Midaxial (lateral) approach to the proximal interphalangeal joint
1. Introduction
The midaxial approach, also known as lateral, gives access to the ipsilateral extensor mechanism, the distal condyle of the proximal phalanx, the base of the middle phalanx, the volar plate, and the associated ligaments.
The lateral approach does not give access to the opposite condyle, which in some situations is necessary, notably in irreducible bicondylar fractures.
Compared to a dorsal approach, only half of the dorsal aspect of the joint can be approached.
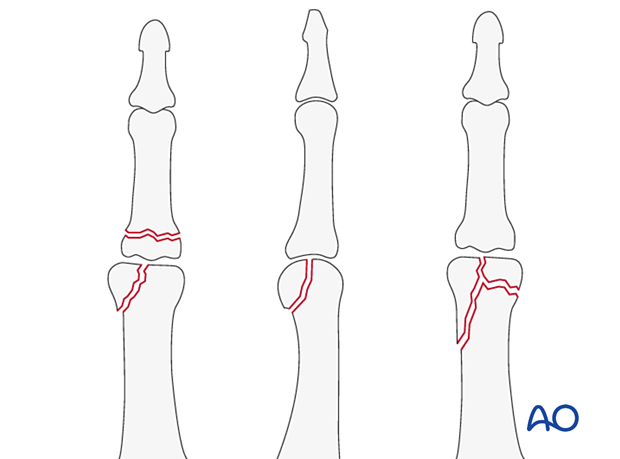
This approach is indicated for:
- Intra- or extraarticular basal fractures
- Condylar fractures
- Bicondylar fractures if the fracture morphology and choice of implant are optimal with the main fracture line
It is also used for irreducible dislocations with repair of the collateral ligament.
2. Surgical anatomy
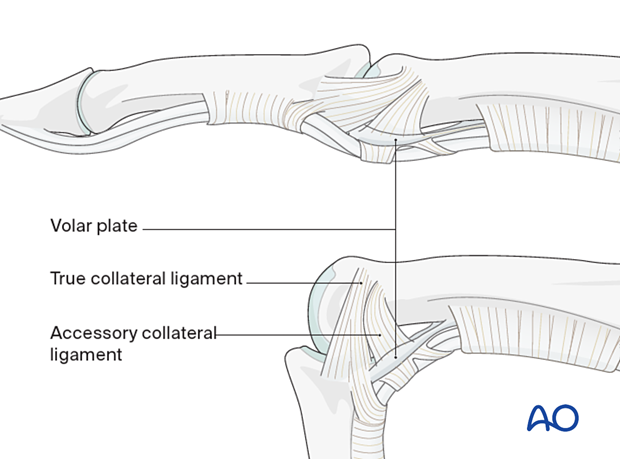
The interphalangeal joints are hinge joints. The heads of the proximal and middle phalanges each have two articular condyles that resemble a grooved trochlea and assist in preventing adduction/abduction and rotation in conjunction with the collateral ligaments.
Dynamic stability results from compressive forces, which increase during pinch and grip. Passive stability derives from the bone morphology and tension in the collateral ligaments and the volar plate. This passive stability is maximal in full extension.
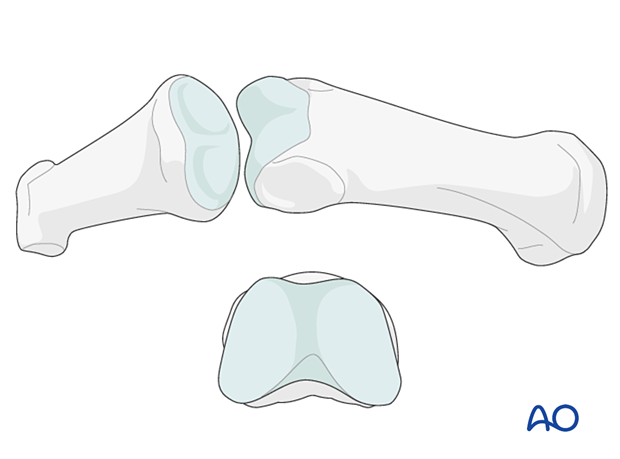
The two collateral ligaments and the volar plate are the primary structures stabilizing the interphalangeal joints and preventing displacement in the coronal plane (abduction/adduction).
The collateral ligaments also prevent side-to-side translational displacement.
The accessory collateral ligaments slacken in flexion, while the true collateral ligament is further tensioned in flexion due to the greater palmar width of the condyles.
When using a lateral approach, avoiding injury to these structures is mandatory.
