Minicondylar bridge plate fixation
1. Principles
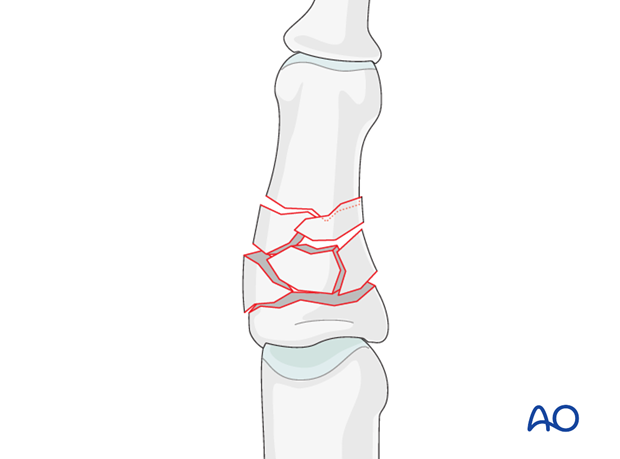
Comminuted fractures
Comminuted fractures are rarely isolated injuries, as they usually result from high-energy trauma (crushing). Soft-tissue lesions are frequently associated with the potential risk of edema, fibrotic reactions and eventual stiffness.
For these reasons, these injuries are usually treated by ORIF, in order to provide sufficient stability for immediate mobilization, reducing the risk of joint stiffness and tendon adhesions.
Even in the hand, which is well vascularized, small fragment comminution means poor soft-tissue attachment to the fragments and, thereby, compromised vascularity.
2. Approach
For this procedure a midaxial approach to the middle phalanx is normally used.

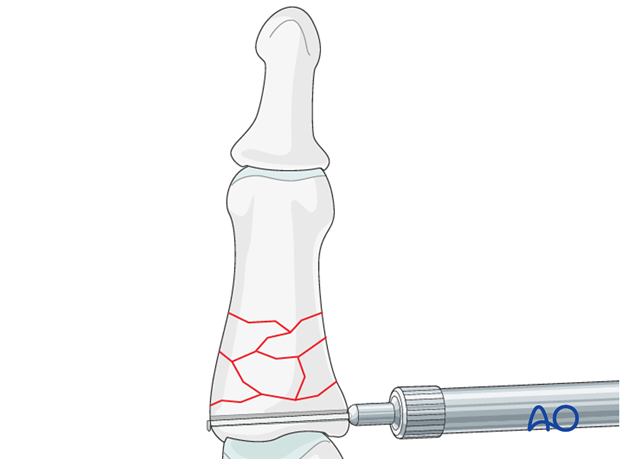
3. Reduction
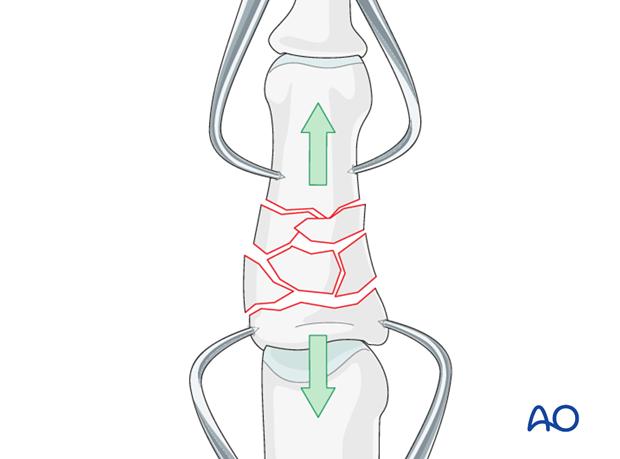
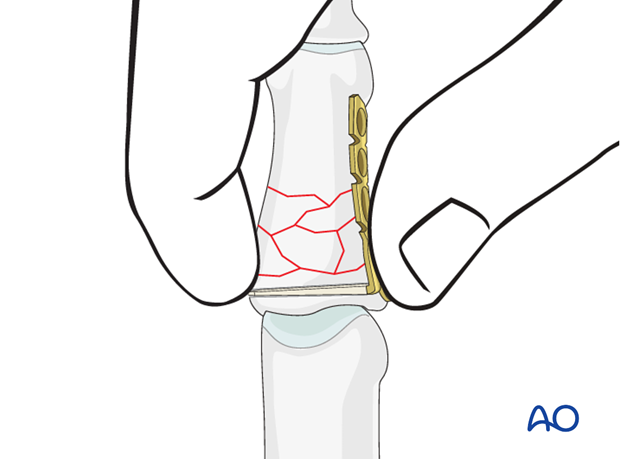
Indirect reduction by traction
Reduction can be achieved by traction and flexion exerted manually,...
