Anterior ORIF SI Joint
1. Introduction
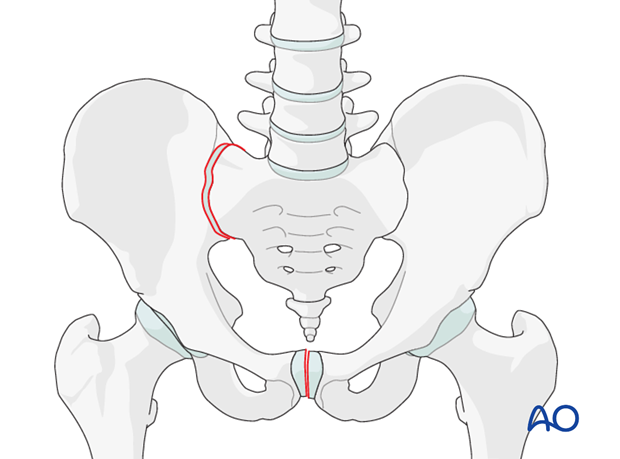
Sacroiliac joint instability, with or without associated fracture, is the most common cause of posterior instability of Type-C pelvic ring injuries.
Instability of the sacroiliac joint occurs most commonly with a pure disruption of the sacroiliac joint.
Most pure sacroiliac joint dislocations may be treated with closed reduction and percutaneous iliosacral screw placement. Therefore, open reduction and anterior plating should be reserved for only select cases, primarily when closed reduction is not possible, or when an anterior approach to the innominate bone is required for another injury.
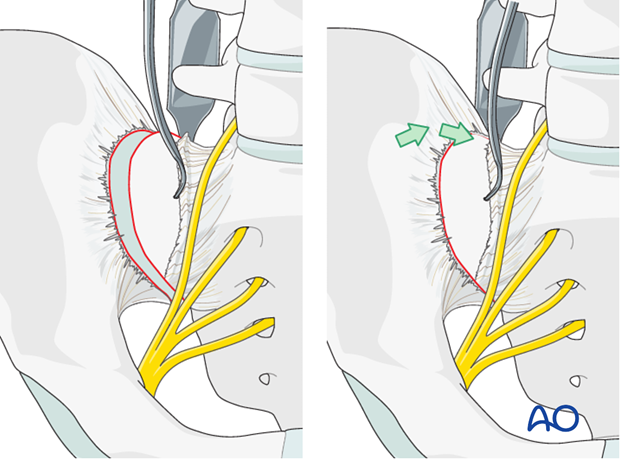
2. Preparation of the sacroiliac joint
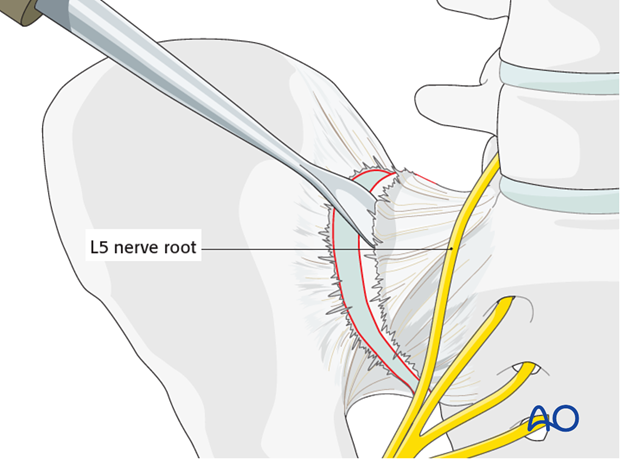
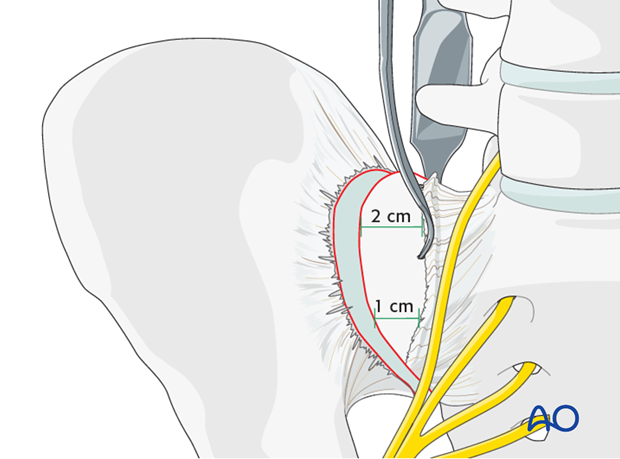
Use a Cobb elevator to elevate the anterior fibers of the sacroiliac ligament from the sacrum. Further medial dissection must respect the L5 nerve root but can be extended 1-2 cm and should be subperiosteal.
