Patient examination
1. General considerations
Patellar fractures are some of the most difficult fractures to treat. The surgeon will often underestimate the complexity of the injury and will therefore not be prepared for a very challenging osteosynthesis.
The articular injury is usually much more severe than predicted from the radiographs. In addition, multiple small articular fragments may be difficult to bring together. Patellar fractures are important for two reasons:
- they generally disrupt the extensor mechanism and
- they are associated with a significant articular injury to the patellofemoral joint
Patellar fractures comprise about 1% of all fractures and are mostly caused by direct trauma to the front of the knee, for example, a direct fall, or a blow onto the flexed knee.
Bony avulsions of the adjacent tendons, or pure ruptures of the quadriceps and patellar tendons, are caused by indirect forces.

2. Clinical examination
Careful examination of the whole extensor mechanism starting with the quadriceps, quadriceps tendon, patella, patellar tendon, and insertion into the tibial tuberosity is necessary.
An injury to the extensor mechanism may have any one of these anatomic components injured and necessitates the careful exam.
Typical signs are swelling, tenderness and limited, or loss of function of the extensor mechanism.
Preservation of active knee extension does not rule out a patellar fracture if the auxiliary extensors of the knee - the medial and lateral parapatellar retinacula - are intact.
If displacement is significant, it is possible to palpate a defect between the fragments, if present. The hemarthrosis is usually obvious.
The examination must include assessment of the soft tissues, so as not to confuse with an injury to the prepatellar bursa, or to omit grading the injury if the fracture is open.
Injury to the patella may disrupt the extensor apparatus of the knee and the patient may be unable to perform an active straight leg raise. Untreated, displaced patellar fractures may lead to marked difficulty with normal gait. If there is clinical uncertainly about the correct diagnosis of disruption of the extensor apparatus of the knee, an ultrasound scan, or MRI, of the extensor apparatus, including the quadriceps tendon and patellar tendon should be obtained, in order to elucidate the correct diagnosis.
As well because of the physical location of the knee, open fractures are very common and must be treated appropriately.
Because so many of these patellar injuries happen in car crashes with dashboard mechanisms, then ligamentous injuries must also be clinically ruled out.

3. Radiological examination
X-rays include AP and lateral, and skyline view. Obliques are occasionally useful but not necessary.
CT scans are not commonly made.
In general, the complexity of a patellar fracture may be underestimated by a cursory review of the injury radiographs.
Comminution and/or additional fracture lines may often be missed. Therefore, a scrutiny of good quality AP, lateral and axial radiographs can prepare the surgeon better for fixation of the fracture.
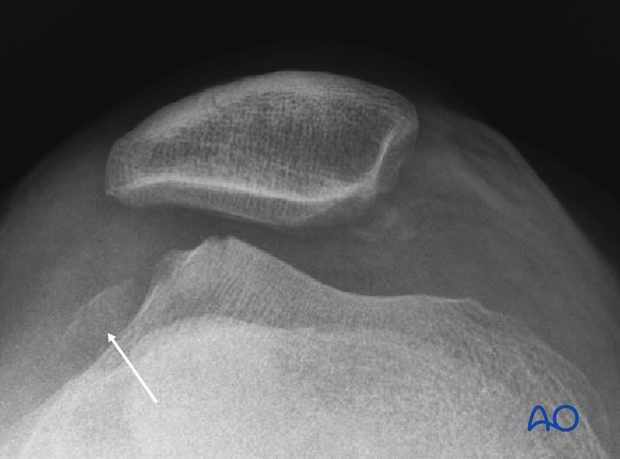
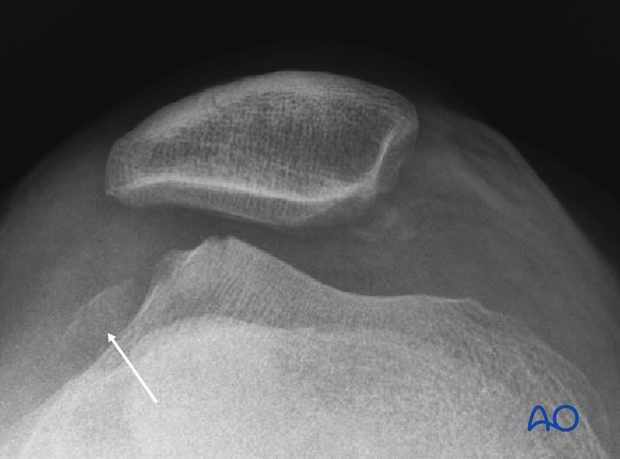
Occasionally, there are articular impaction, or osteochondral shear injuries, to the distal femur that are often irreparable. Knowledge of this preoperatively will allow an appropriate discussion with the patient of the expected clinical outcome.
If additional fracture lines are seen, preoperative planning will allow for additional instrumentation to be available. This may include small-fragment, or mini-fragment, screws.
This image shows (arrow) a displaced femoral condylar articular fragment and the accompanying defect in the condyle.
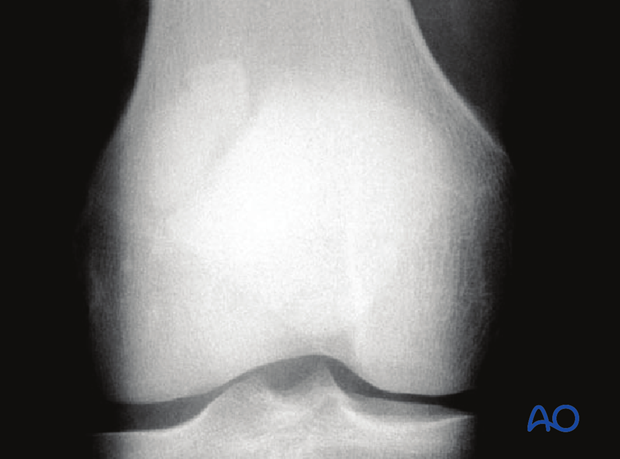
4. AP view
In the AP view, the patella normally projects into the midline of the femoral sulcus. Its lower pole is located just above a line drawn across the distal profile of the femoral condyles.
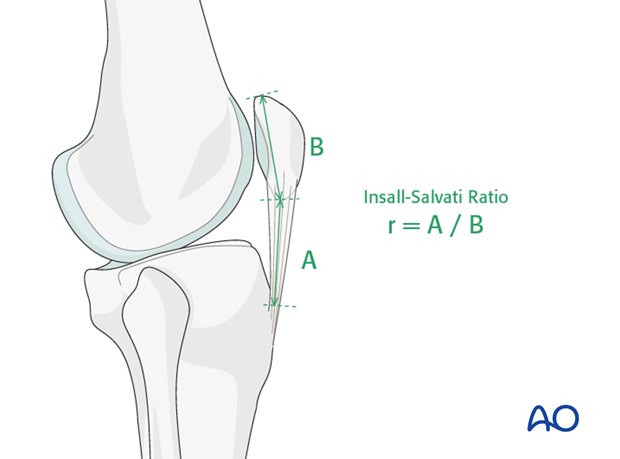
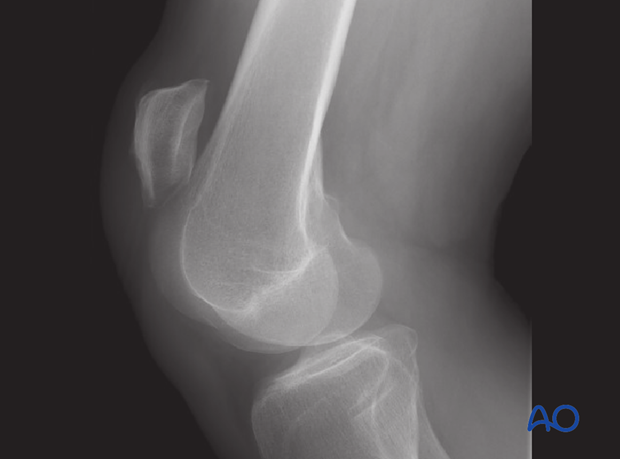
5. Lateral view
In the lateral view the proximal tibia must be visible to exclude a bone avulsion of the patellar tendon from the tibial tuberosity.
A rupture of the patellar tendon, or an abnormal position of the patella like patella alta (high-riding patella), or patella baja (shortening of the tendon), can be recognized with the help of the Insall-Salvati method. This is the relationship between the length of the patella (B) and of the patellar tendon (A) on the lateral x-ray, r = A/B. This ratio is normally r = 1+/-0.2, i.e. 0.8-1.2. A ratio r > 1.2 suggests a high-riding patella (patella alta), or patellar tendon rupture.
6. 30° tangential view (skyline view)
The third important x-ray projection is the 30° tangential view, which is obtainable in 45° knee flexion. If a longitudinal, or osteochondral fracture, is suspected, the 30° tangential view is a helpful diagnostic adjunct.