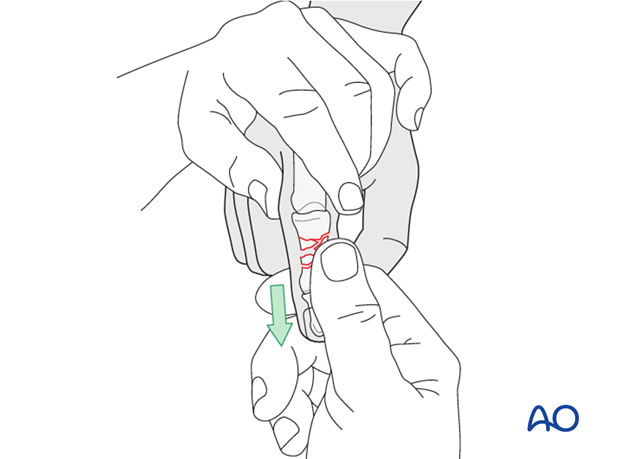
...or using two forceps.
Confirm reduction using image intensification.
4. Drilling
In order to determine the position of the first drill hole, it can be very helpful to turn the plate over and use it as a template.
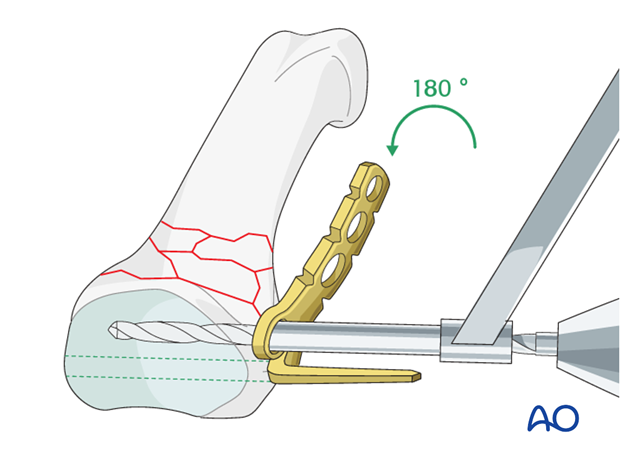
Drill a 1.5 mm transverse hole through the base of the middle phalanx adjacent to the joint surface as a track for the blade of the plate.
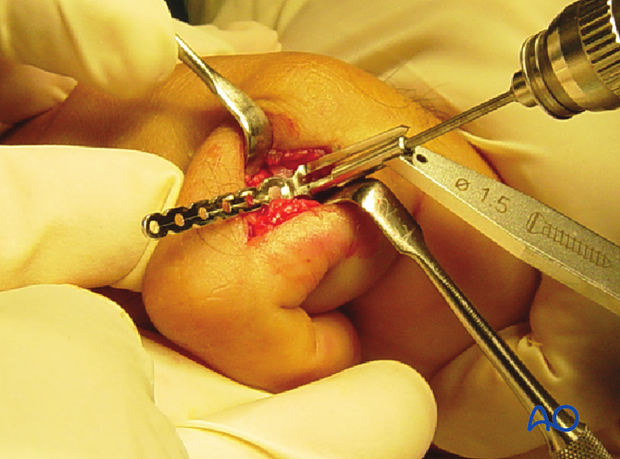
The drill hole needs to be dorsal enough as to leave enough space for the plate’s most proximal screw hole.