Prepare sacral ala for screw insertion
Insert sharp Hohmann retractors posteriorly and anteriorly into the sacrum to expose approximately 1–2 cm of the lateral section of the sacrum for later screw positioning.
The pointed tips of these retractors may be gently impacted into the bone of the sacral ala.
Inspect and debride the sacroiliac joint
The SI joint is distracted using a laminar spreader. The joint is inspected, irrigated, and small fragments are removed.
3. Reduction
Manual reduction with pressure on the ilium
It may be possible to reduce the sacroiliac joint by pushing the lateral surface of the iliac wing medially toward the sacrum.
Reduction using Schanz screw
A Schanz screw may be inserted into the iliac crest or the supraacetabular region in order to aid reduction of the SI joint.
The Schanz screw may be used as a joy stick to allow manipulation of the iliac wing. This is particularly useful if there is a rotational displacement at the SI joint.
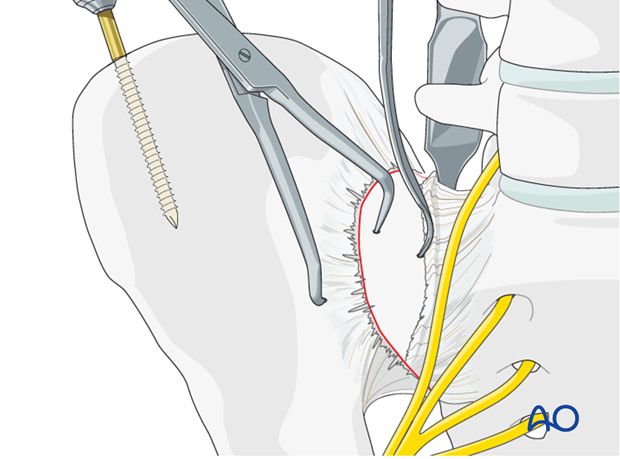
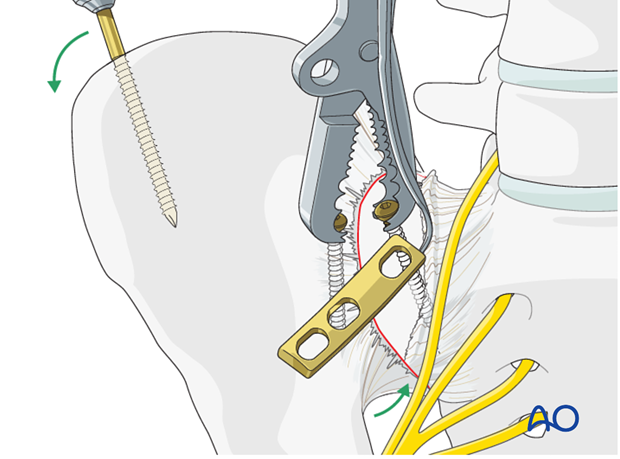
Reduction using a pointed reduction clamp
A pointed reduction clamp may be applied as an adjunct across the SI joint in order to achieve reduction. Alternatively, the clamp may be applied to maintain a reduction achieved by other means.
