Dynamic external fixation
1. General considerations
In its various forms, the dynamic external fixation is readily available, can be easily applied, and allows for early mobilization of the joint in cases of unreconstructible articular fractures.
It may also be added temporarily for protect internally fixed articular fractures during the healing process.
Additionally, periarticular dynamic fixation can be used to reduce compressive load to the articular surface through arthrodiastasis (ligamentotaxis).
The advantage of this device is the early controlled mobilization by the patient to regain function of the finger.
In this procedure, the application of the Suzuki type fixator frame is shown.
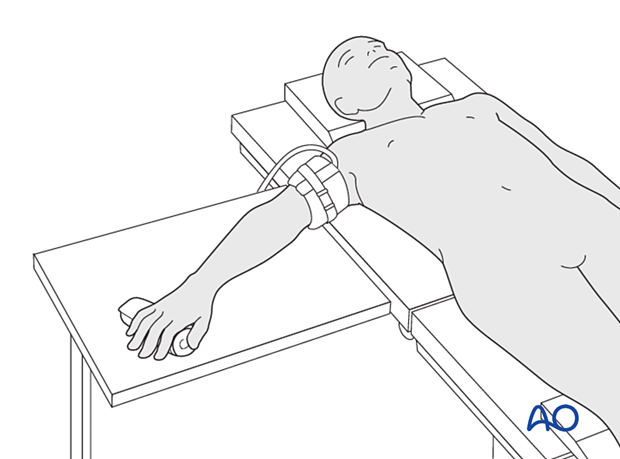
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
The application of a dynamic external fixator requires an image intensifier.
The procedure is recommended to be performed with the patient awake with local anesthesia (WALANT) to check the active motion.
3. Reduction
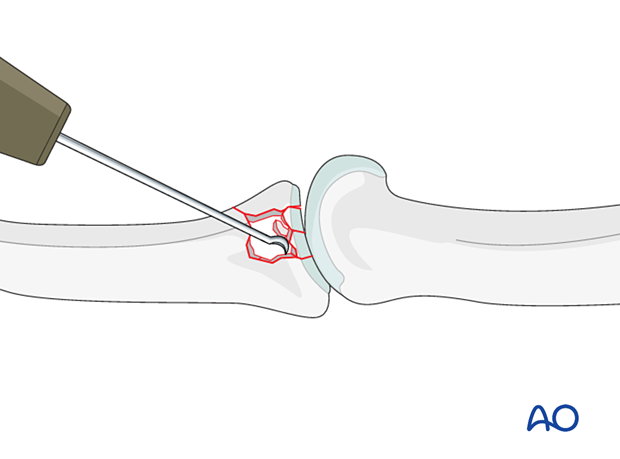
Reduction of the depressed articular fragments
Compression fractures are not reducible by ligamentotaxis, as the centrally impacted fragments are devoid of soft-tissue attachments.
Direct reduction is thus necessary.
The key to fixing compression fractures is restoring the joint surface to as close to normal as possible (anatomically) and supporting the reduction with bone graft if needed.
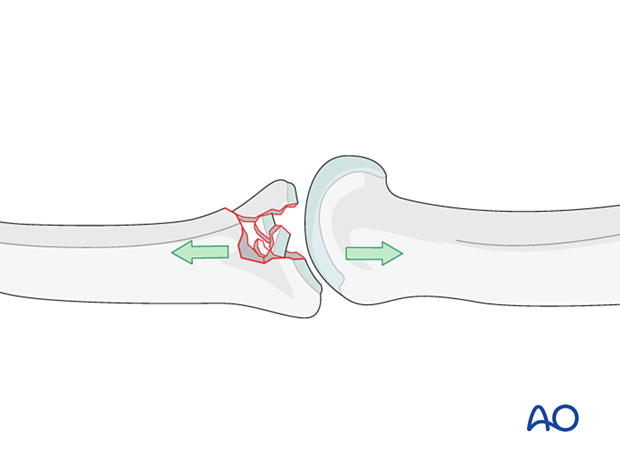
Use a K-wire, a dental pick, or a small curette to push the depressed fragments towards the head of the proximal phalanx, which should be used as a template to restore congruity of the articular surface of the middle phalanx to reduce the risk of later degenerative joint disease.