5. Preparation
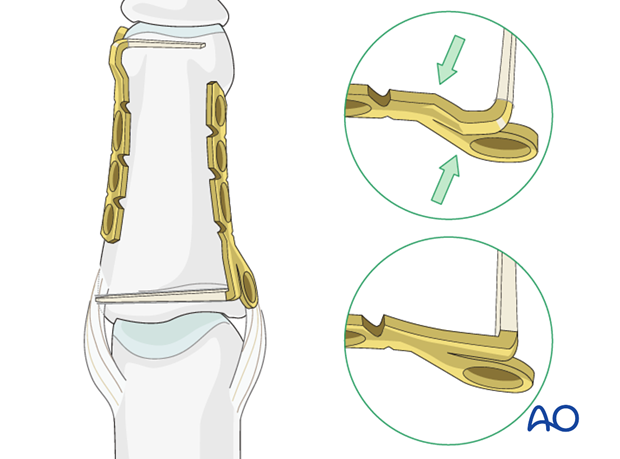
Prepare the blade
Measure the length of the drill hole using a measuring device.
Cut the blade to the determined length, so that it just fills the drill hole.
Pitfall
Avoid protrusion from the opposite cortex, as friction during movement and eventual ligament injury may result.
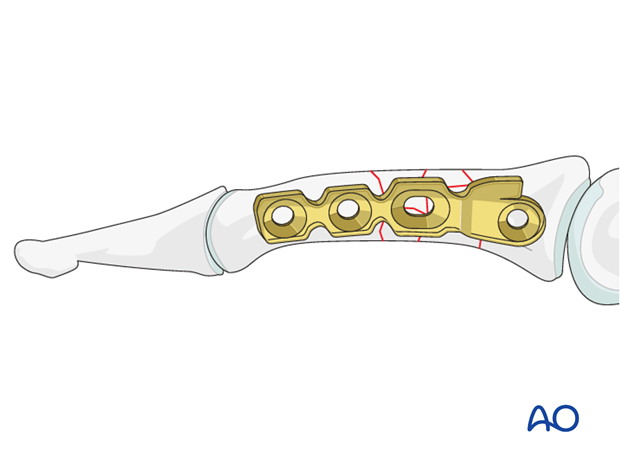
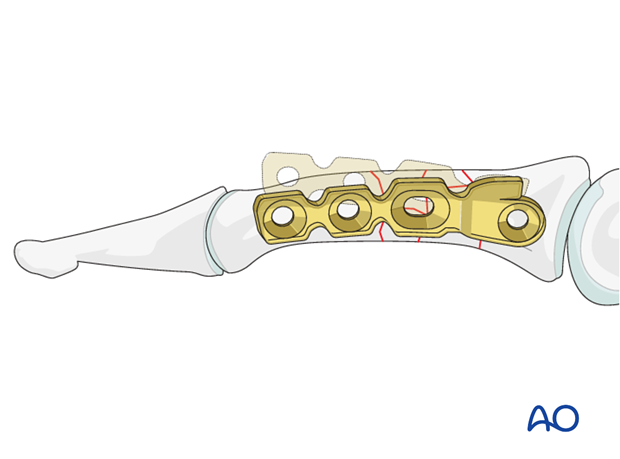
Trim the plate
Adapt the plate length to fit the length of the proximal phalanx. Avoid sharp edges which may be injurious to the tendons. There should be at least 3 plate holes distal to the fracture available for fixation in the diaphysis. At least two screws need to be inserted into the diaphysis.
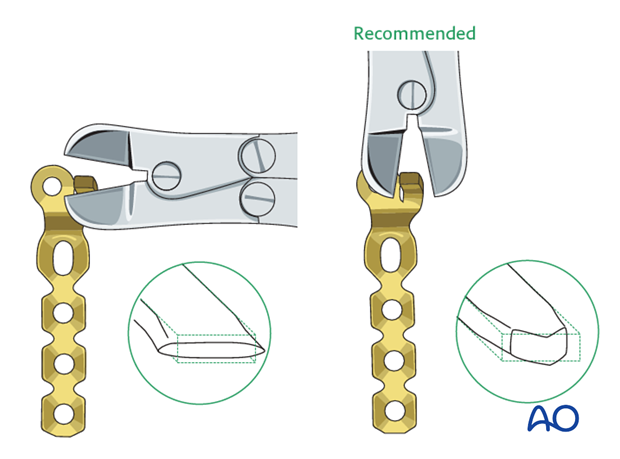
Pearl: Cut the blade transversely
If you cut the blade on the flat, it will compress and widen very slightly as it is cut. This makes its maximal width very slightly larger than 1.5 mm. It may not fit in the 1.5 mm hole that you have drilled.