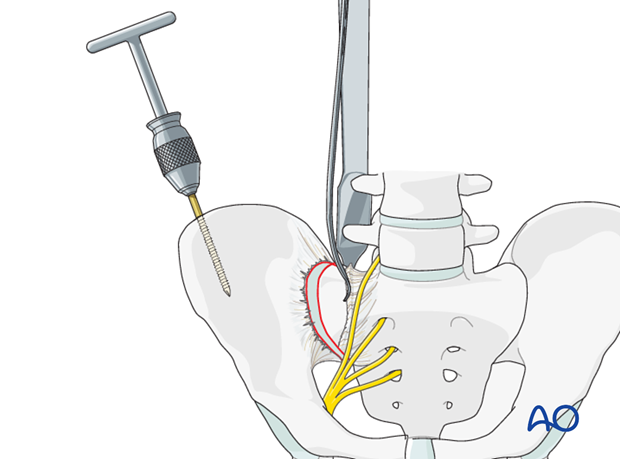
Reduction using a Farabeuf or Jungbluth clamp
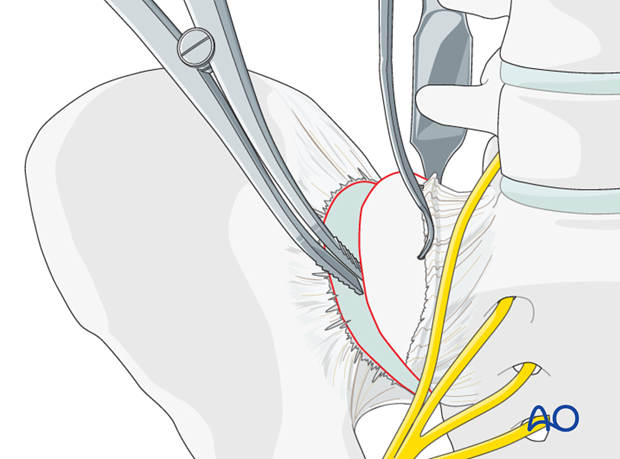
In order to apply the Farabeuf or Jungbluth clamp a screw is placed into the sacral ala. First, the drill hole is made. The drill is placed parallel to the SI joint under direct vision.
These screws are usually 50–60 mm in length.
There is a limited area (approximately 1–2 cm medial to the SI joint) that allows for safe placement of screws in the sacral ala, due to the proximity of the L5 nerve root.
Insert a screw into the sacral ala using the previously drilled hole. A second hole is drilled in the ilium just lateral to the sacroiliac joint. Insert a second screw into this hole.
These screws should be placed in the central portion of the sacroiliac joint (from anterior to posterior) in order to leave room for the plates to be applied, both anteriorly and posteriorly to the reduction screws.
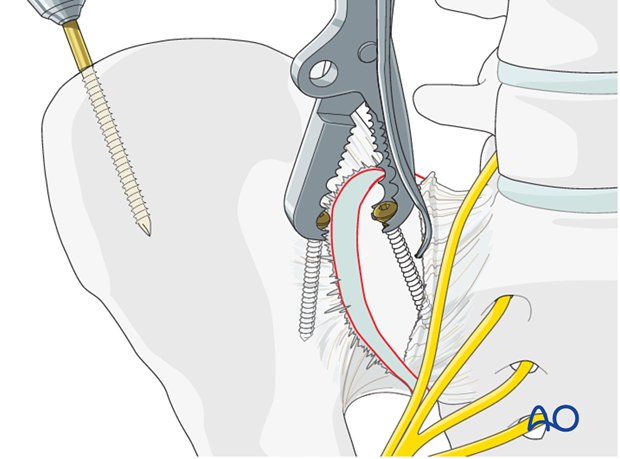
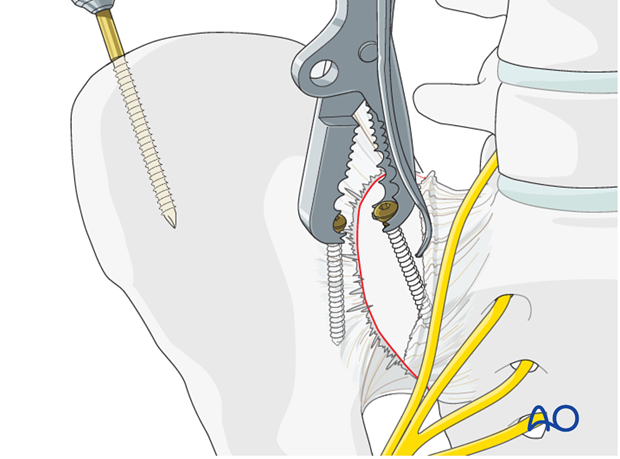
Next, apply a Farabeuf or Jungbluth clamp to these screws. The clamp can then be used to reduce the sacroiliac joint. The clamp allows for reduction in multiple planes.
