Volar plate avulsion of the proximal end segment
Definition
Avulsions involving the articular surface of the base of the middle phalanx are partial articular fractures and classified according to AO/OTA as 78.2–5.2.1B, where 2–5 indicates which finger is injured. The fractures may be simple or fragmentary.
An avulsion fracture may be associated with a proximal interphalangeal (PIP) joint dislocation.
Injury types of volar plate avulsions
Avulsion fractures of the volar plate are very common injuries, often resulting from sporting injuries and usually involving the middle and ring fingers. Several classification systems have been proposed for them. The Eaton classification is useful and practical. Its premise is that successful treatment must be based on the stability of the fracture, which in turn depends on:
- Size of the fragment
- Degree of impaction
- Ruptures of one or both collateral ligaments
- Direction of the dislocation (palmar, lateral, or dorsal)
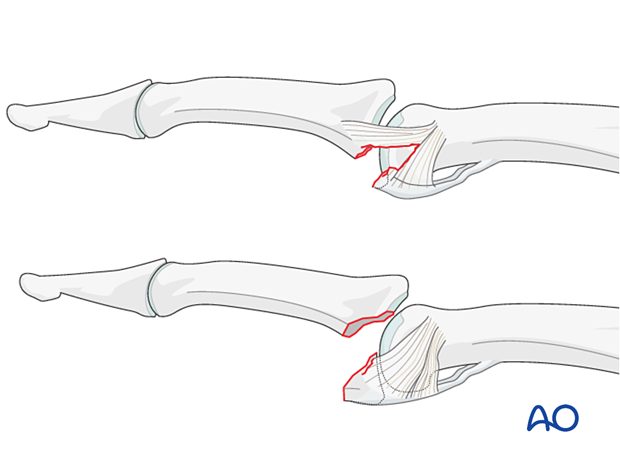
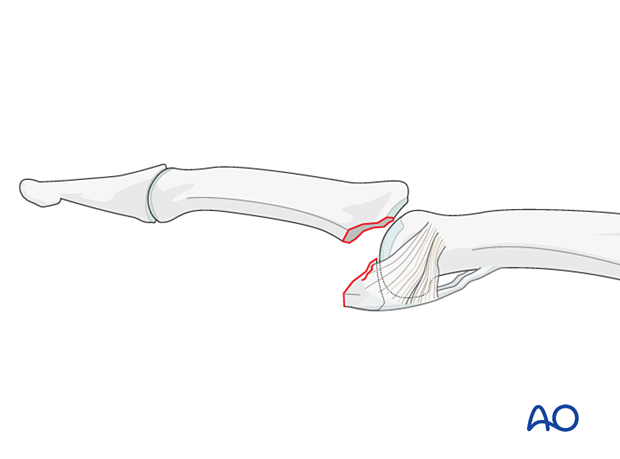
Eaton type I (hyperextension)
These are hyperextension injuries, with an avulsion of the volar plate and a longitudinal split in the collateral ligaments.
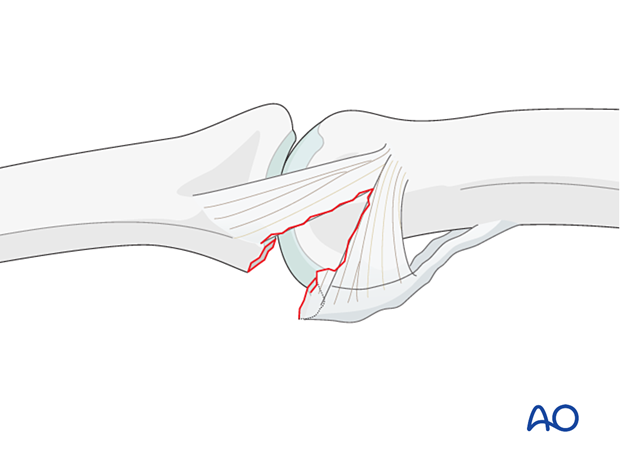
Eaton type II (dorsal dislocation)
Complete dorsal dislocation of the proximal interphalangeal (PIP) joint and avulsion of the volar plate. The base of the middle phalanx rests dorsally on the condyles of the proximal phalanx, with no contact between the articular surfaces.
