MIO transdeltoid lateral approach to the humerus
1. Introduction
The MIO transdeltoid lateral approach can be used for the more proximal humeral shaft fractures. It is especially useful if there is an extension of the fracture into the greater tuberosity.
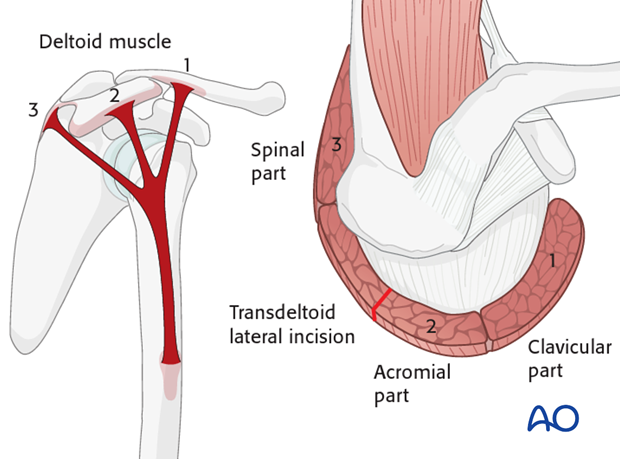
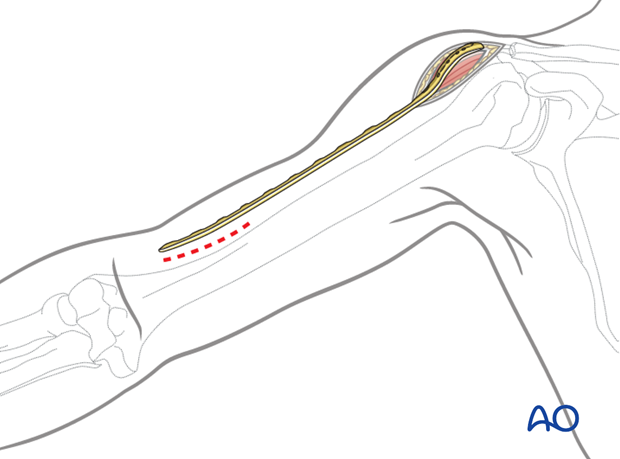
This incision is placed between the acromial part (2) and the spinal part (3) of the deltoid muscle, as illustrated.
The skin incision should not extend more than 5 cm distally to the acromion, to protect the axillary nerve.
2. Anatomy
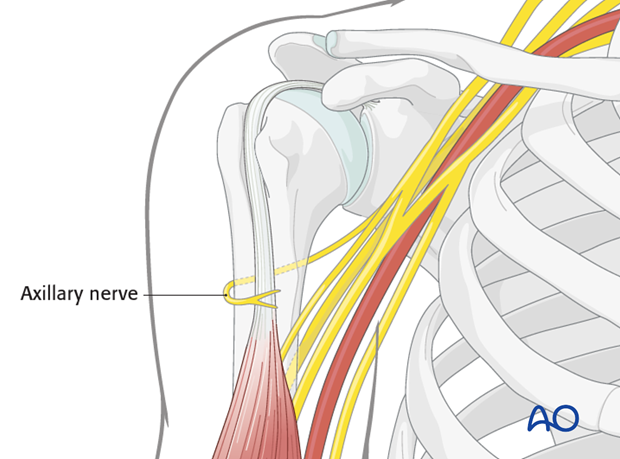
Neurovascular structures
The course of the axillary nerve must be kept in mind.
Note: The anterior motor branch of the axillary nerve crosses the humerus horizontally about 6 cm distal to the lateral border of the acromion. This distance does not vary significantly and is reliable.
Anatomical landmarks
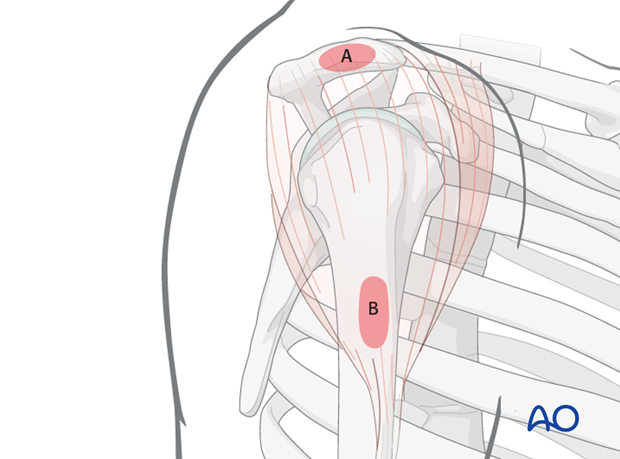
Anatomical landmarks for the transdeltoid lateral approach are:
A) Lateral border of the acromion
B) Lateral side of the humeral shaft
Both landmarks can easily be palpated.
