Excision arthroplasty
1. General considerations
Excision arthroplasty
Excision arthroplasty is a procedure where one of the two sides of articulation is excised.
Excisional arthroplasty can still preserve motion.
Soft tissue injury
These fractures often have severe associated soft tissue injury.
Repeat debridements may be required.
Temporary stabilization with percutaneous K-wires or external fixators may be placed to promote soft tissue recovery before the definitive procedure.

Anatomical considerations
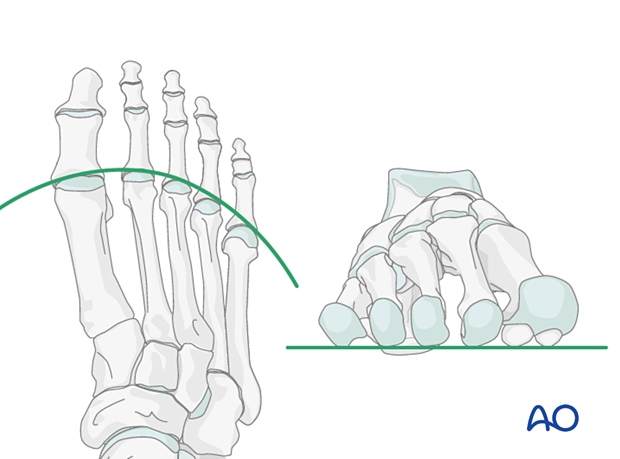
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approach
Selection of approach
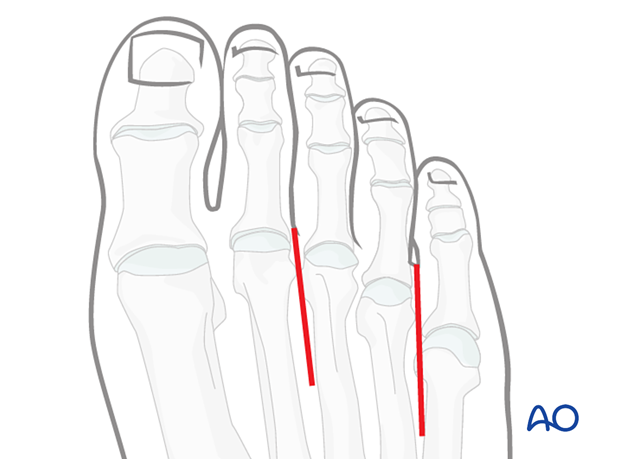
If two adjacent MTP joints are treated, one may center the incision over each digit …
… or utilize one single incision between the metatarsal heads four and five, and if needed, between two and three.
Visualization
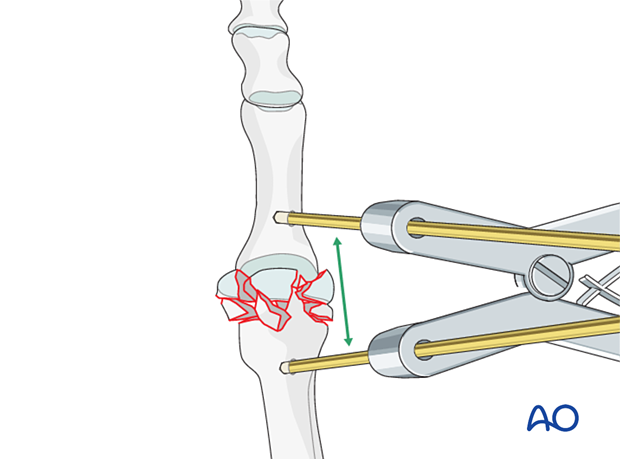
Expose the articular surfaces.
Visualization may be improved by longitudinal manual distraction or a mini distractor.
Alternatively, simple flexion of the joint may provide similar exposure.