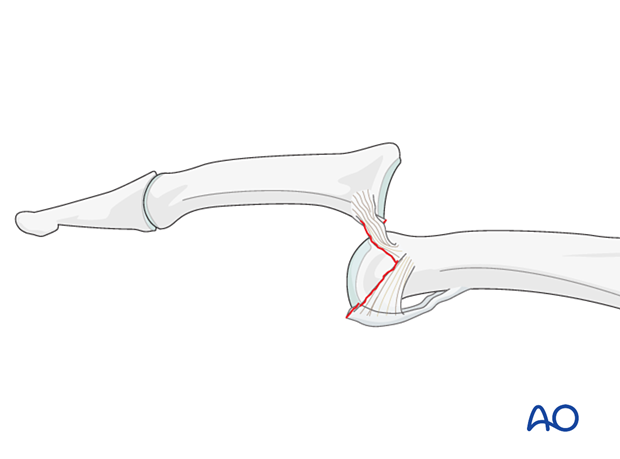
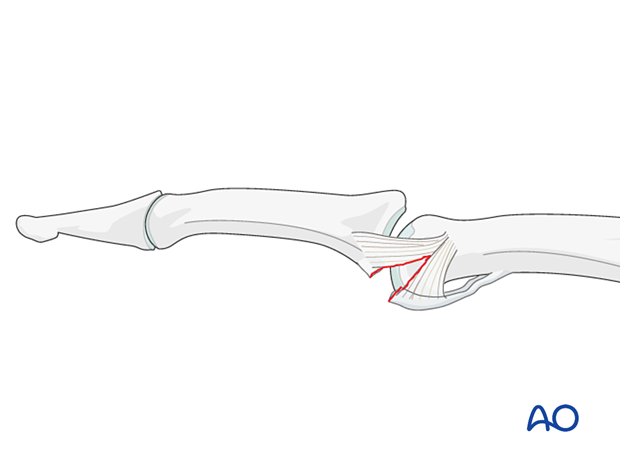
Eaton type III (fracture-dislocation)
A fracture dislocation with an avulsed small fragment.
Further characteristics
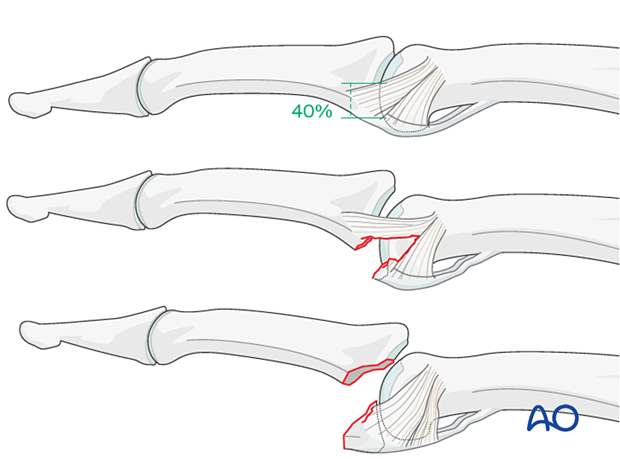
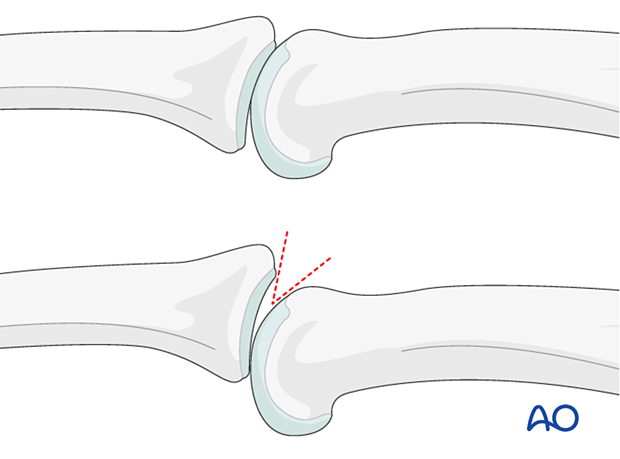
Stability of fracture-dislocations (Eaton type III)
Stability of the reduction depends on the size of the avulsed fragment and the amount of ligament remaining attached to the middle phalanx.
