Nonoperative treatment
1. General considerations
Indications
Stable volar plate avulsions, multifragmentary metaphyseal and diaphyseal fractures may be treated with a dorsal splint to avoid overextension of the proximal interphalangeal (PIP) joint. Some stable distal complete articular fractures may be treated in the same way.
The dorsal splint allows immediate active mobilization (flexion) of the finger joints.
Irreducible rotational malalignment is an indication for operative treatment.
Hand position for splinting
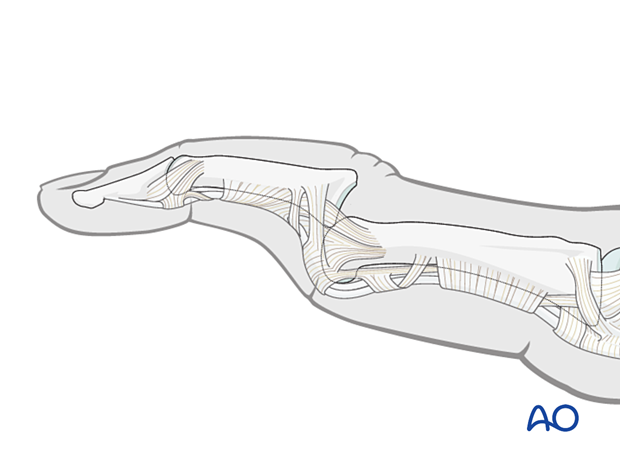
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- Metacarpophalangeal (MCP) joint in 90° flexion
- Proximal interphalangeal (PIP) joint in extension
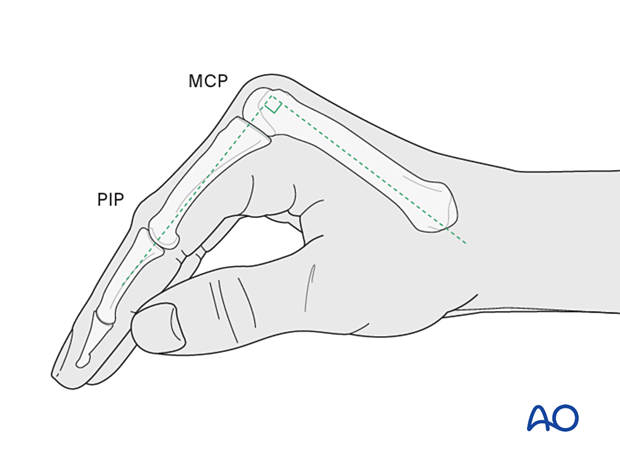
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
AO Teaching video
Phalanx - Proximal Fractures - Extension Block Splint (Burke Halter)
2. Reduction of dislocation
Closed reduction
Dislocation usually presents as an extension displacement with dorsal deformity.
This can be reduced by increasing the deformity with gentle dorsally applied pressure on the middle phalanx to reduce the joint. This keeps the palmar structures in tension and reduced the risk of soft-tissue interposition.
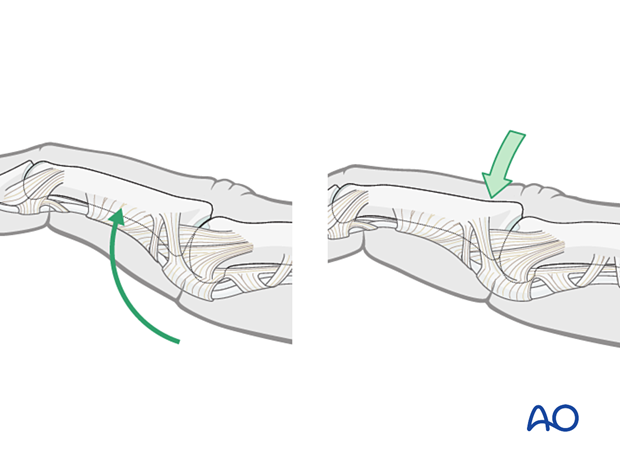
Stability evaluation
Confirm reduction with an image intensifier and check the joint stability by active flexion and extension. This should show congruent movement compared with the adjacent joints.
If this is the case, no further operative treatment is necessary.
