be in place). C-clamp or an external fixator may provide better stability in some cases.
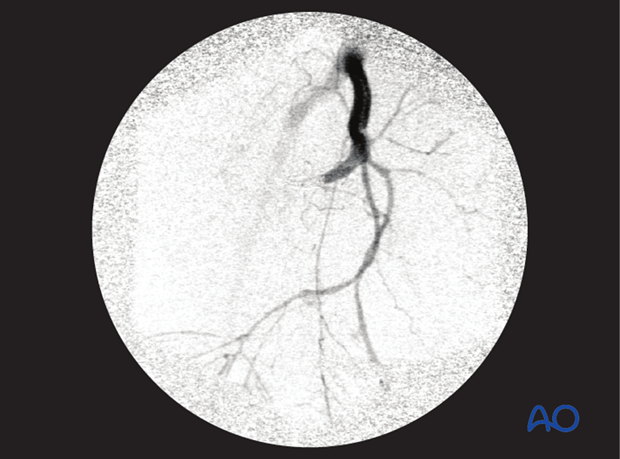
- If the patient remains unstable after mechanical stabilization, pelvic packing and/or angio-embolization should be added.
- If the patient is in extremis (unobtainable BP) immediate surgical packing is essential.
Failed embolization
If hemorrhage continues after angio embolization, this procedure may be repeated, or pelvic packing should be performed. In either case the pelvic binder remains in place continuously until alternative mechanical stabilization is provided.
Failed packing
If there is ongoing hemorrhage after mechanical stabilization and packing, angio embolization is performed if available.
If treatment is successful and the bleeding has stopped, patient is re-examined for A and B again, and then the neurological state of the patient is examined.