Dorsal approach to the metacarpophalangeal joints
1. General considerations
Indications
This approach is indicated for:
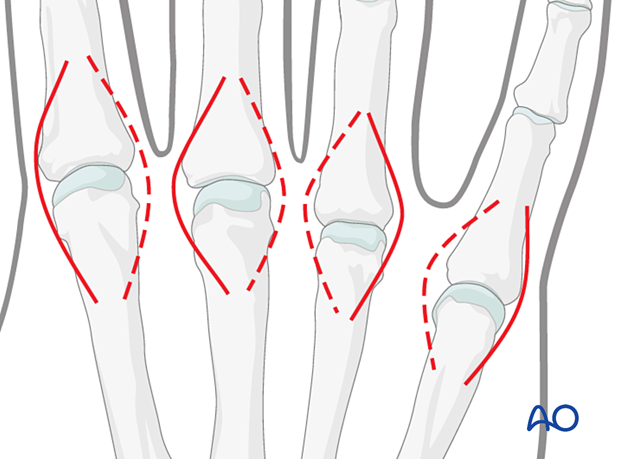
- Intraarticular fractures of the metacarpal head
- Injuries of the metacarpophalangeal (MCP) collateral ligaments (either avulsion fractures or ligament ruptures)
- Intra- or extraarticular fractures of the base of the proximal phalanx
AO teaching video
Dorsal Approach to Metacarpo-Phalangeal (MP) Joint of the Finger
2. Surgical anatomy
Tendinous anatomy
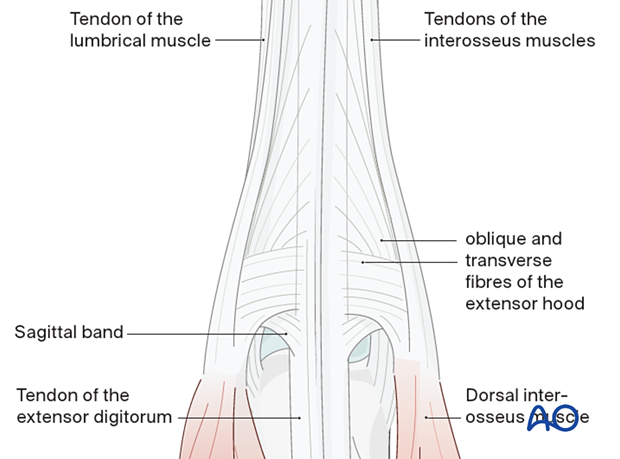
The extensor digitorum tendons and the extensor hood cover the MCP joints dorsally. The extensor tendon receives the insertions of the tendons of the interosseous and lumbrical muscles via the extensor hood.
Proximal to the 2nd MCP joint, the extensor indicis tendon lies ulnar to the extensor digitorum tendon. At the 5th MCP joint, the extensor digiti minimi tendon is ulnar to the extensor digitorum tendon.
Nerve identification
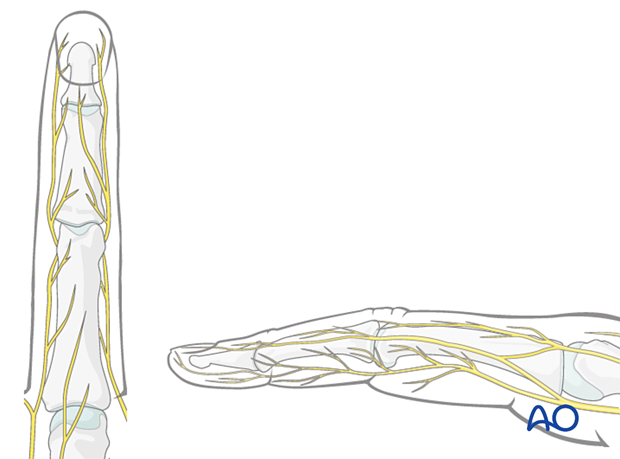
In the thin subcutaneous tissue, identify and protect the dorsal sensory branches of the radial and ulnar nerves.