3. Skin incision
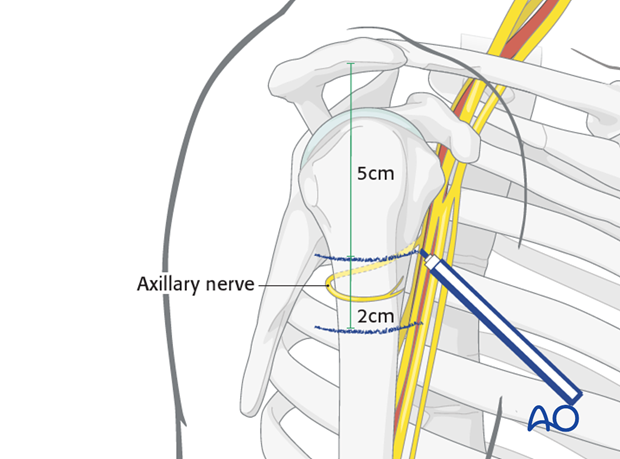
Axillary nerve
Before incising the skin, mark the distal limit of the approach, 5cm below the acromion, which is 1 cm above the course of the axillary nerve.
Mark a second line 2 cm distal to the first, below which the axillary nerve should not be encountered. The space between these two lines is the danger zone on the lateral humerus.
Skin incision
Make a skin incision from the lateral border of the acromion 5 cm distally, parallel to the axis of the humerus.
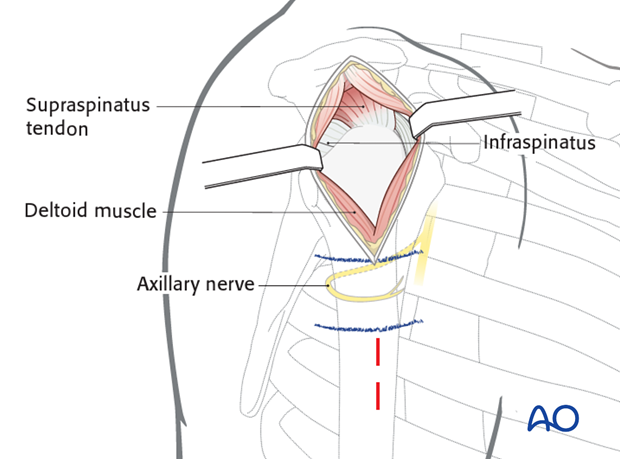
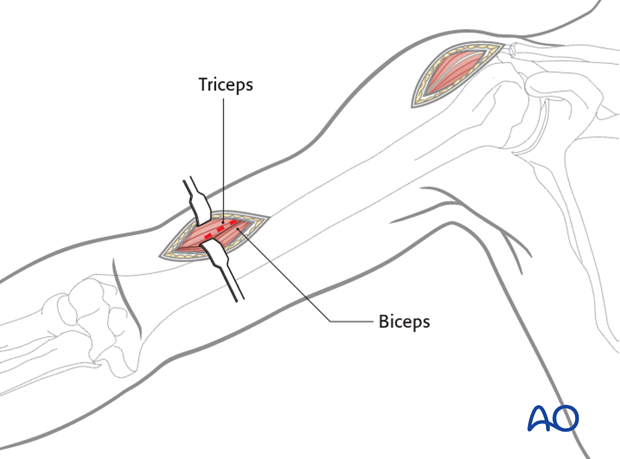
4. Exposure of the middle third part of the deltoid muscle
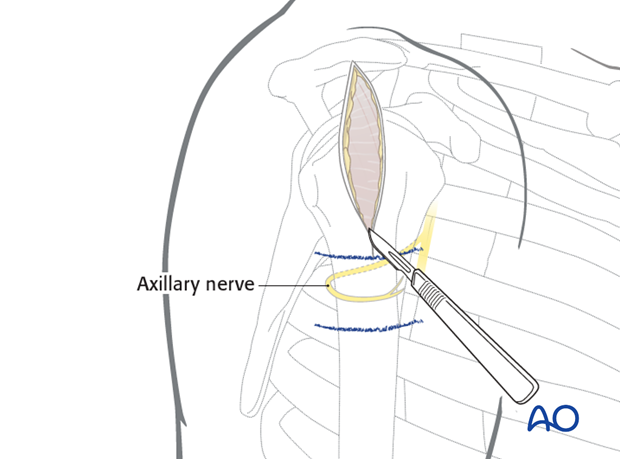
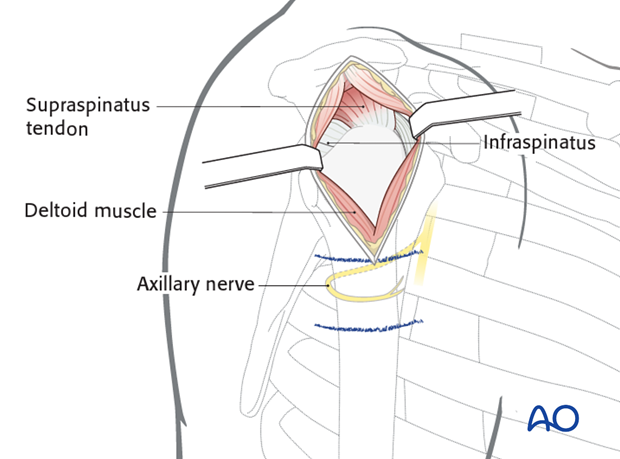
Expose the middle third (acromial) part of the deltoid muscle and split it between its fibers.
