ORIF
1. Principles
Anatomical considerations
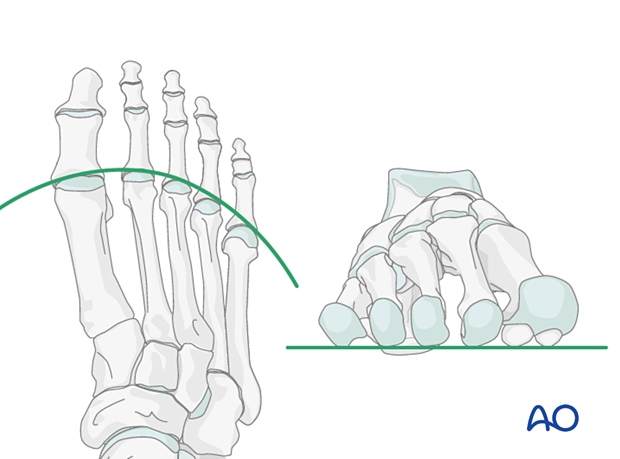
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Restoration of normal architecture can be challenging when multiple metatarsals are involved.
Timing of surgery
The timing of surgery is influenced by the soft-tissue injury and the patient's physiologic status.
Multiple fractures are associated with more soft-tissue compromise than isolated injuries. Swelling should decrease before open treatment.

Strategy
Anatomic reduction of the medial metatarsals (1–3) is prioritized. Due to the mobility of the 4th–5th cuboid articulation, more deformity of the 4th and 5th metatarsals is acceptable.
Anatomic reduction is more likely to be achieved with simple fractures. Thus, simple fractures of the 1st–3rd metatarsals are typically addressed first, starting with the 1st metatarsal. Often with accurate fixation of the medial rays, the lateral rays “fall” into acceptable position.
Anatomic reduction is more challenging for multifragmentary fractures. Contralateral foot x-rays can be a valuable template to judge alignment.
Below we will give some examples of treatment strategies.
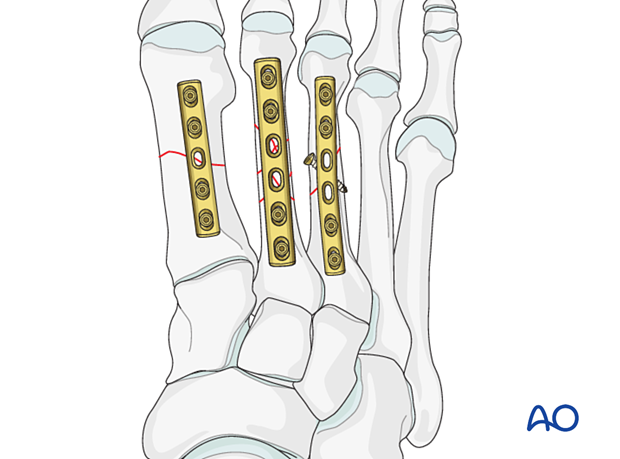
2. Example 1
In this example, the three first metatarsals each have a simple fracture.