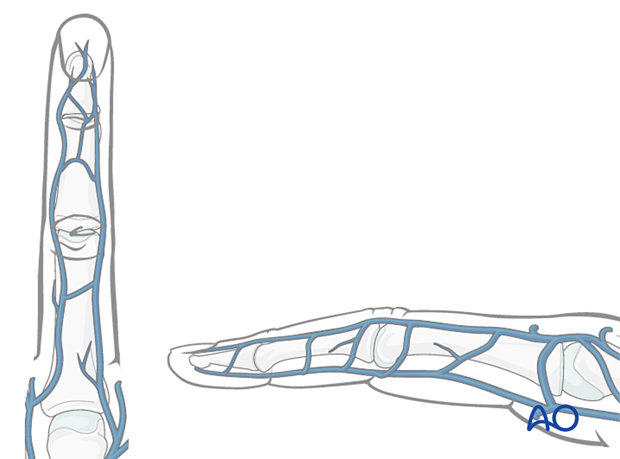
Vein identification
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized, but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
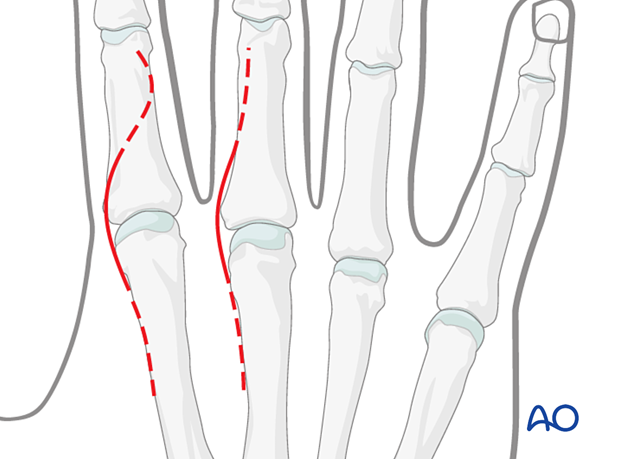
3. Skin incision
Perform a gently curved longitudinal incision over the MCP joint.
Depending on the fracture pattern, place the incision over the dorsoradial or dorsoulnar aspect of the MCP joint. A radially curved incision is preferred over the 2nd MCP joint and a dorsoulnar curved incision over the 5th MCP joint.
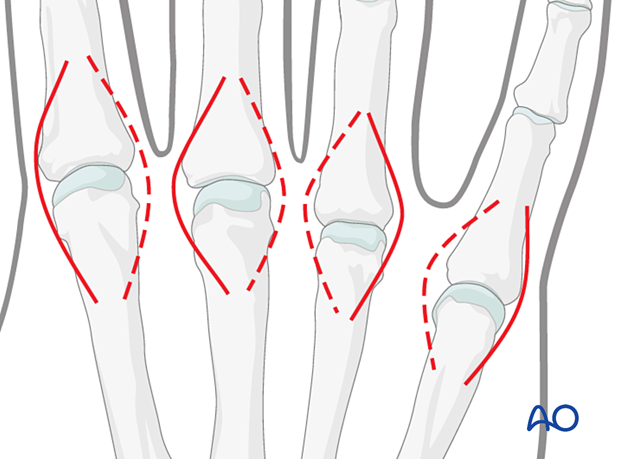
Extension of the incision
If necessary, extend the incision distally or proximally in a curvilinear or longitudinal manner.
4. Exposure of the extensor apparatus
Elevate the skin flap from the extensor apparatus without damaging the surrounding loose connective tissue, the sensory nerve branches, or the longitudinal veins.