Anatomic reduction should be confirmed by direct visualization and verified by image intensification.
Temporary iliosacral fixation with a K-wire is possible
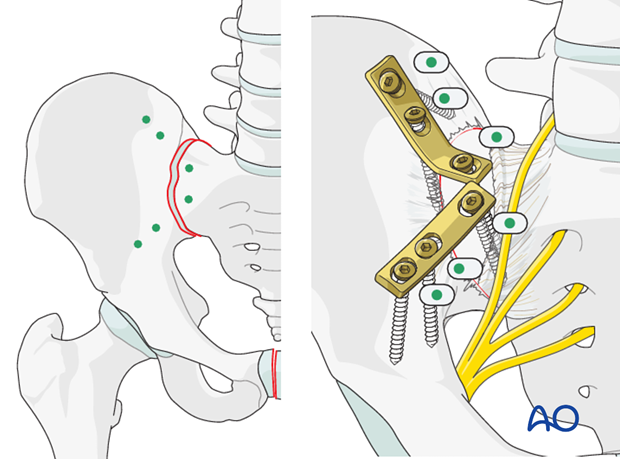
Planning for plate fixation
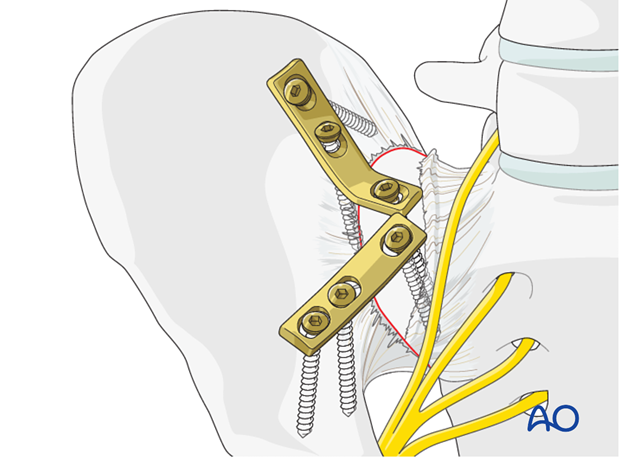
Two dynamic compression plates are necessary for control of rotation at the sacroiliac joint.
As shown in the illustration, the plates should be positioned across the SI joint.
Place them under compression using the dynamic compression holes.
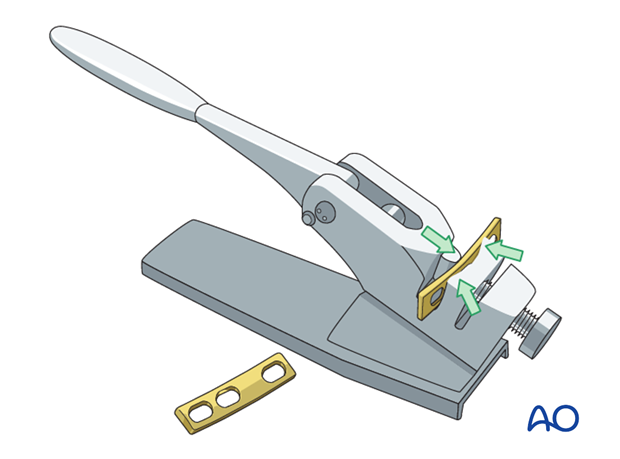
Pre-contouring of the plates
The plates are contoured using a table top bending press. The plates are contoured to fit across the SI joint with one screw in the sacrum and two in the ilium.