If a cartilage step-off remains, degenerative joint disease is likely to follow.
Optionally, for reduction, a K-wire may be inserted through the shaft and the medullary canal up to the subchondral region.
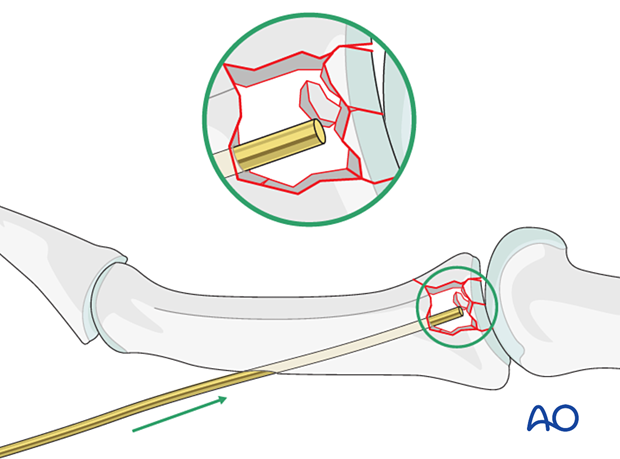
Stabilization of articular fragments
Optionally, to maintain joint surface congruity, insert K-wires preferably from dorsal to palmar to stabilize the reduction of the articular