If less than 40% of the articular segment is avulsed, the fracture is displaced dorsally, with the dorsal portion of the collateral ligament remaining attached to the middle phalanx. This helps to keep the reduction stable.
However, if more than 40% of the articular segment has avulsed, only very little or no ligament will remain attached to the base of the middle phalanx, rendering the reduction unstable.
Irreducible fracture
When the avulsed fragment is very small (<30% of the articular segment), nonoperative treatment is usually a good choice.
In some cases, the fracture can not be reduced due to interposed tissues, or blood clot. In these cases, open reduction is required.
As the use of a lag screw could easily shatter such a small fragment, internal fixation with sutures is often chosen.
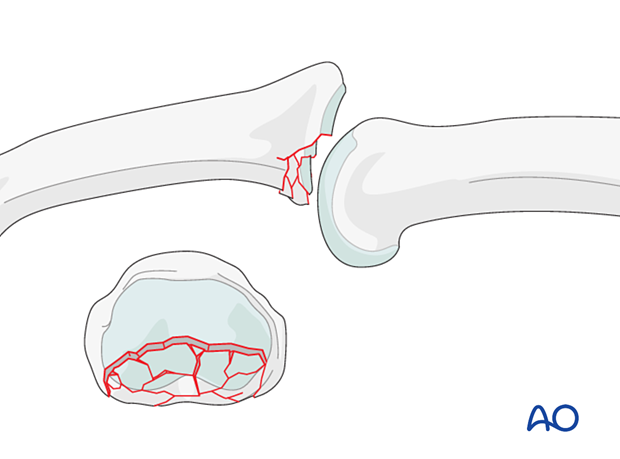
Impaction injuries
Impaction is possible both in the sagittal and the coronal planes. Check both true AP and lateral views. A CT scan should be considered.
For further information on impaction fractures, see the multifragmentary articular fracture type.
Recognizing subluxation
In the lateral view, the dorsal cortical profiles of the proximal and middle phalanges should be collinear. Any axial malalignment is a clear indication of subluxation.
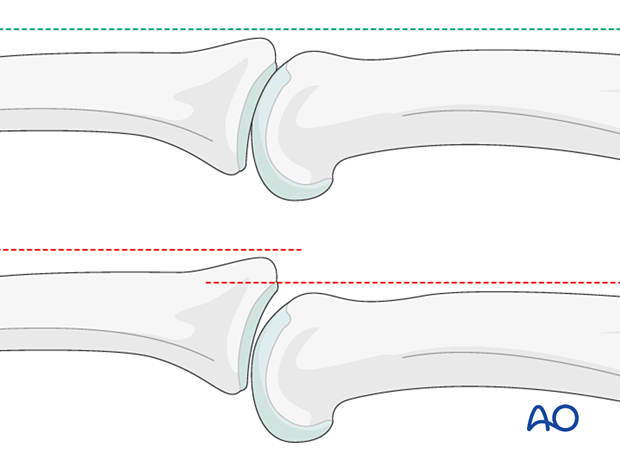
Another indication of subluxation is the presence of a so-called V-sign in the lateral x-ray.
Imaging
X-ray
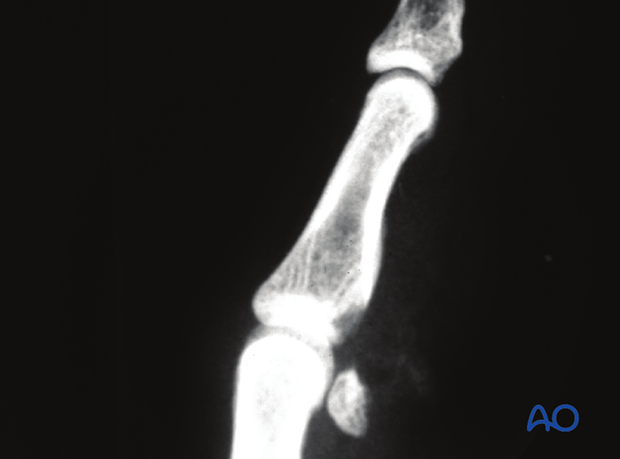
This lateral x-ray shows a volar plate avulsion.