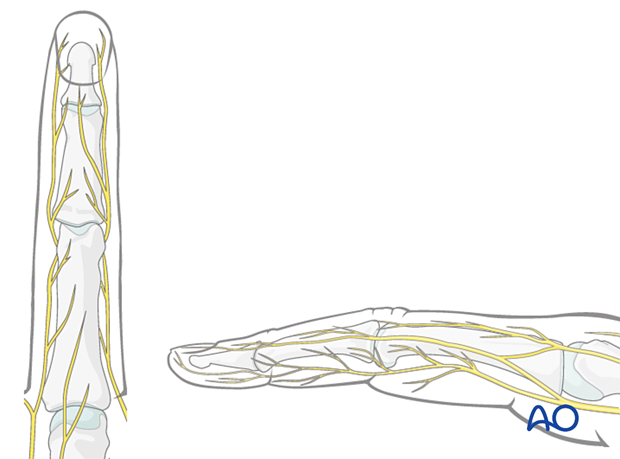
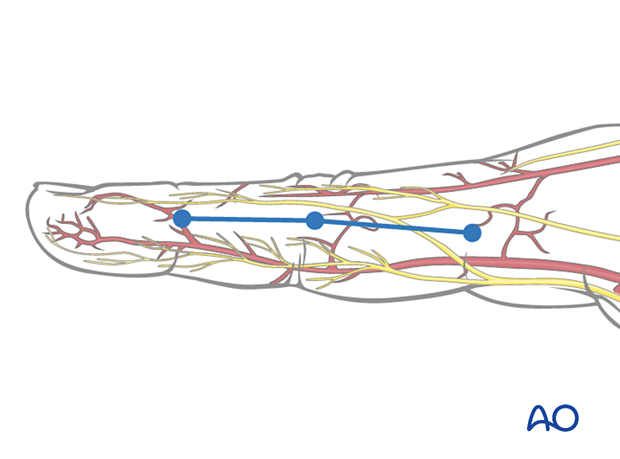
Nerve identification
In the thin subcutaneous tissue, identify and protect the dorsal sensory branches of the radial and ulnar nerves.
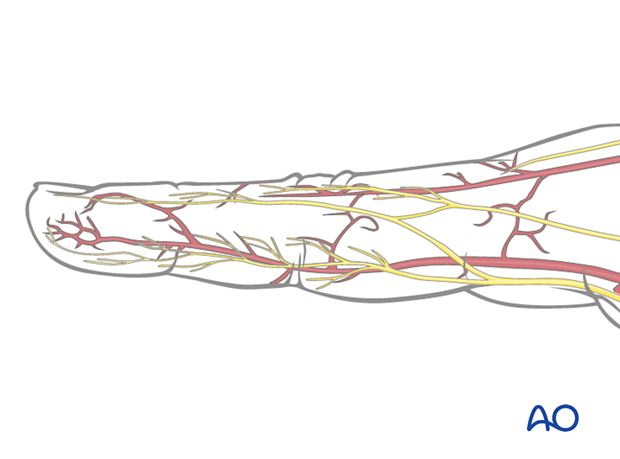
Identification of vascular structures
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized, but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
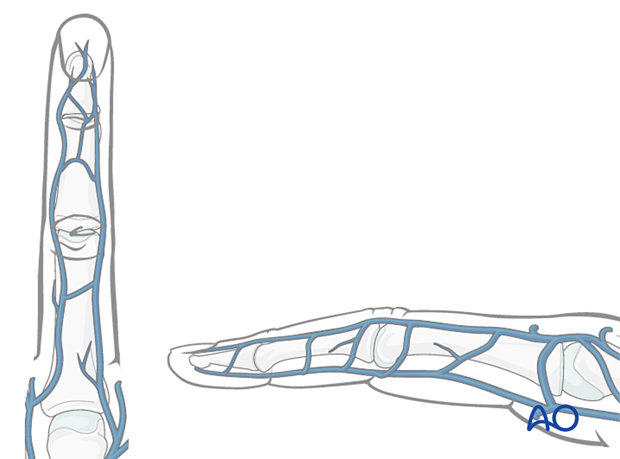
The digital artery and nerve lie palmar to the midaxial line in collateral relation with the flexor tendon sheath.
