Dorsal approach to the 1st metatarsal phalangeal joint (MTPJ)
1. Indications
This approach is helpful for tendon injuries and ORIF of the distal metatarsal, irreducible first MTP dislocations, and proximal phalanx fractures.
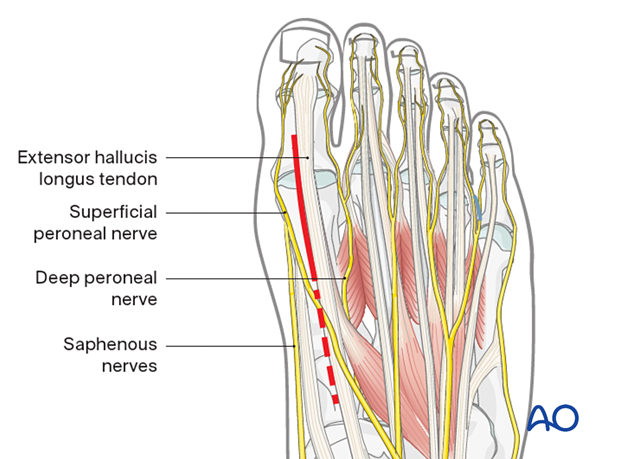
2. Anatomy
The primary structures at risk during this approach:
- The superficial peroneal nerve and digital artery are located dorsomedially at the medial metatarsal
- Crossing superficial dorsal veins will need to be ligated
- The deep peroneal nerve will be lateral
- The extensor hallux longus tendon will be located dorsally at the phalanx, attaching to the distal phalanx

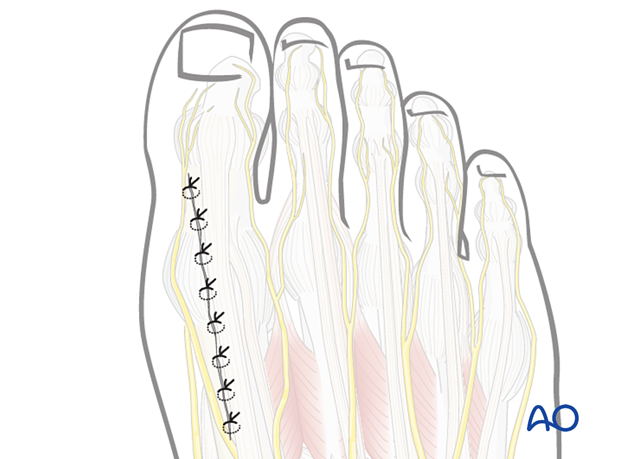
3. Incision
The skin incision runs medial to the EHL tendon at the level of the first MTP joint, between the branches of the deep peroneal nerve, the superficial peroneal nerve, and the saphenous nerves. If needed, the incision can be extended proximally (dotted line) with care to protect the nerve up to and across the first TMT joint.
4. Deep dissection
After dissection through the dermal tissues and coagulating the traversing dorsal veins, retract the EHL tendon laterally to expose the joint capsule.
The capsule can be incised in line with its fibers at the midline of the joint to expose the first metatarsal head and base of the proximal phalanx.
The medial and lateral collateral ligaments can be carefully released from the first metatarsal head if additional visualization is required. Excessive detachment will improve visualization of the joint but will result in joint instability if the collateral ligaments are not reattached.
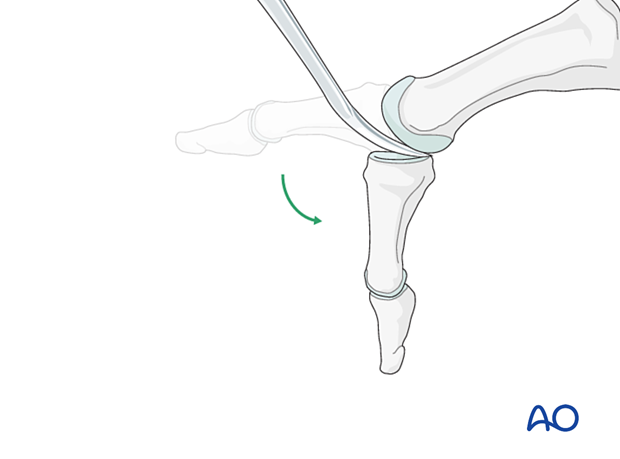
Free the plantar sesamoids with a smooth rounded elevator. Plantar flexion of the hallux will help visualize the articular surface of the metatarsal head.