For maximum exposure, split the deltoid up to the margin of the acromion, but do not split it distally more than 5 cm from its origin to avoid damaging the axillary nerve and paralyzing the anterior part of the deltoid.
Palpate the axillary nerve on the deep surface of the deltoid muscle, distal to the incision. This nerve encircles the proximal humerus a little less than half way from the lateral margin of the acromion to the insertion of the deltoid muscle.
Hemorrhagic subdeltoid bursal tissue may need to be excised to expose the humeral head.
Pearl: To protect the axillary nerve from uncontrolled distal dissection, a stay suture may be placed at the inferior border of the deltoid split.
5. Distal incision
Place the selected plate on the arm with the proximal end level with the intended final placement. This indicates the site of the distal portal.
Distal access is gained between the biceps and triceps to reveal the lateral humeral surface. Depending on the level of the incision the radial nerve may have already entered the anterior compartment and is at risk. It should be identified and protected.
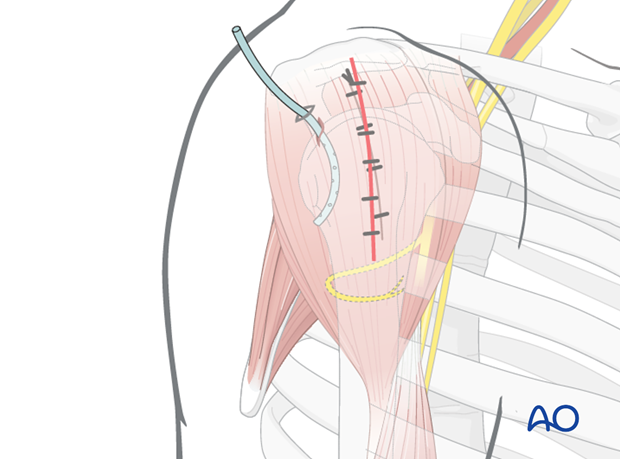
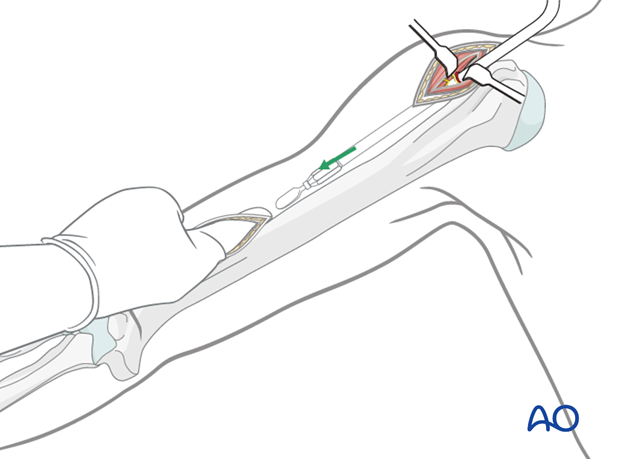
6. Creating the tunnel
Pass an instrument carefully under the axillary nerve and its vessels, to elevate them gently and create a plane deep to them.
The illustrated large probe or dissector is then used to pass distally beneath the deltoid and slid through the deltoid insertion.
As the tip of the instrument nears the distal portal, it should be palpated and guided into alignment with the humeral shaft.
7. Pitfall: nerve damage
Take care not to injure the axillary nerve and its accompanying vessels.

8. Wound closure
After surgery irrigate the wound. Some surgeons place a drain beneath the deltoid muscle.
Close the deltoid fascia, the subcutaneous tissues and the skin.