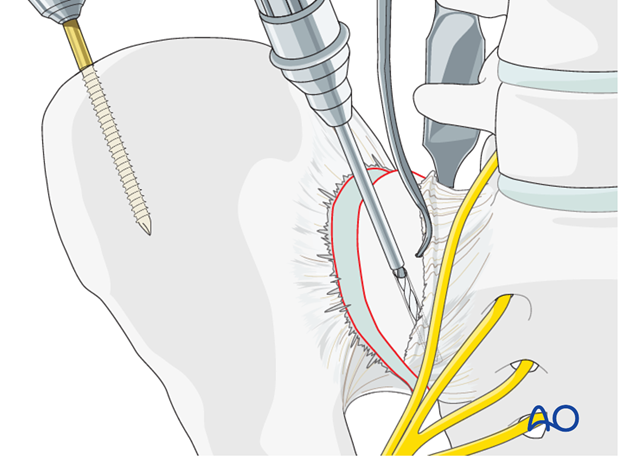
4. Plate application
Apply the stabilizing plate
After reduction has been achieved, the plates are applied across the SI joint. If a Jungbluth or Farabeuf clamp has been used, one plate is applied anteriorly to the clamp.
If there is sufficient space, the second plate may be applied posterior to the clamp. Otherwise, once the first plate has been applied, the clamp may be removed to make room for the second plate.
Insertion of screws
Drill the sacral hole in a carefully selected site without the plate in place. The densest bone of the ilium is within the first 3 cm lateral to the sacroiliac joint.
After securing the plate to the sacrum the first iliac screw is placed eccentrically for compression.
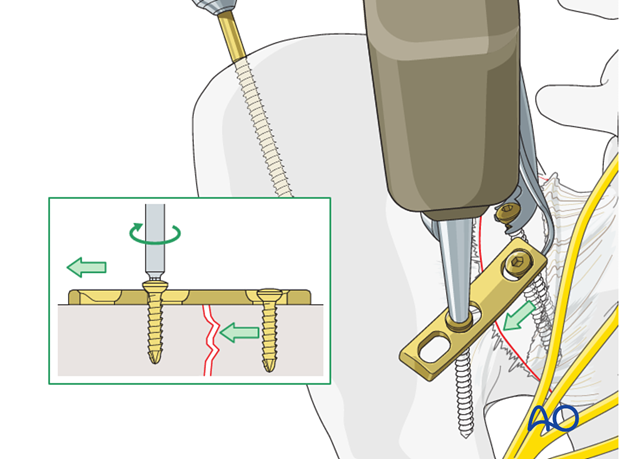
The most lateral screw is inserted in neutral position.
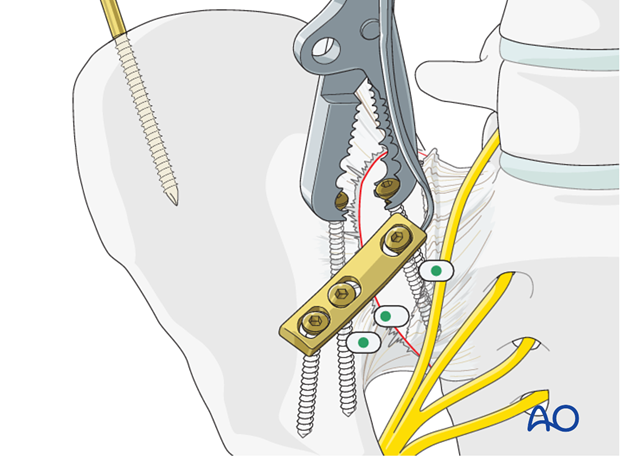
Placement of the second plate
Two plates are needed. Remove any clamps and insert the second plate in the same manner.
5. Postoperative x-ray control
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.