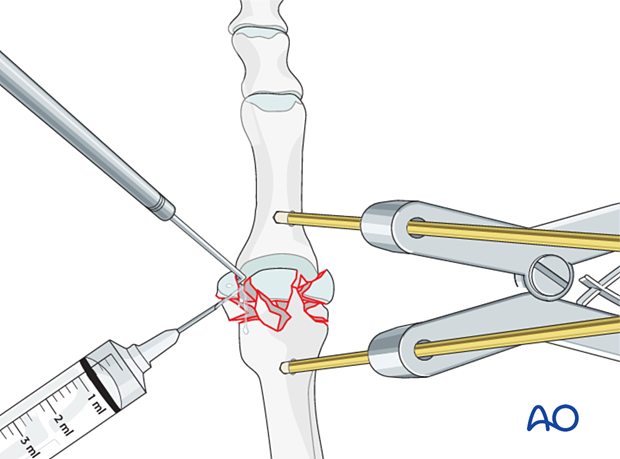
Irrigation
Irrigate the fracture site using a syringe.
Once adequate visualization has been achieved and the joint surface thoroughly irrigated, examine the extent of articular surface involvement to validate the preoperative plan of excision arthroplasty versus fusion.
If joint fragmentation is less than expected, it may be possible to perform internal fixation.
4. Debridement
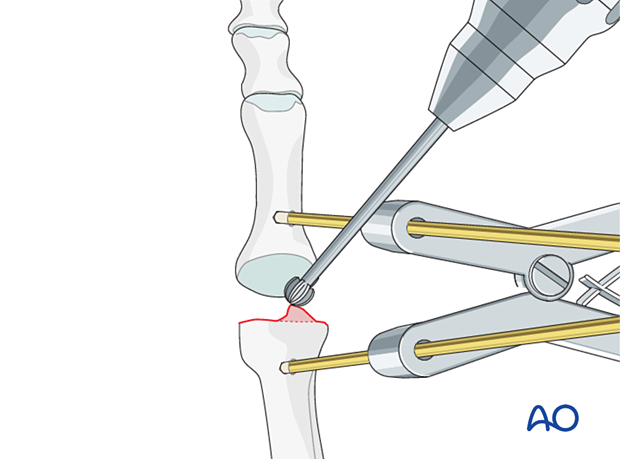
Displaced fragments are debrided and mobilized with a dental pick or Freer elevator.
All osteochondral fragments are removed.
It is desirable to leave cancellous fragments as they can help maintain length.
It is not necessary to remove the cartilage of the adjacent bone.
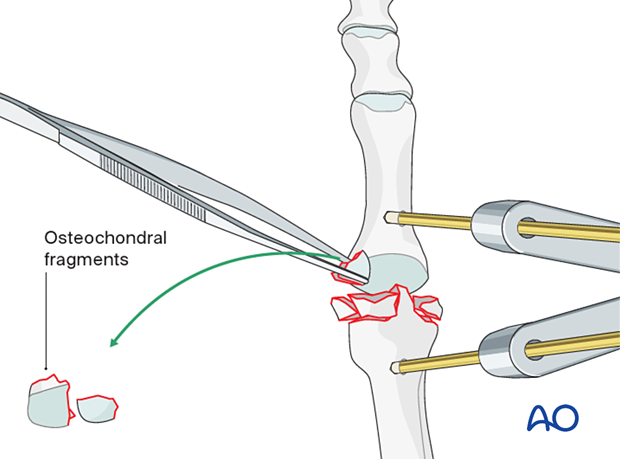
Debride fracture edges which may damage the adjacent intact joint surface.