Therefore, cut the blade on edge (to deform it through its narrower dimension) to the correct length. The resultant tip is somewhat arrow-shaped.
Contouring of the plate
Use pliers to contour the plate so that it fits exactly the anatomy of the base of the proximal phalanx.
The plate was designed for condylar fractures and is precontoured to fit around a condyle. It has to be adapted for the less curved shape of the base of the proximal phalanx.
6. Fixation
Plate application
Introduce the blade into the drill hole. Gently push with the thumb until the plate is fully seated.
Align the plate with the diaphysis
Before inserting the first (distal) screw, ensure that the plate is in line with the phalangeal diaphysis in the sagittal plane by rotating it around the axis of the blade.
Drill distal hole
Use a 1.1 mm drill bit to prepare the first neutral screw hole at the distal end of the plate.
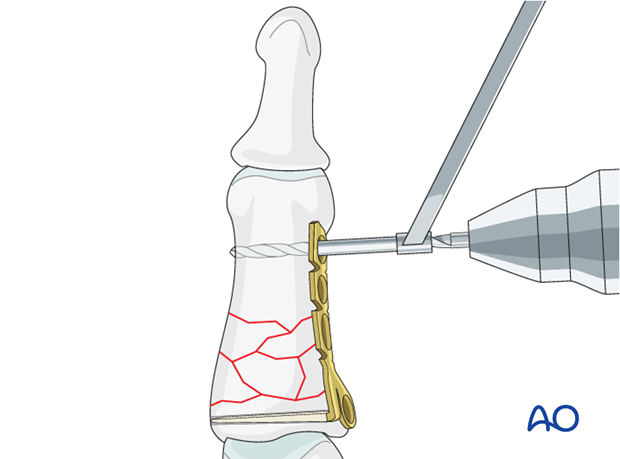
Insert screw
Measure for screw length and insert a self-tapping 1.5 mm screw.
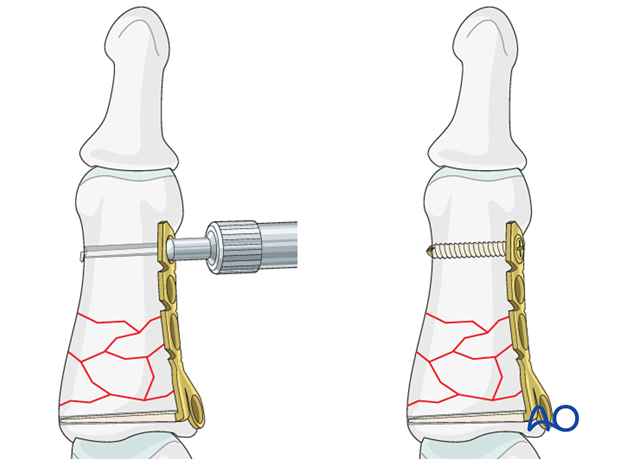
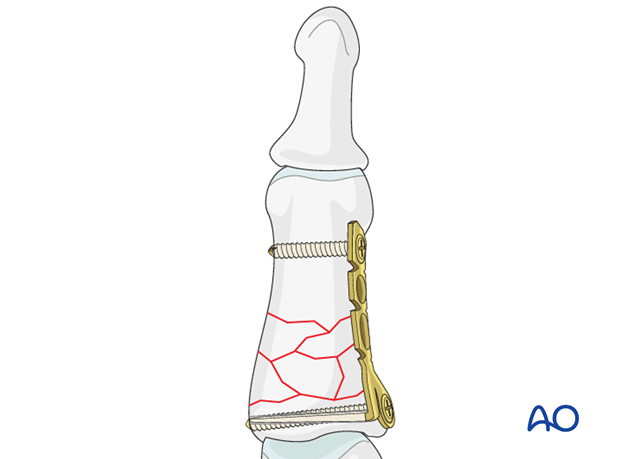
Insert proximal screw
The proximal screw is inserted next, in the same fashion.
The screws should just engage the far cortex. This proximal screw functions as a position screw only.
Do not exert compression through this screw, as this may compromise the reduction of the comminuted zone.
Note
Be careful to avoid protrusion of the proximal screw through the far (trans) cortex, as ligament injury may result from friction during movement.