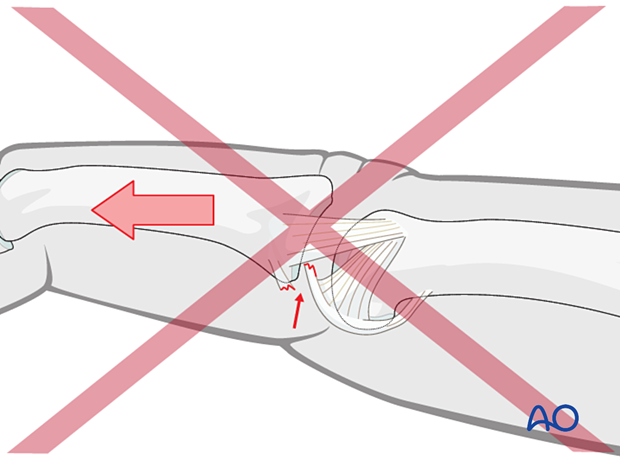
Open reduction
If congruent reduction can not be achieved, often due to interposed soft tissue, an open reduction is necessary.
In this case, consider surgical treatment of the fracture.
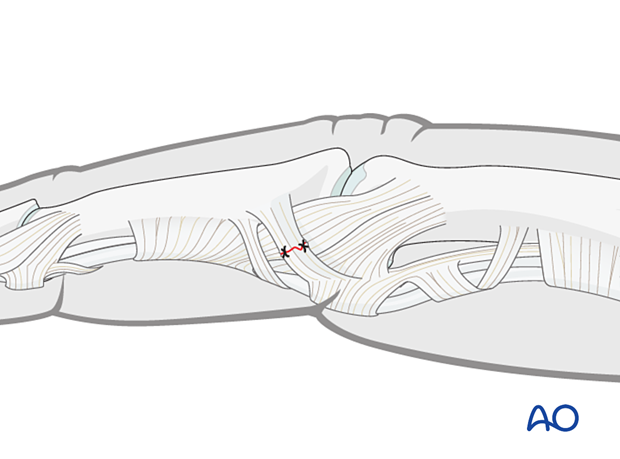
3. Ligament repair
If there is insufficient PIP joint stability, surgical repair of the collateral ligaments and the extensor mechanism may be required. In some cases, surgical repair of the volar plate may be indicated.
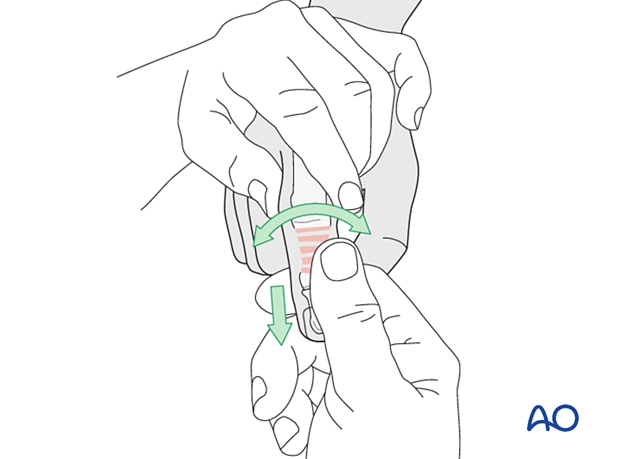
4. Fracture reduction
Displacement usually occurs as an extension deformity.
Reduction is achieved by applying longitudinal traction and extension to the finger.
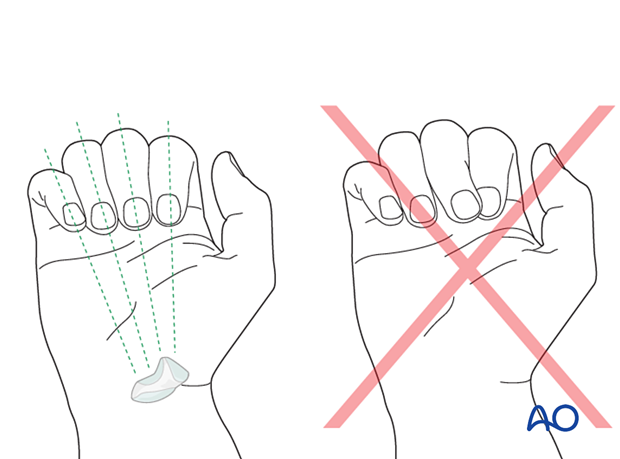
Rotational malalignment should be corrected.