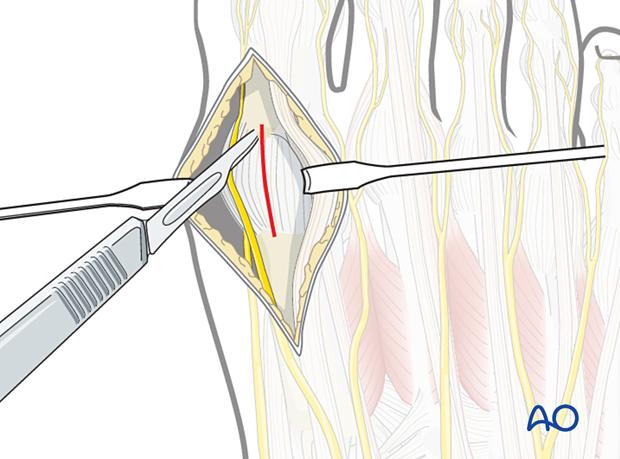
Free the plantar sesamoids with a smooth rounded elevator. Plantar flexion of the hallux will help visualize the articular surface of the metatarsal head and allow partial visualization the articular surface of the proximal phalanx.
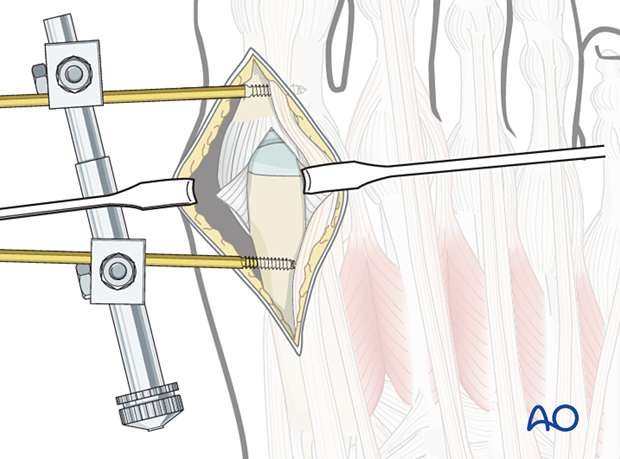
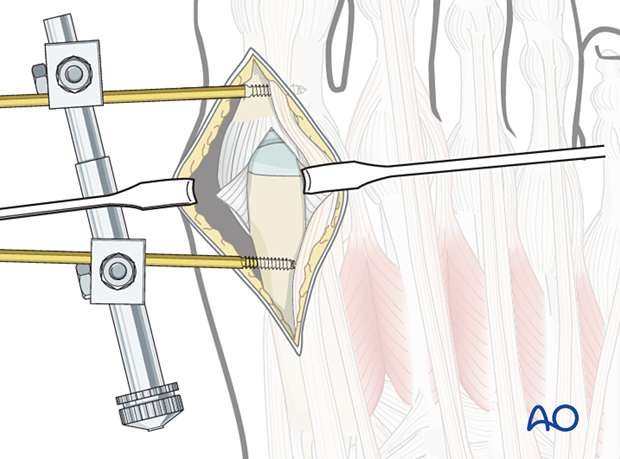
If the surgeon is working alone, a mini distractor or K-wire distractor applied dorsomedially may be helpful to visualize both articular surfaces of the metatarsal phalangeal joint.
5. Closure
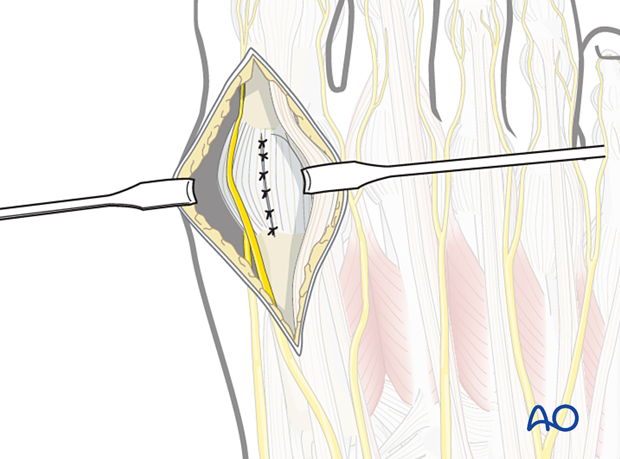
Closure of the capsule
Closure of the capsule can be performed using interrupted sutures.
If excessive collateral ligament detachment was required, repair with suture anchors.
Dermal and skin closure
If possible, skin closure is performed in a layered manner, using a resorbable suture in the dermis and nylon or monofilament for the skin.