Preservation of soft-tissue structures
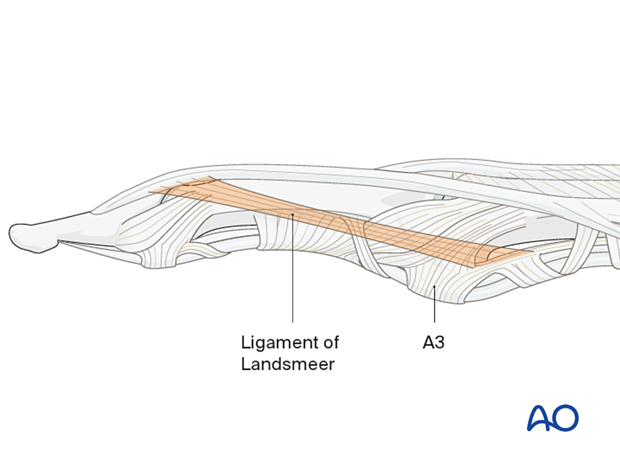
The oblique retinacular ligaments of Landsmeer pass obliquely from the palmar aspect at the attachment of the A3 pulley to the terminal conjoint extensor tendon on each side of the finger.
If it proves necessary to divide these ligaments, they must be repaired carefully to avoid dislocation of the extensor tendon.
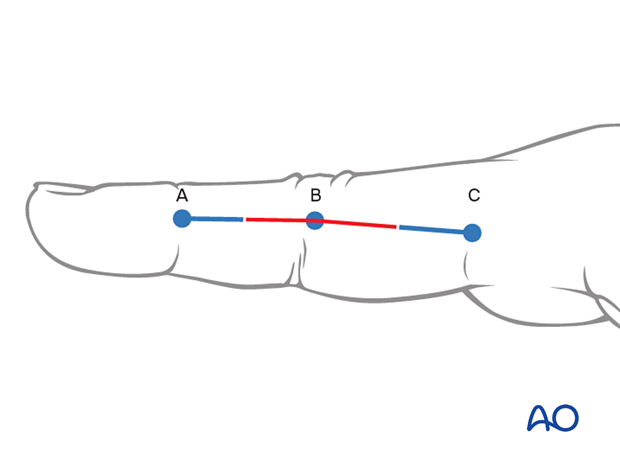
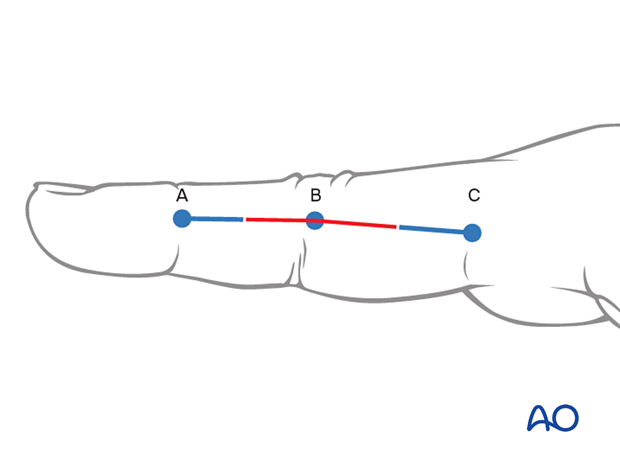
3. Skin incision
To plan the incision line, fully flex the finger as shown and mark the dorsal ends of the flexor creases with dots.
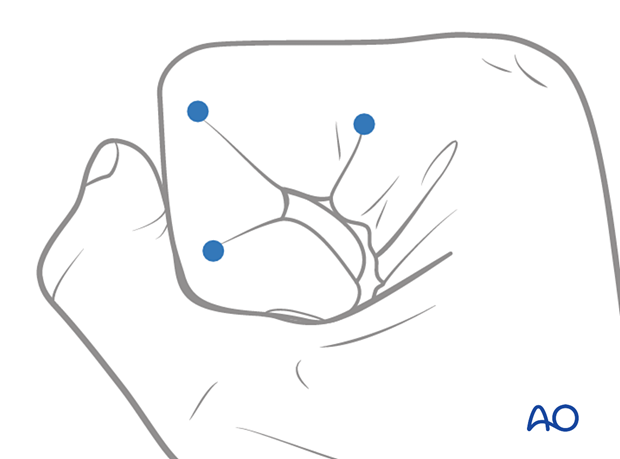
Extend the finger and connect the dots in a line.
The resulting line is safe for a midaxial skin incision. The digital artery and digital nerve will lie palmar to this line.
Perform a skin incision from the middle point between A and B to the middle between B and C.
A limited approach using only this short part of the incision line may be used as an adjunct to percutaneous fixation techniques.