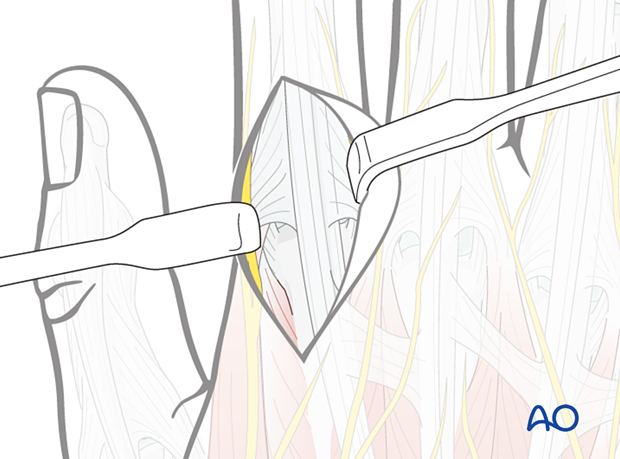
5. Exposure of the joint capsule
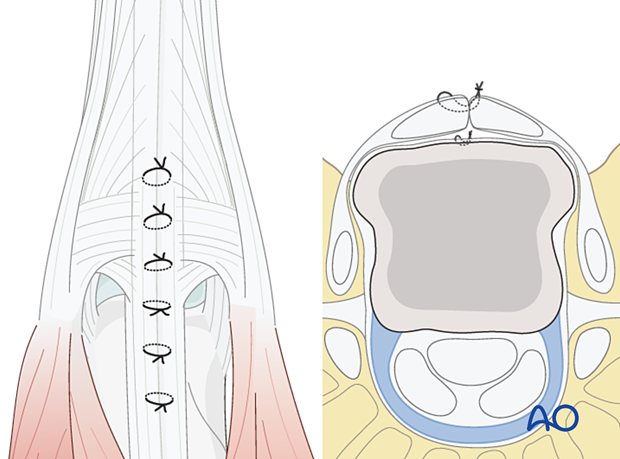
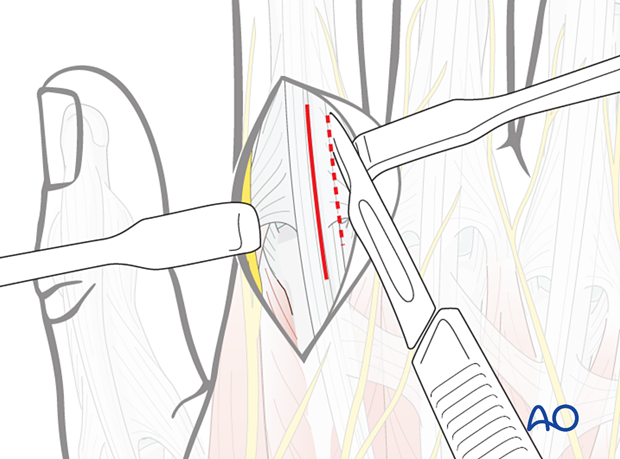
The extensor digitorum tendon can be split longitudinally. In the index and little fingers, the incision can be made between the two extensor tendons.
Alternatively, the extensor hood can be incised parallel to the extensor digitorum tendon, leaving a small fringe for subsequent repair. Depending on the fracture pattern, the incision in the extensor hood is dorsoulnar or dorsoradial.
In general, a dorsoulnar incision is preferable to prevent subluxation of the extensor tendon to the ulnar side should the repair fail.
6. Capsulotomy
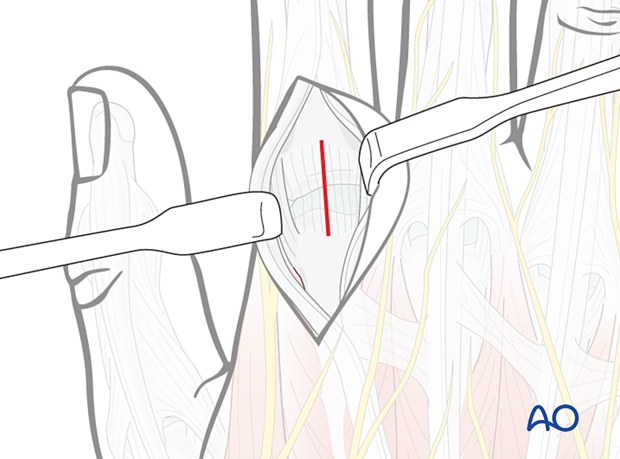
In general, a longitudinal capsulotomy is made to open the MCP joint.
7. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle prior to wound closure.
Repair the joint capsule with fine sutures with the fingers as if in opposition to the thumb.
Cover the implant with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.
Repair the sagittal band if damaged or incised to avoid subluxation of the extensor mechanism.
If an intertendinous connection has been cut, it should be repaired.