5. K-wire insertion
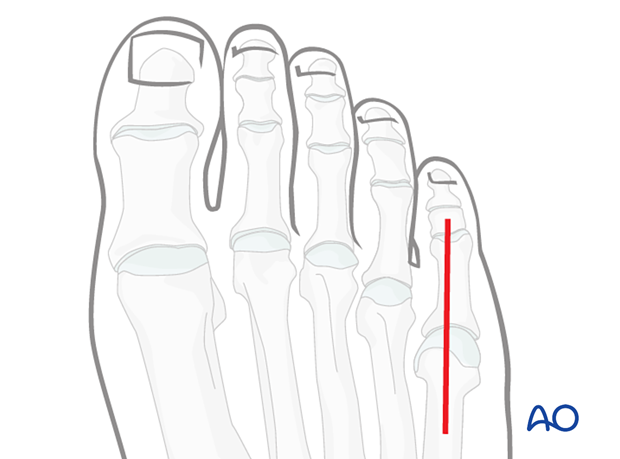
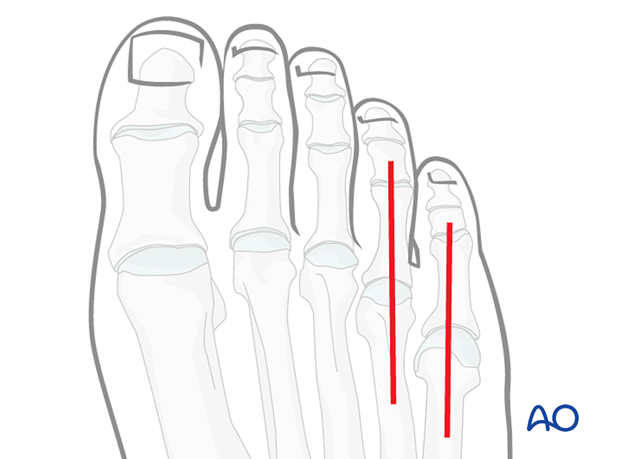
K-wire trajectories
An axial K-wire is inserted temporarily to maintain alignment.
Crossed K-wire configuration may be used if not obstructed by the adjacent phalanges.
While this technique spares the distal interphalangeal joint, it can be more challenging to perform.
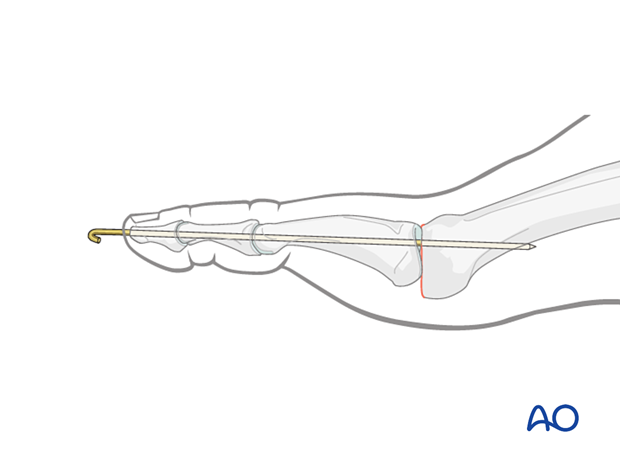
Axial K-wire insertion
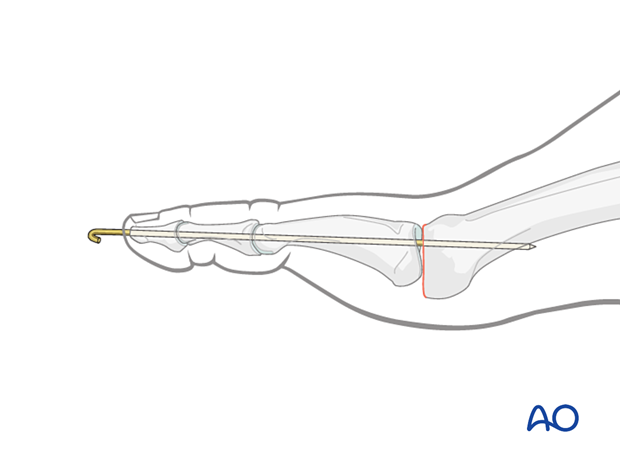
Marking K-wire trackTo avoid unnecessary radiation from image intensification, mark the K-wire's planned track with a skin marker (or methylene blue) on the distal phalanx in both the AP and the lateral aspects.