Any angular deviation can be checked by comparison with the adjacent fingers and must be reduced.
Check the reduction with an image intensifier.
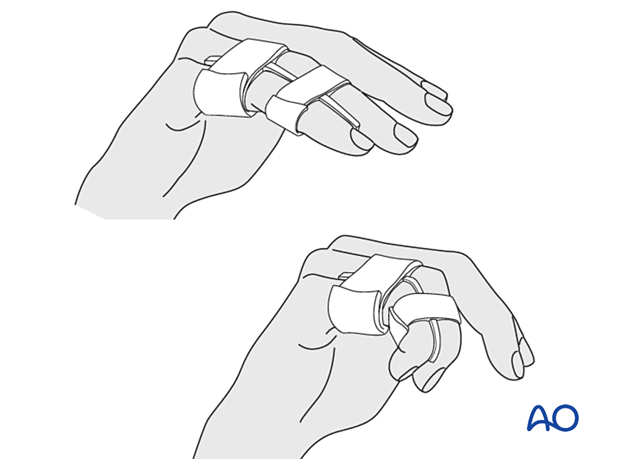
5. Buddy strapping
Strap the injured finger to a neighboring finger.
The strapping should leave the joints free for mobilization.
Direct skin contact with adjacent fingers should be prevented by placing gauze pads between them.
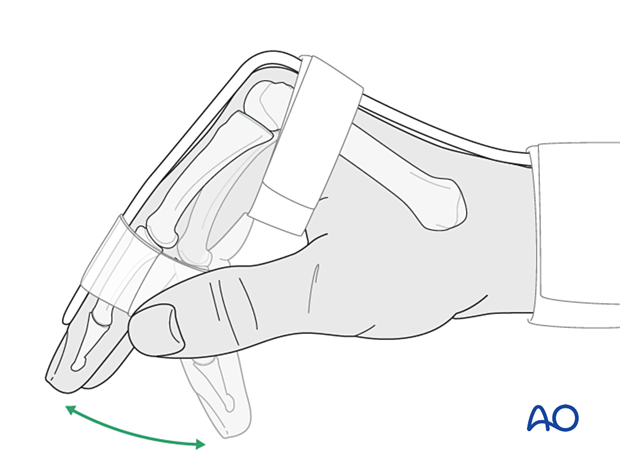
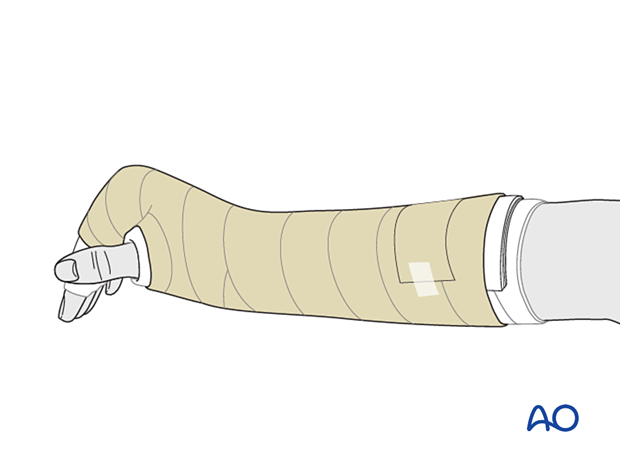
6. Splint application
Protect the skin of the arm and hand with padding/cotton sleeve to avoid pressure sores, especially on the distal ulna and styloid process of the radius.
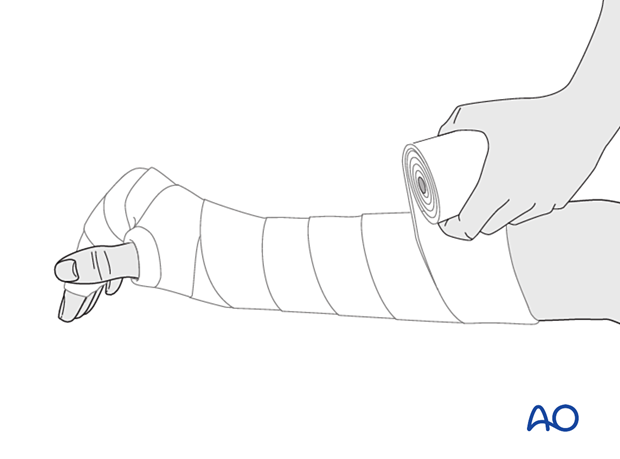
In compliant patients, only the affected and the directly neighboring fingers may be included in the splint.