The following sequence may be utilized:
- Anatomically reduce and fix the first metatarsal
- Anatomically reduce and fix the second metatarsal
- Anatomically reduce and fix the third metatarsal
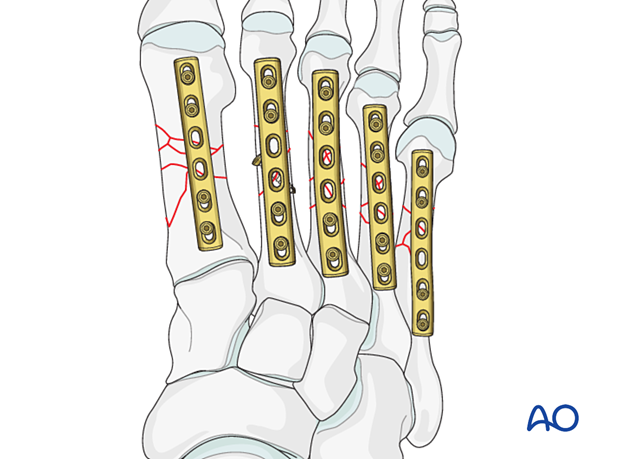
3. Example 2
In this example, the first and third metatarsals are simple fractures, and the second metatarsal is complex.
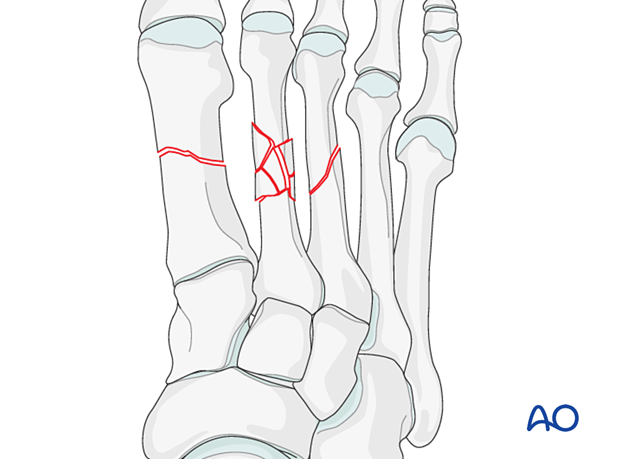
Here the following sequence may be utilized:
- Anatomically reduce and fix the first metatarsal
- Anatomically reduce and fix the third metatarsal
- Reduce the second metatarsal and evaluate the reduction using the contralateral x-ray and the position of the now reconstructed first and third metatarsals. Once sufficient length has been obtained, the position of the second metatarsal head can be secured using a K-wire. Fixation can then be performed using a bridge plate.
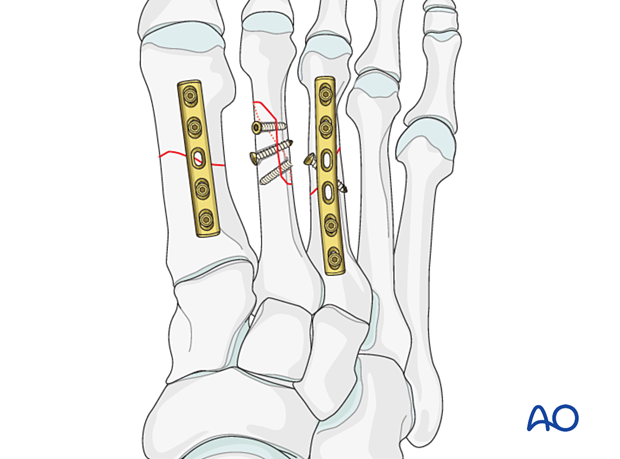
4. Example 3
An anatomical reconstruction will be difficult to obtain when all metatarsals have a complex fracture.
Here imaging of the contralateral foot will be essential for evaluating the reduction.
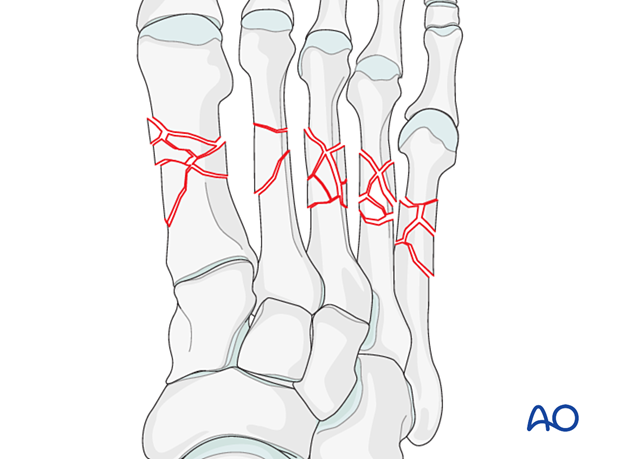
Evaluate if any metatarsals can be anatomically reduced despite the multifragmentary pattern. In this case, the second metatarsal fracture can be reconstructed using lag screws and compression plating; thus, it may be a favorable starting point.
The next step would be to address the first metatarsal using the contralateral x-ray and the second metatarsal as a reference. Once sufficient length has been obtained, the position of the first metatarsal head can be secured using a K-wire. Fixation can then be performed using a bridge plate.
The 3rd, 4th, and 5th metatarsals are then reconstructed consecutively either in a similar manner or by using K-wires.
5. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.
6. Case
This fracture case demonstrates displaced mid metatarsal fractures of the 2nd–4th metatarsals.
Due to the displacement, the fractures were treated operatively.
Sometimes fractures of 2nd–4th metatarsals are nondisplaced if the 1st and 5th rays are not fractured.

Clinical image showing retrograde pinning of the 2nd and 3rd mid metatarsal fractures.

AP postoperative image of 2nd and 3rd metatarsals that have been treated with intramedullary K-wires.
By pinning the 2nd and 3rd metatarsals, the 4th metatarsal was adequately reduced and did not require any hardware.

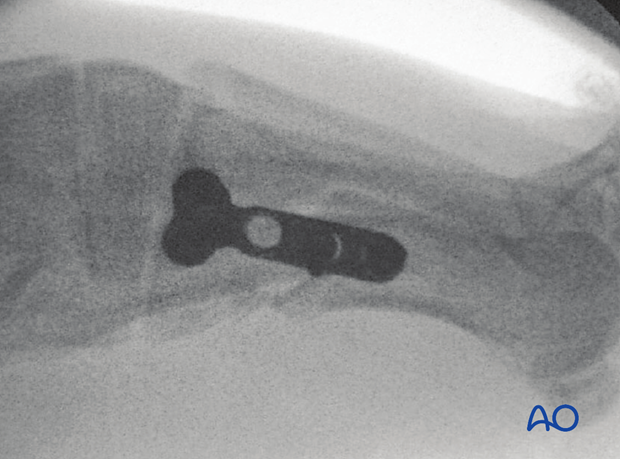
Lateral image of the final fixation.

7. Case 2
This case shows a significant foot injury with an extraarticular base fracture of the 1st metatarsal with associated fractures of the 2nd–4th metatarsals.

AP image showing reduction of the first metatarsal fracture with the resultant alignment of the 2nd–4th metatarsal fractures.
Often the first metatarsal is the key to reducing the other metatarsals because it bears much more biomechanical stress.
The fixation of the 1st metatarsal with subsequent nonoperative management of the 2nd–4th metatarsal may be a very reasonable choice.

Lateral image