7. Other imaging techniques
Special imaging is helpful in certain cases, such as stress fractures, in elderly patients with osteopenia and hemarthrosis, and in cases of patellar nonunion, or malunion.
Computed tomography is recommended only for the evaluation of articular incongruity in cases of nonunion, malunion and patello-femoral alignment disorders.
Scintigraphic examination (or MRI) can be helpful in the diagnosis of stress fractures; a leukocyte scan can reveal signs of osteomyelitis.
MRI can be helpful to diagnose cartilage defects and lesions.
8. Isolated tendon ruptures
Isolated rupture of the quadriceps, or patellar, tendon must be excluded by clinical evaluation (palpation) and ultrasound scan (or MRI).
This lateral X-ray shows a ruptured patellar tendon.
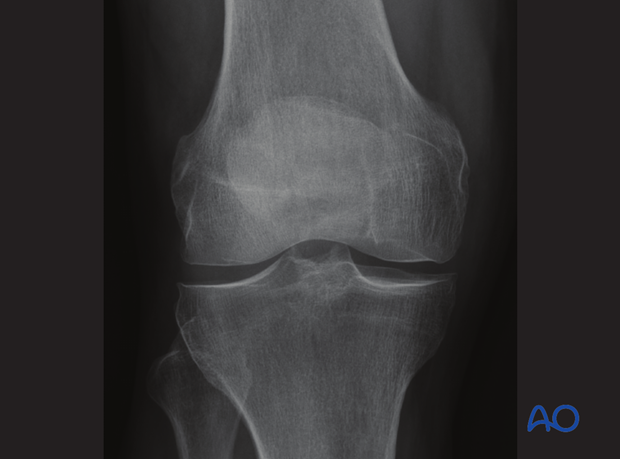
9. Patella dislocations
Dislocation, most commonly occurring to the lateral side, may result in osteochondral shear fractures with lesions of the medial margin of the patella, and occasionally impaction fractures of the lateral lip of the patellar groove of the femur.
X-ray by courtesy of Spital Davos, Switzerland, Dr C Ryf and Dr A Leumann.
10. Bipartite patella
Bipartite patella is an anatomical variant that results from developmental lack of assimilation of the bone during growth. Located on the proximal lateral quadrant of the patella, the condition is without clinical relevance, is usually bilateral and has a characteristic x-ray feature with rounded, sclerotic lines rather than the sharp edges of a fracture.