Midaxial (lateral) approach to the proximal phalanx
1. Introduction
The midaxial approach, also known as lateral, to the proximal phalanx gives access to the midaxial ligaments, the proximal phalanx, and the proximal and distal end segments.
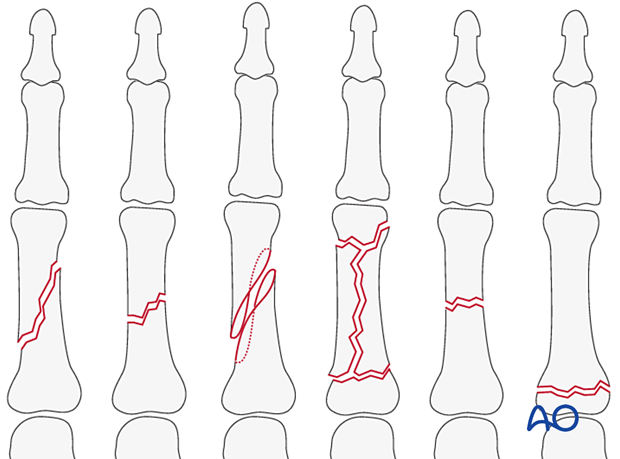
This approach is indicated for the treatment of the following fracture types of diaphysis and metaphysis:
- Oblique
- Spiral
- Transverse
- Multifragmentary
It is also indicated for proximal metaphyseal fractures.
AO teaching video
Lateral Approach to Proximal Phalanx of the Finger
2. Surgical anatomy
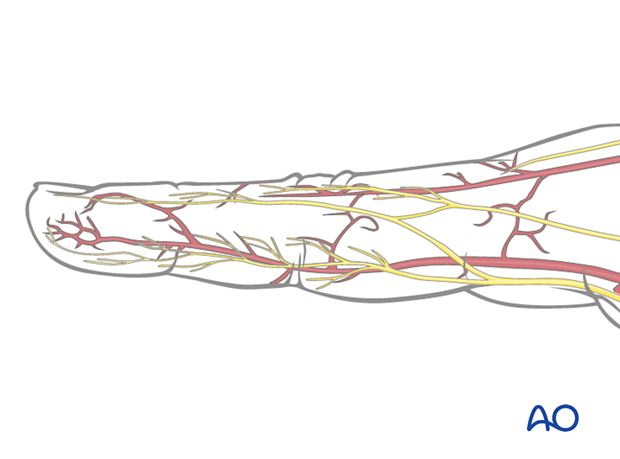
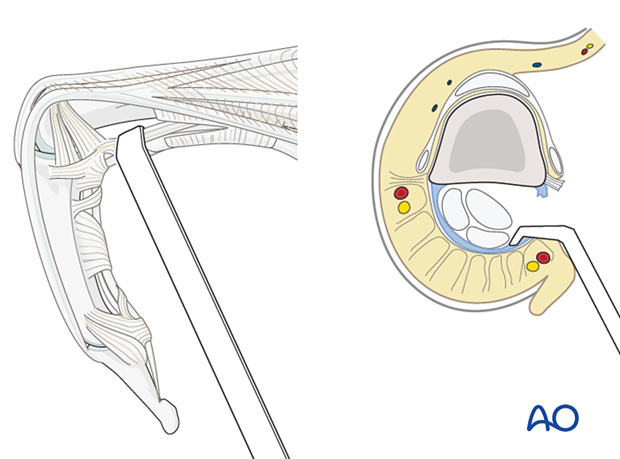
Nerve identification
In the thin subcutaneous tissue, identify and protect the dorsal sensory branches of the radial and ulnar nerves.
