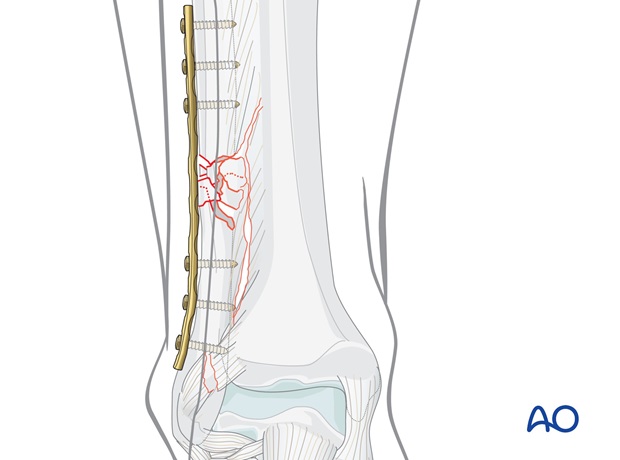
Fibula, multifragmentary C fracture: lateral bridging plate
1. Principles
Bridging
Bridge plating uses the plate as an extramedullary splint, fixed to the two main fragments, while the fracture zone is left virtually untouched.
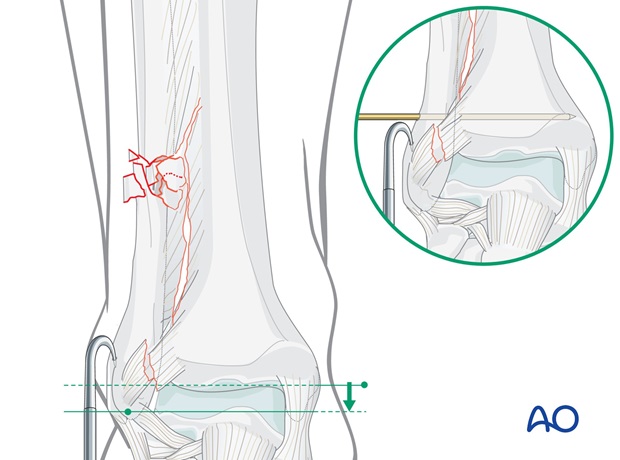
Reduction of the distal tibiofibular joint is important Therefore, restoration of the length, axis and rotation of the fibula is crucial. and must be checked intraoperatively under image intensification.
Reduction can usually be achieved indirectly by distraction. Anatomical reduction in the fibular fracture zone is not necessary.

Bridging plates are commonly used in multifragmentary lateral fractures.
Mechanical stability
Mechanical stability, provided by the bridging plate, should be adequate for indirect healing (callus formation).
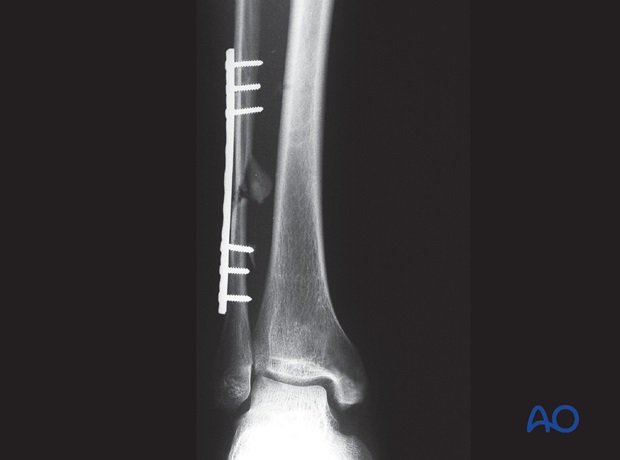
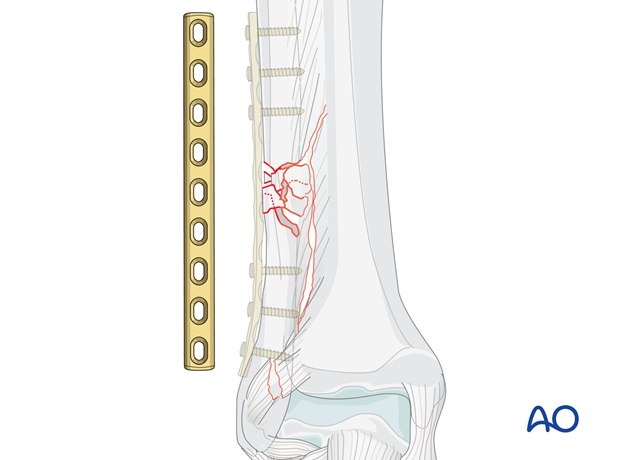
In cases of large zones of comminution, stronger plates, such as reconstruction plates or locking compression plates (LCP), provide better stability than one-third-tubular plates.