Create a splint of at least 6 slabs of cast bandage. It should cover the dorsal or palmar half of the forearm, wrist, and hand.
The wrist should be in neutral or up to 15° extension.
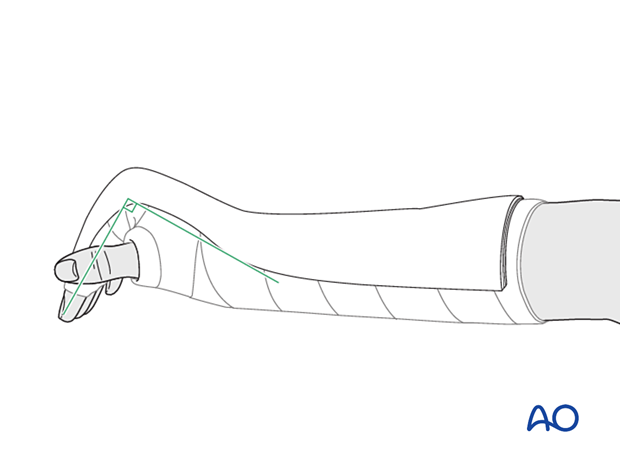
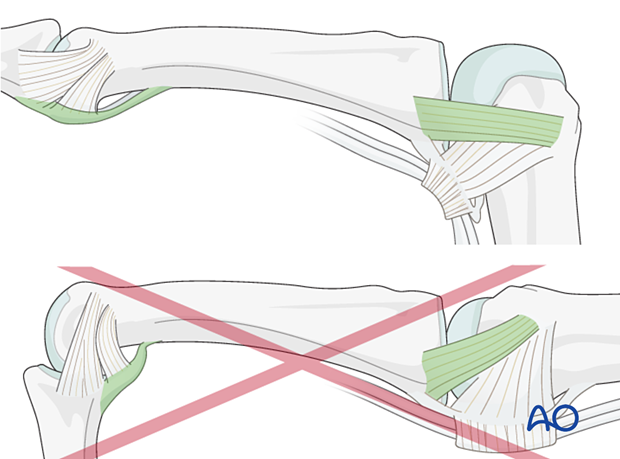
The splint is held in place with an elastic bandage. The bandage should not be overtightened at the level of the wrist joint to avoid excessive swelling of the hand.
Direct skin contact with adjacent fingers should be prevented by placing gauze pads between them.
In a dorsal splint, buddy strap the injured finger to an adjacent finger.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
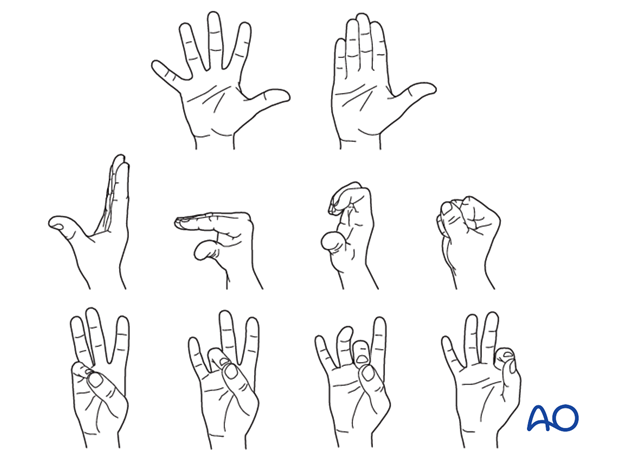
Mobilization
Active mobilization can be started early while supported by the splint. Functional exercises are recommended.
Follow-up
X-ray checks of joint position must be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week and, if necessary, after 2 weeks. A final x-ray can be taken at the expected fracture consolidation.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
Immobilization is continued until about 4–6 weeks after the injury. At that time, an x-ray may be taken to confirm healing, and range of motion should be pain-free. Buddy strapping is continued for another 2 weeks.
A palmar thermoplastic night splint, with the PIP joint in full extension, is used to avoid flexion contraction.
In the absence of pain during functional activities, full manual loading can be permitted. In case of doubt, an x-ray to confirm healing and consolidation, which would be expected by 8 weeks, should be taken.