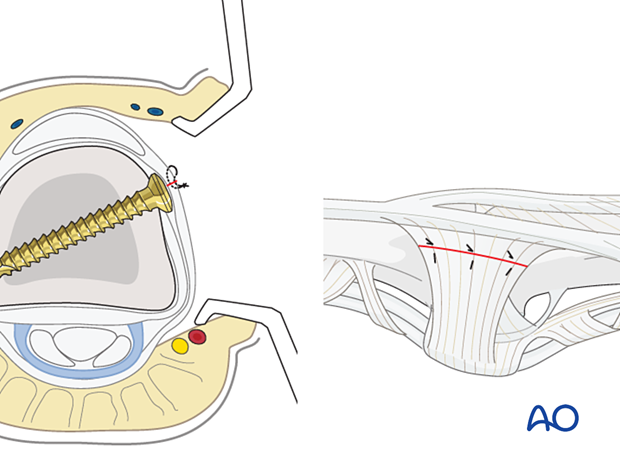
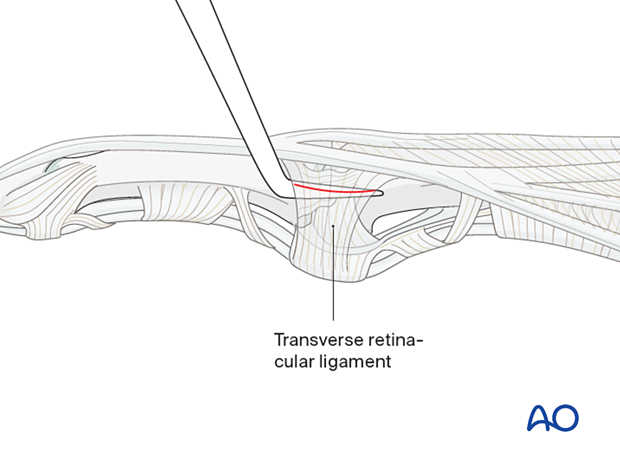
4. Division of the transverse retinacular ligament
To avoid accidentally cutting the collateral ligament, insert a dental pick between it and the transverse retinacular ligament (TRL).
The TRL can now be divided safely by cutting onto the dental pick.
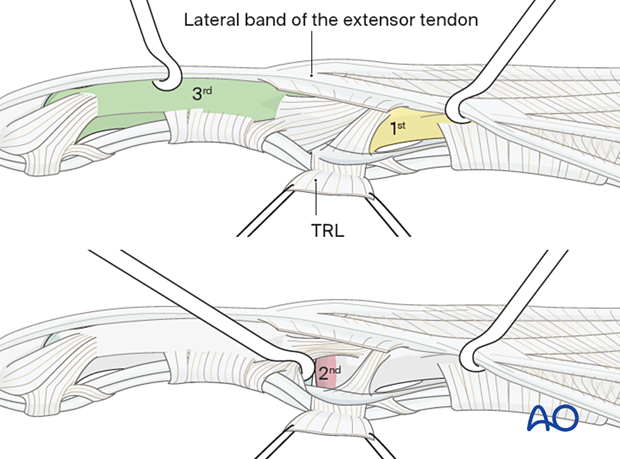
Retract the dorsal fringe of the TRL dorsally with the lateral band of the extensor tendon to expose the collateral ligament. Retract the palmar remainder of the TRL in a palmar direction using two fine sutures.
Three windows can then be developed:
- The first window is proximal to the collateral ligaments (shown in yellow), allowing exposure of the distal of the proximal phalangeal diaphysis.
- There is a small intermediate window between the true collateral and the accessory ligaments (shown in red). This is likely necessary to approach and stabilize certain small articular fragments.
- The 3rd window (shown in green) is distal to the collateral ligaments, allowing exposure to the middle phalangeal shaft.
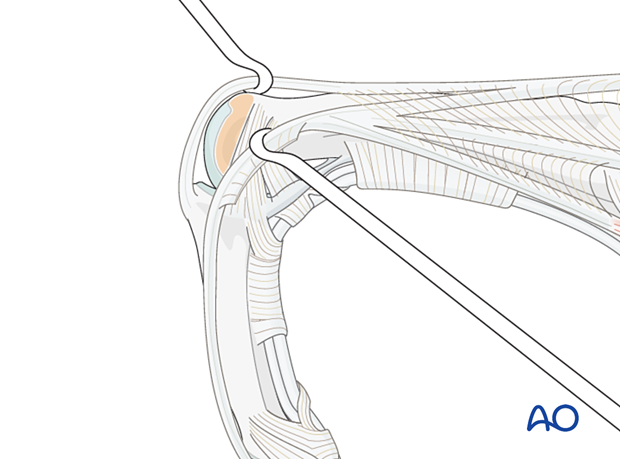
Alternative articular window
A further window can be created by flexing the proximal interphalangeal (PIP) joint and developing the interval between the central and lateral slips of the extensor apparatus. A longitudinal capsulotomy can then be made to inspect the joint.
5. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle before wound closure.
Cover the implant with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.
Repair the TRL with multiple fine mattress sutures before closing the skin.