The angular stability provided by the LCP may be advantageous.
Mechanical stability (syndesmosis)
In suprasyndesmotic fractures (Lauge-Hansen type PE 4), the syndesmosis complex is usually unstable.
2. Reduction
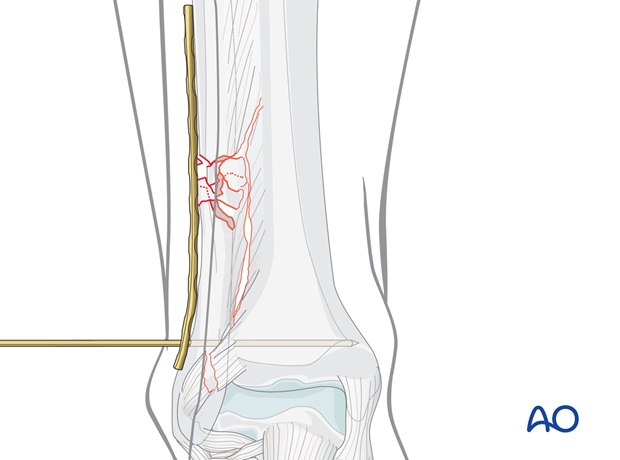
In multifragmentary fractures, care must be taken to avoid excessive stripping of the periosteum as well as devascularization of the fragments.
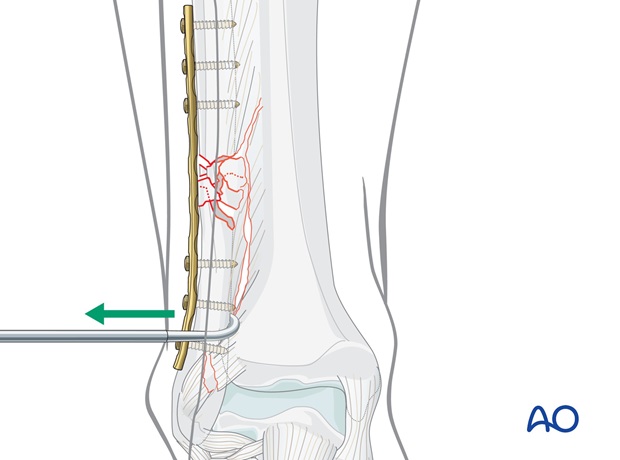
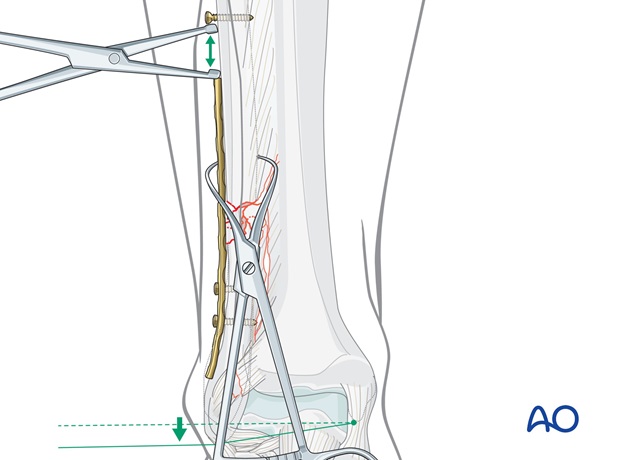
Indirect reduction may be obtained by longitudinal traction, either on the foot, or of the main distal fragment using a bone hook.