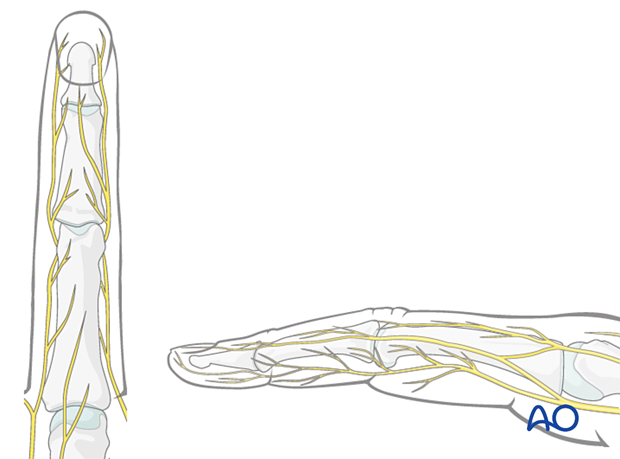
Identification of vascular structures
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized, but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
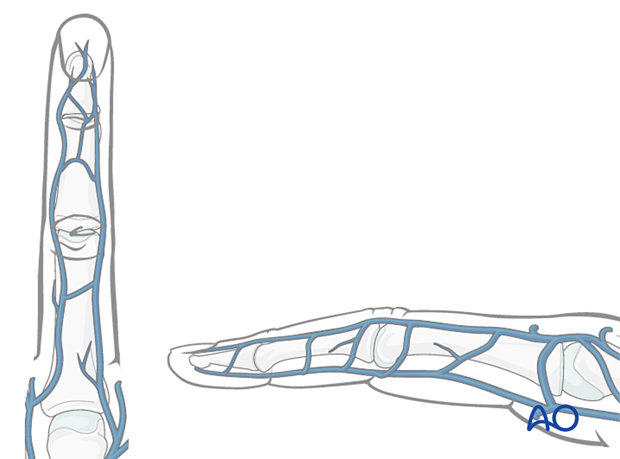
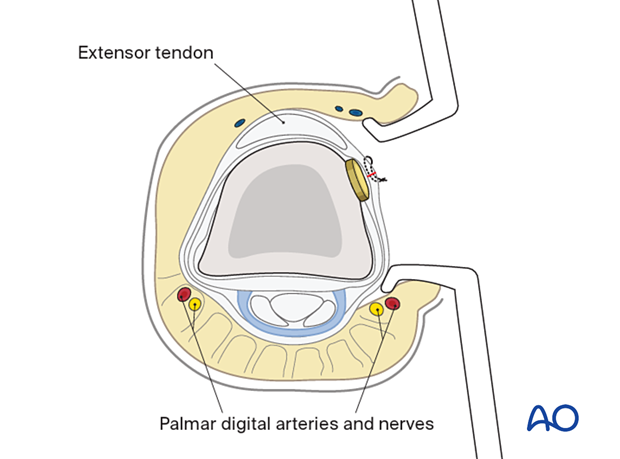
The digital artery and nerve lie palmar to the midaxial line in collateral relation with the flexor tendon sheath.
3. Skin incision
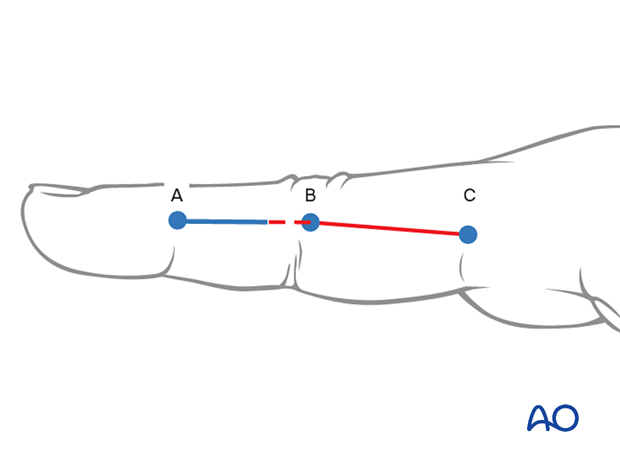
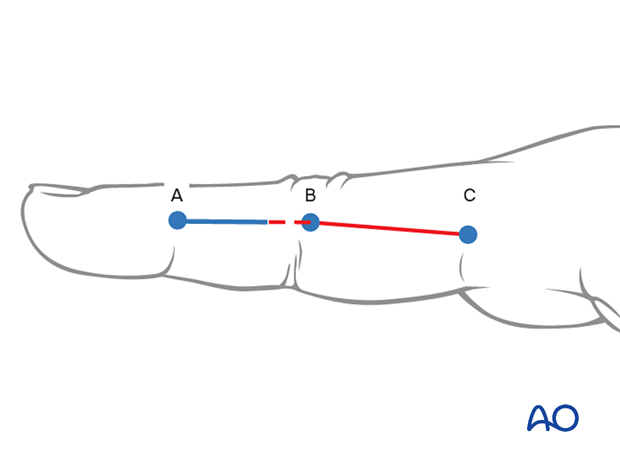
To plan the incision line, fully flex the finger as shown and mark the dorsal ends of the flexor creases with dots.
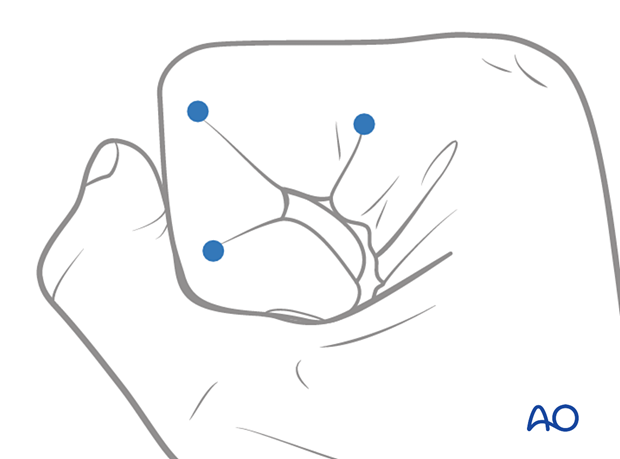
Extend the finger and connect the dots in a line.