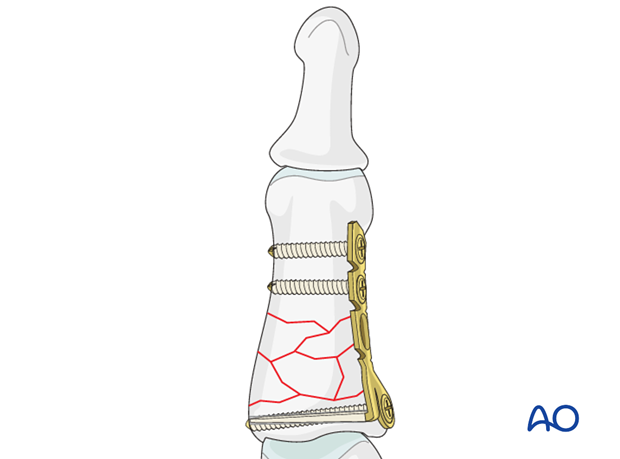
Finalize fixation
Insert a further screw into one of the diaphyseal holes in a neutral position.
7. Aftertreatment
Postoperatively
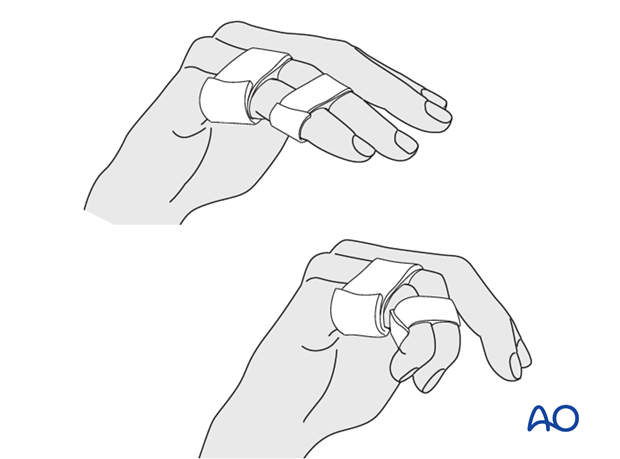
Protect the digit with buddy strapping to the adjacent finger, to neutralize lateral forces on the finger.
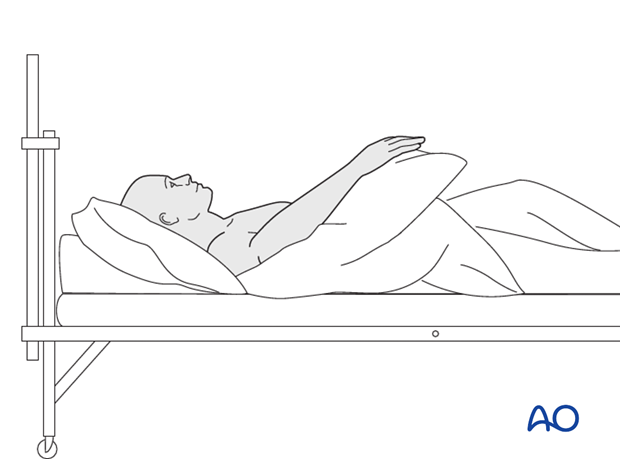
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
Follow up
See the patient 5 days and 10 days after surgery.
Functional exercises
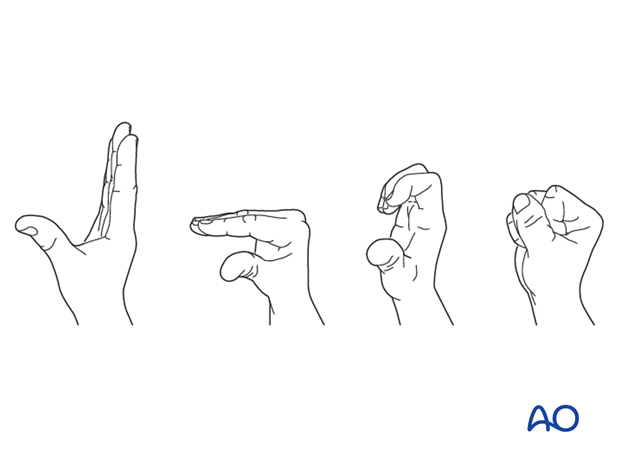
The patient can begin active motion (flexion and extension) immediately after surgery.
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.