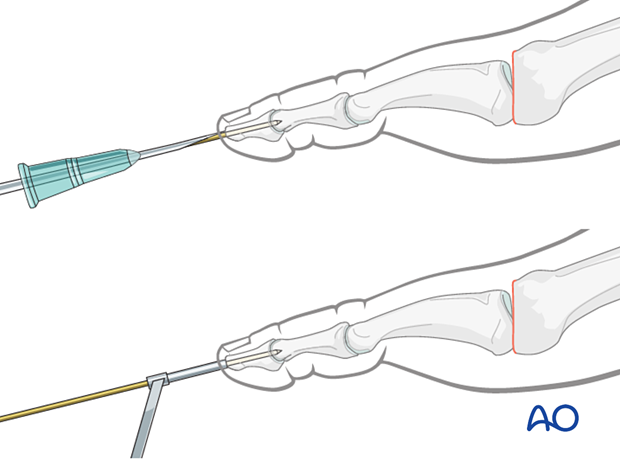
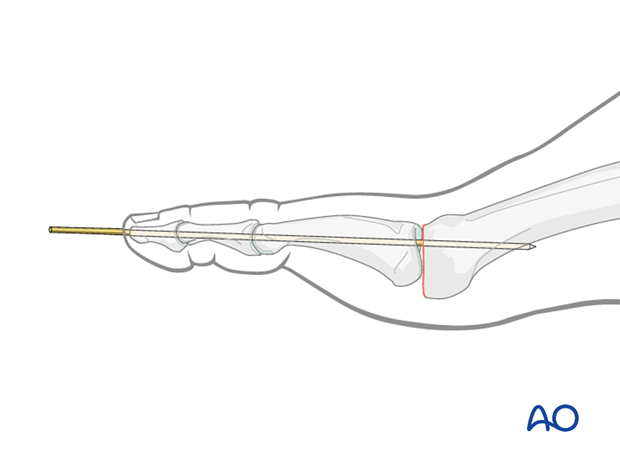
To prevent the K-wire from slipping during insertion, either a 16 gauge hypodermic needle or a small-caliber drill guide can be used.
Both techniques help insert the K-wire in the center and along the longitudinal axis of the phalanx.
Try to avoid injury to the germinal matrix or the nail during wire insertion.
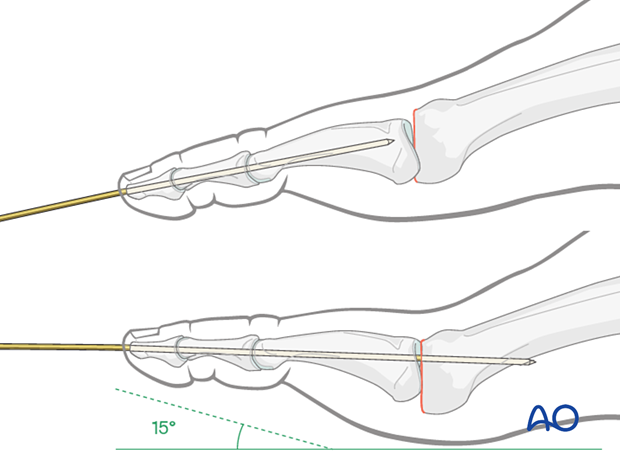
Advance a 1.4 wire until it is secured in the bone proximal to the treated joint.
Typically, the PIP joint is secured in a neutral position.
The toe is positioned with 15° of dorsiflexion for the MTP joint relative to the floor (foot sole).