The resulting line is safe for a midaxial skin incision. The digital artery and digital nerve will lie palmar to this line.
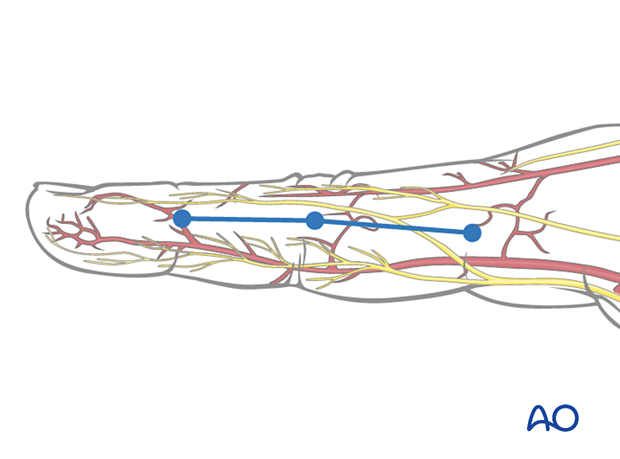
For proximal fractures, perform a skin incision from B to C. For further exposure, the incision can be extended to A.
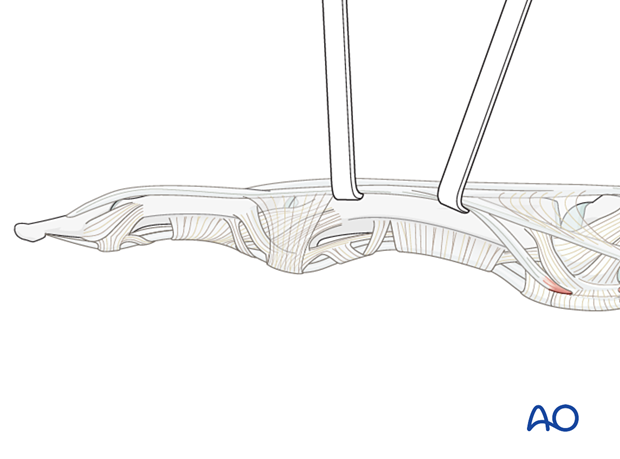
Intraoperative image of the skin incision

4. Deep dissection
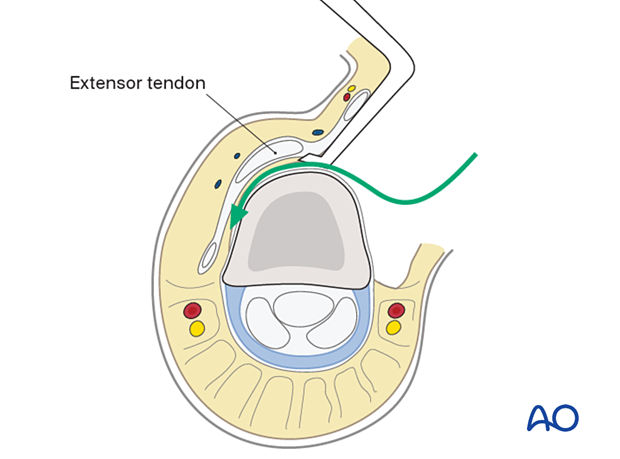
Retraction of the oblique fibers of the lateral band
Retract the oblique fibers of the lateral band using two retractors.
To avoid scar formation, tendon adhesion, and fragment devascularization, try to preserve the periosteum, which should be elevated only immediately adjacent to the fracture line.
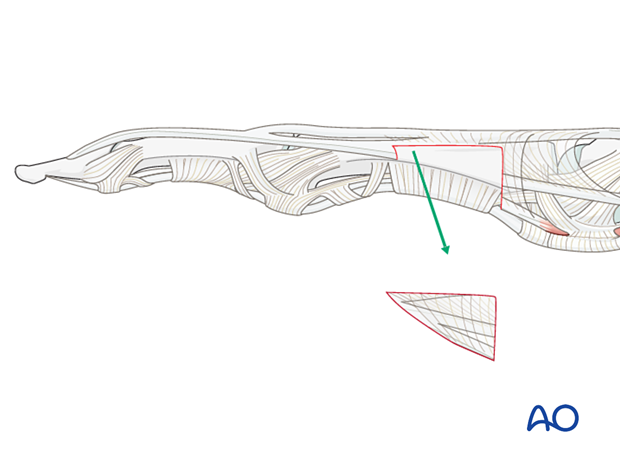
Alternative: resection of the oblique fibers of the lateral band
For the visualization of very proximal fractures, it is occasionally necessary to resect unilaterally oblique fibers of the lateral band.
This resection also avoids impingement with the planned implant and intrinsic tendon adhesions.
Palmar access
Generally, avoid penetration of the flexor tendon sheaths.
In the case of tendon laceration, however, the midaxial approach can be used to perform tendon repair.
5. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle before wound closure.
Cover the implant with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.
To avoid subluxation of the tendon after a paratendon approach, repair the tendon sheath.