In a suprasyndesmotic fracture, once the lateral malleolus is reduced in its anatomic position, it may be helpful to insert a K-wire, 30 degrees from dorsal, 2-3 cm supramalleolar.
Reduction with the plate
Alternatively, the plate can be used for gaining length after fixing it to the distal fibular fragment (see step 4).
For this purpose, insert a screw into the fibula proximal to the plate and distract the fracture to the correct length with a laminar spreader. When tension on the plate can be felt, secure the plate to the fibula with pointed reduction forceps applied through a hole in the plate.
Check rotation and the position in the incisura fibularis before fixing the plate to the proximal fibula.
3. Plate preparation
Plate selection
Anatomic plates with locking screw option are available from various manufacturers. To illustrate the principles of the procedure, the use of a classic plate is described.
Plate length
The plate must be long enough both to cover the length of the fracture zone and ideally to allow insertion of three screws in each main fragment.
Contouring the plate
Before the plate is applied, it must be contoured.
Contouring is best done with the help of the appropriate aluminum template. The plate should perfectly fit the bone contour throughout its entire length.
If a plate with locking screws is used on the shaft of the fibula, it does not have to fit perfectly against the bone.
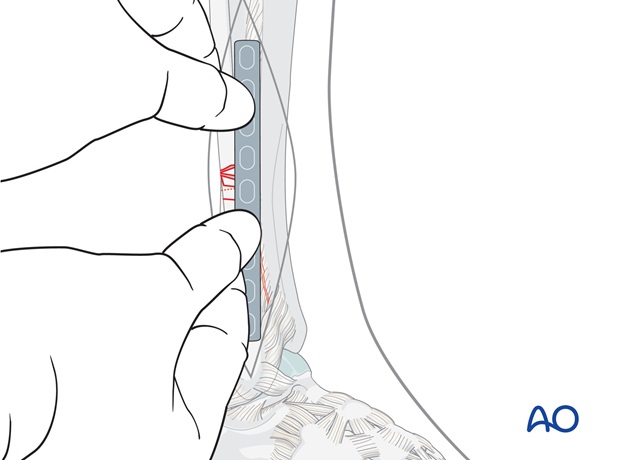
Plate position
Position the plate firmly by hand and plan the position of the first proximal screw near the fracture.
Remove the plate.
4. Fixation of multifragmentary suprasyndesmotic fractures
Applying the plate after preliminary fixation with a K-wire
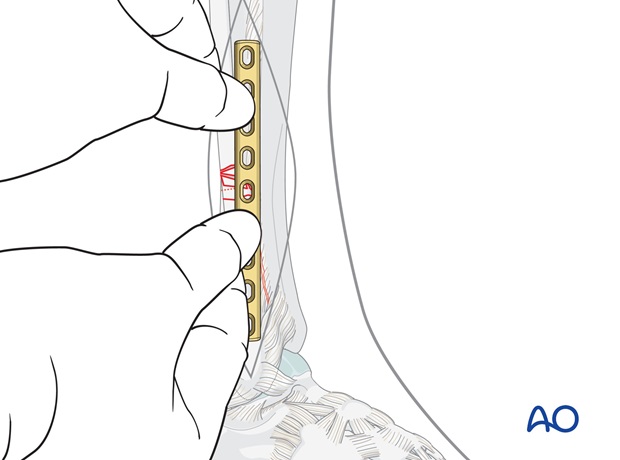
If the fracture has been preliminarily fixed with a K-wire, position the plate over the K-wire.
If the wire gets in the way of the plate, it can be advanced to project medially and then cut off flush with the lateral fibular cortex. This way it can be removed medially after the plate has been applied over it.
Screw insertion
Drill a pilot hole through the first plate hole distal to the fracture zone, using a 2.5 mm drill bit and protection sleeve.
Measure the depth with a depth gauge and insert the first cortex screw into the distal fragment.
Next insert the three proximal screws, then complete screw insertion in the distal fragment, remove the K-wire, and check the syndesmotic stability.