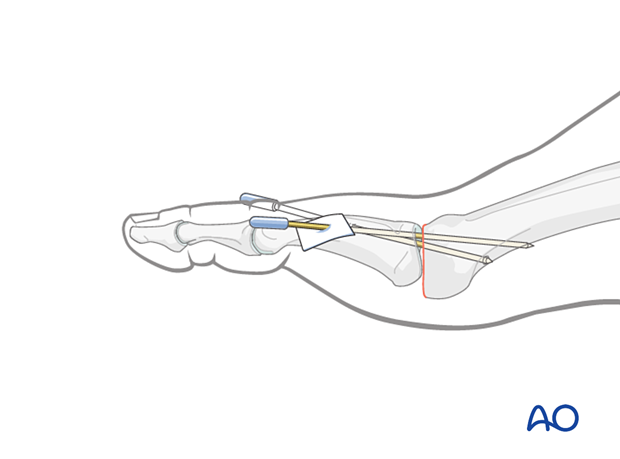
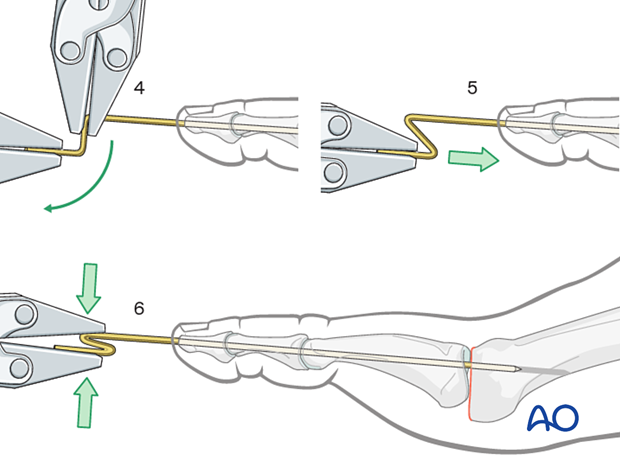
Cut the K-wire so that it protrudes through the skin, about 1 cm from the tip of the digit. Bend its end to form a tight U-configuration to prevent catching on clothing and other objects.
Leaving the K-wire to protrude through the skin in this way has the advantage of its being easy to remove. The disadvantages are patient discomfort and the risk of pin-track infection.
The tip can be protected with a pin cap.
Distract the wire a little to simplify the bending.
Bend the tip of the wire 90°.
Distal to the first 90° angle, bend the wire again to a 90° angle so that the distal portion is parallel to the inserted portion of the wire.
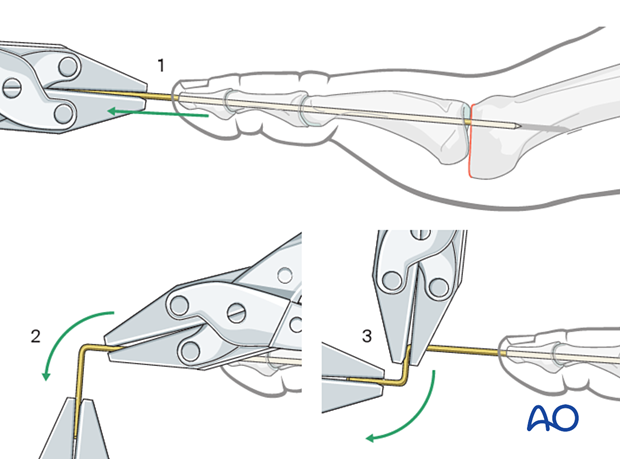
An axial force can be applied to the distal end of the wire to achieve a U-bend of the first angle.
Further tightening of the U-bend can be achieved by squeezing the loop with a clamp.
The distal portion is then cut and the wire re-inserted.
Crossed K-wire insertion
Insert two crossing K-wires from dorsal distally to plantar proximally. The K-wires should not cross each other at the joint.
K-wires should be inserted percutaneously.
The K-wire should be long enough to ensure the stability of the construct. Overly long K-wires should be avoided to minimize soft tissue irritation.
Typically, the PIP joint is secured in a neutral position.
The toe is positioned with 15° of dorsiflexion for the MTP joint relative to the floor (foot sole).
The K-wires are cut and covered with caps and dressing.

6. K-wire removal
Typically the K-wires are kept for 6–8 weeks and then removed before ambulation.
7. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













