Complications and technical failures
1. General considerations
The most frequent complications are related to soft-tissue problems including tendon adhesions, intraarticular fibrosis, and scarring around implants and the surgical site. Attention to careful soft-tissue management and early rehabilitation including mobilization and appropriate splintage are all relevant to prevention of these problems.
Complications associated with fractures in the hand include:
- Severe soft-tissue loss including skin, muscle, and tendon
- Delayed wound healing
- Nerve injuries, altered sensibility
- Ischemia
- Compartment syndrome
- Infection
- Peritendinal fibrosis
- Loss of reduction
- Malunion or nonunion
- Stiffness (complications with nonoperative treatment)
- Arthritis
- Loss of function including grip weakness
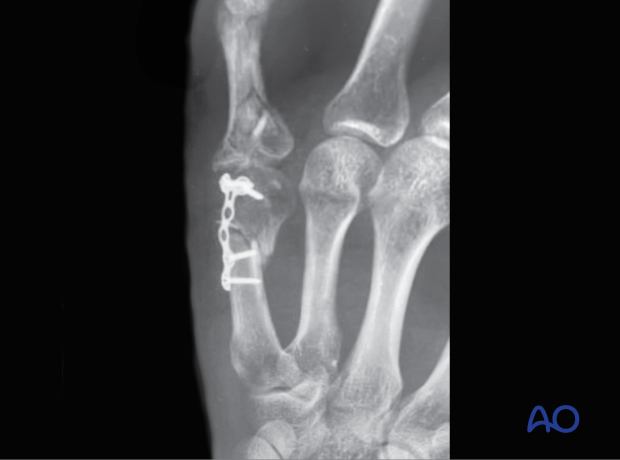
This case shows severe inflammatory reaction and cartilage compromise in a fracture of the 5th metacarpal head with screw fixation.

The x-ray of this case shows an articular screw protrusion.

2. Wound healing
Significant swelling, particularly when associated with blistering, may necessitate a delay in surgical treatment.
The hand is protected with a splint until the condition of the skin and soft-tissue envelope has improved.
In some cases, a temporary external fixator is necessary to provide sufficient stability.
Definitive surgery should be delayed until the skin and soft tissues recover.
3. Soft-tissue, skin, and tendon issues
Frequent tendon issues include flexor and extensor adhesions after surgery. This can be prevented with a correct functional position of the hand in a dorsal splint and early mobilization.
The skin over implants may get irritated. Closure of the periosteum over the implant can help to prevent this.
Open fractures with severe skin compromise require specific skin management (flaps). A surgeon familiar with these techniques should be available.
4. Loss of reduction
Loss of reduction may result from inadequate fixation of an unstable injury.
This can be prevented by:
- Checking for soft-tissue interposition
- Assessing stability after reduction
- Using suitable implants, eg, appropriately sized plates/anatomical implants
- Confirming stability after fixation
5. Malunion
Malunion is usually a consequence of inaccurate reduction and ineffective fixation.
It strongly affects the balance of flexor and extensor mechanisms and biomechanical relations of the hand. For example:
- Angulation may result in loss of grip strength.
- Rotation is usually associated with an oblique or spiral fracture and may result in loss of length leading to reduction of dexterity.
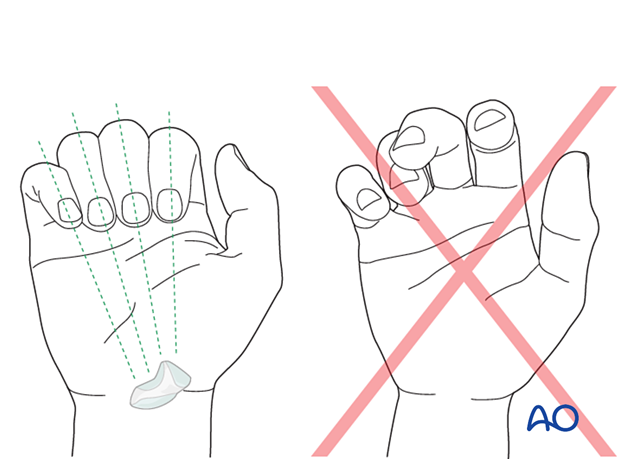
- Rotational malalignment will also compromise palmar grip due to conflict with neighboring fingers.
This case shows a rotational and axial malalignment with nonunion of a distal diaphyseal fracture of the 5th metacarpal. The proximal intraarticular complex fracture of the 5th proximal phalanx is also maluniting. This will cause stiffness of the MCP joint. Attempts to use the little finger, for instance for power grip, will result in transfer of bending and rotational forces to the proximal metacarpal. In this case eventual fatigue failure of the plate is highly likely.
It is crucial to confirm any alteration of alignment, especially length, angulation, and rotation. All fingers should point to the scaphoid tubercle.
6. Nonunion
Nonunion may be the result of insufficient fracture reduction and/or stabilization.
Confirm proper reduction, anatomical in articular fractures, before and after fixation in AP, lateral, and oblique views. Select the optimal fracture fixation based on fracture configuration, fracture biomechanics, the likely healing mode, and patient needs, expectations, and compliance.
7. Complications with nonoperative treatments
Inappropriate stabilization with a splint may lead to redisplacement, malunion, (hypertrophic) nonunion, and stiffness.
Intrinsic muscle contracture, collateral ligament fibrosis , and subsequent limitation of movement may occur if the hand is immobilized incorrectly.
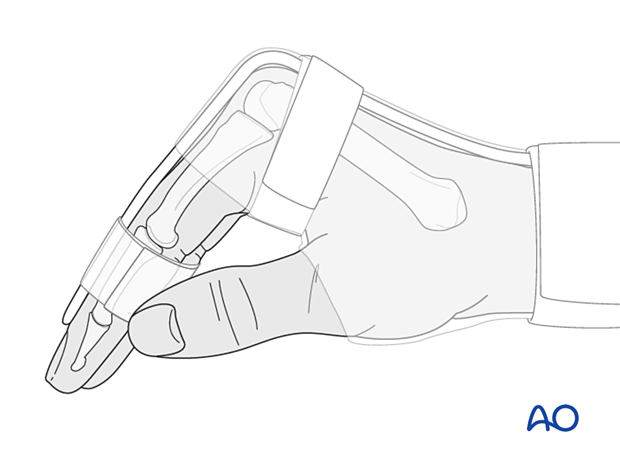
To lower these risks, a dorsal splint should be applied with the hand in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- Metacarpophalangeal (MCP) joint in 90° flexion
- Proximal interphalangeal (PIP) joint in extension
In noncompliant patients, additional K-wire fixation may be considered.
8. Stiffness
Long periods of immobilization or unstable fractures with pain may cause joint stiffness.
The patient should be instructed to mobilize the joints as soon as possible.
Unstable fractures should be reevaluated, and secondary surgical treatment should be considered.