The partial articular fragment of the middle phalangeal base has displaced and is rotated.
These AP and lateral x-rays show a small avulsion fracture of the volar plate with dorsal dislocation of the PIP joint.
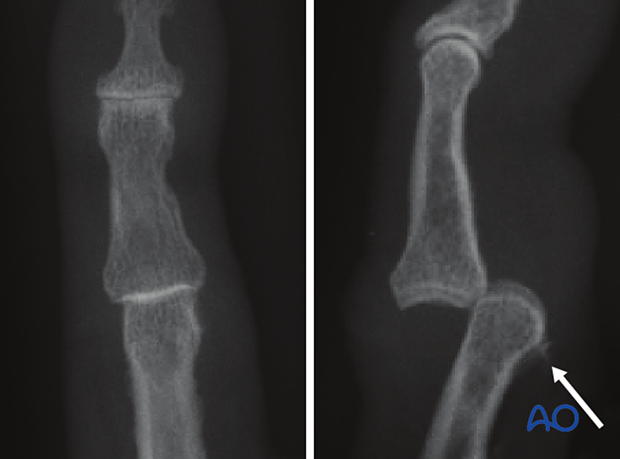
These lateral views show a PIP joint dislocation before and after reduction.
In the right image, the small bony avulsion fragments suggest avulsion of the flexor tendon attachment and a substantial ligament rupture.

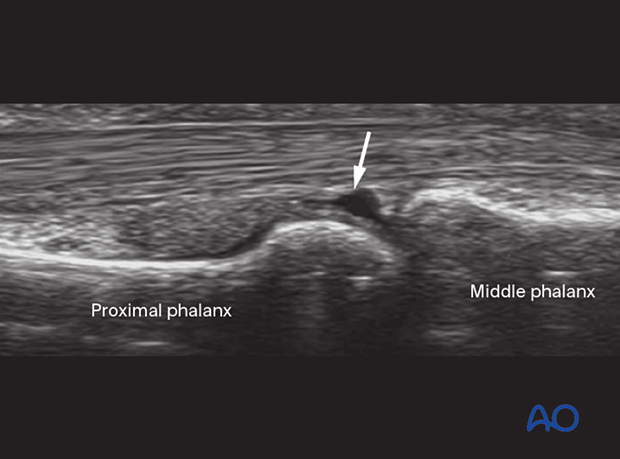
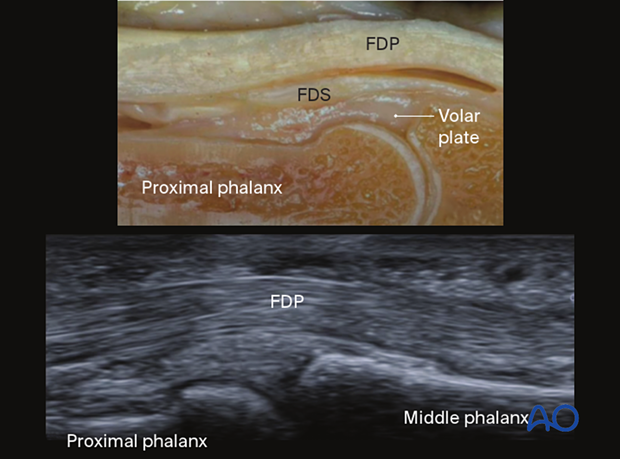
Ultrasound
In these images of an anatomical specimen and ultrasound of an intact volar plate, the flexor digitorum profundus (FDP) and superficialis (FDS) are labelled.
This ultrasound shows avulsion with partial rupture of the volar plate. The rupture site is indicated with an arrow.