fragments. These can be left until fracture consolidation.
4. Application of the fixator
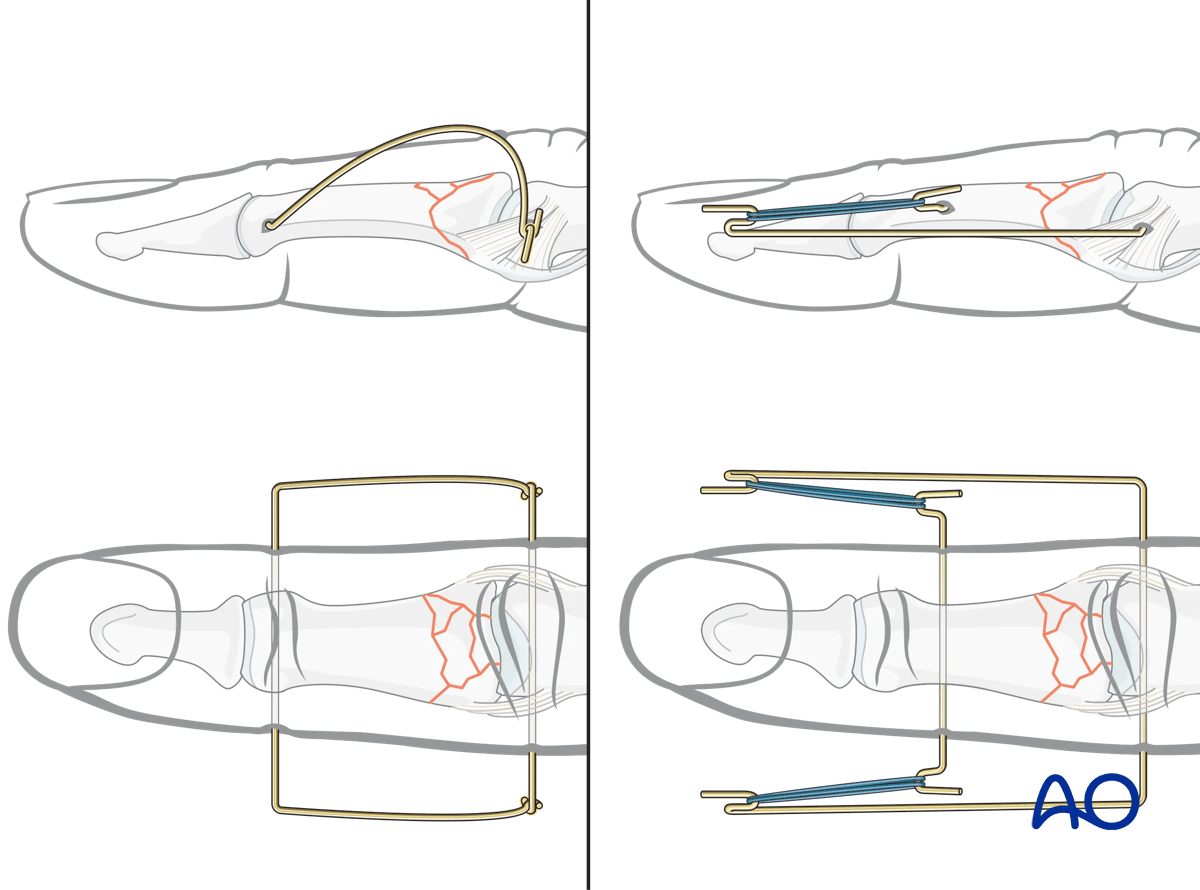
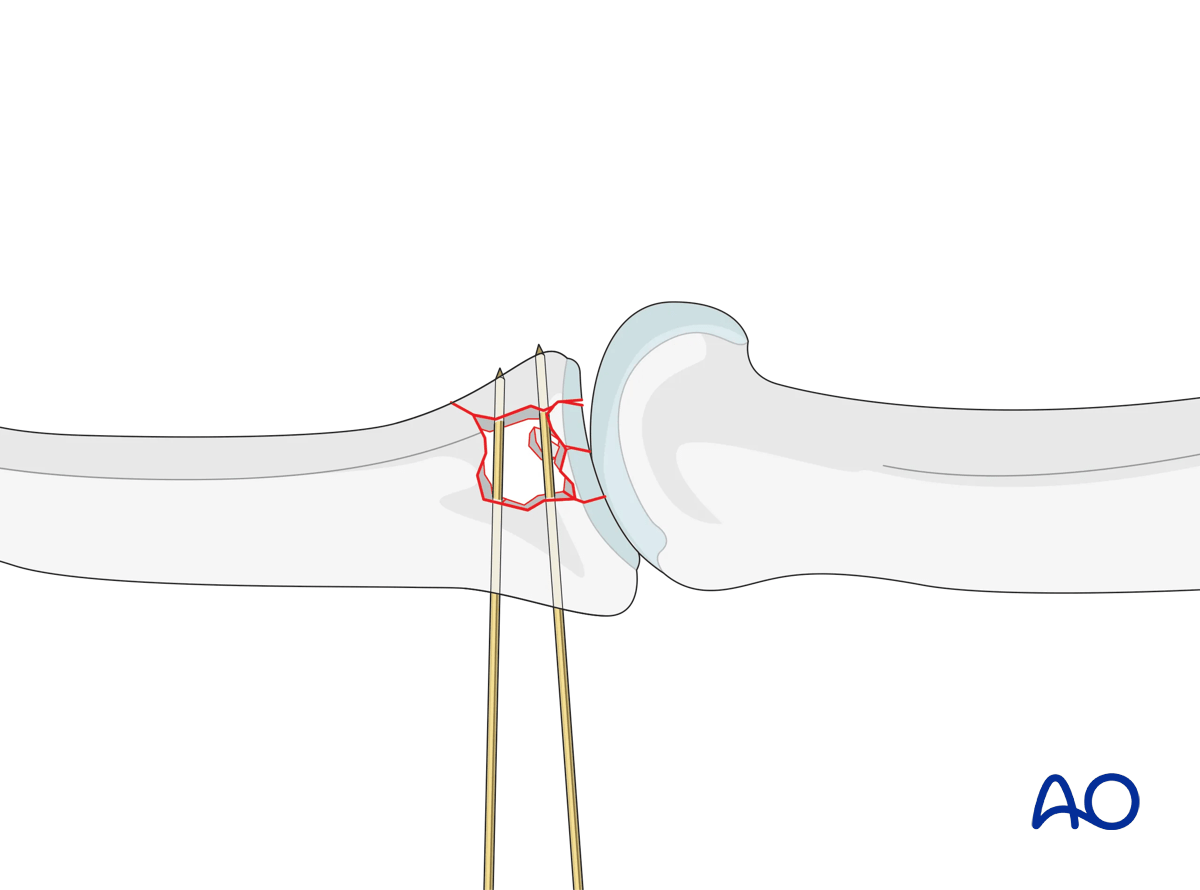
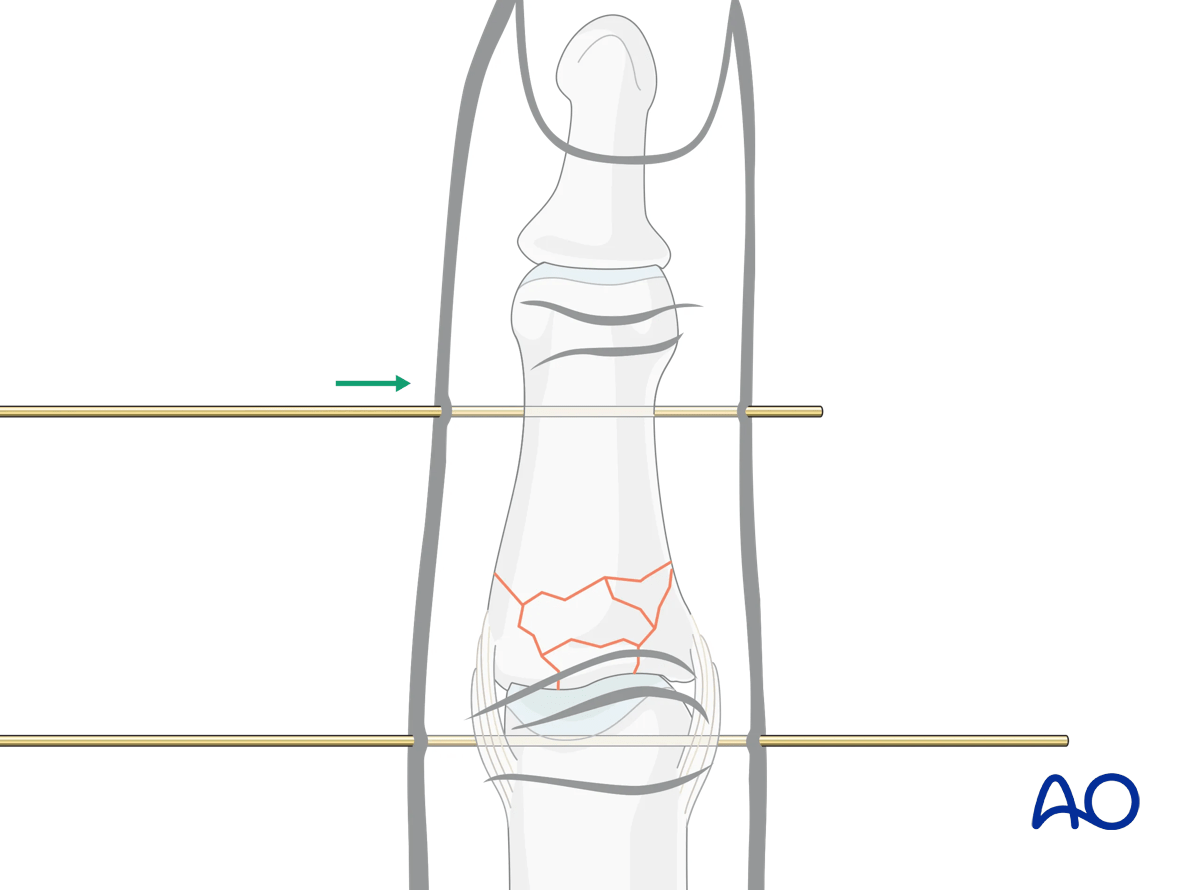
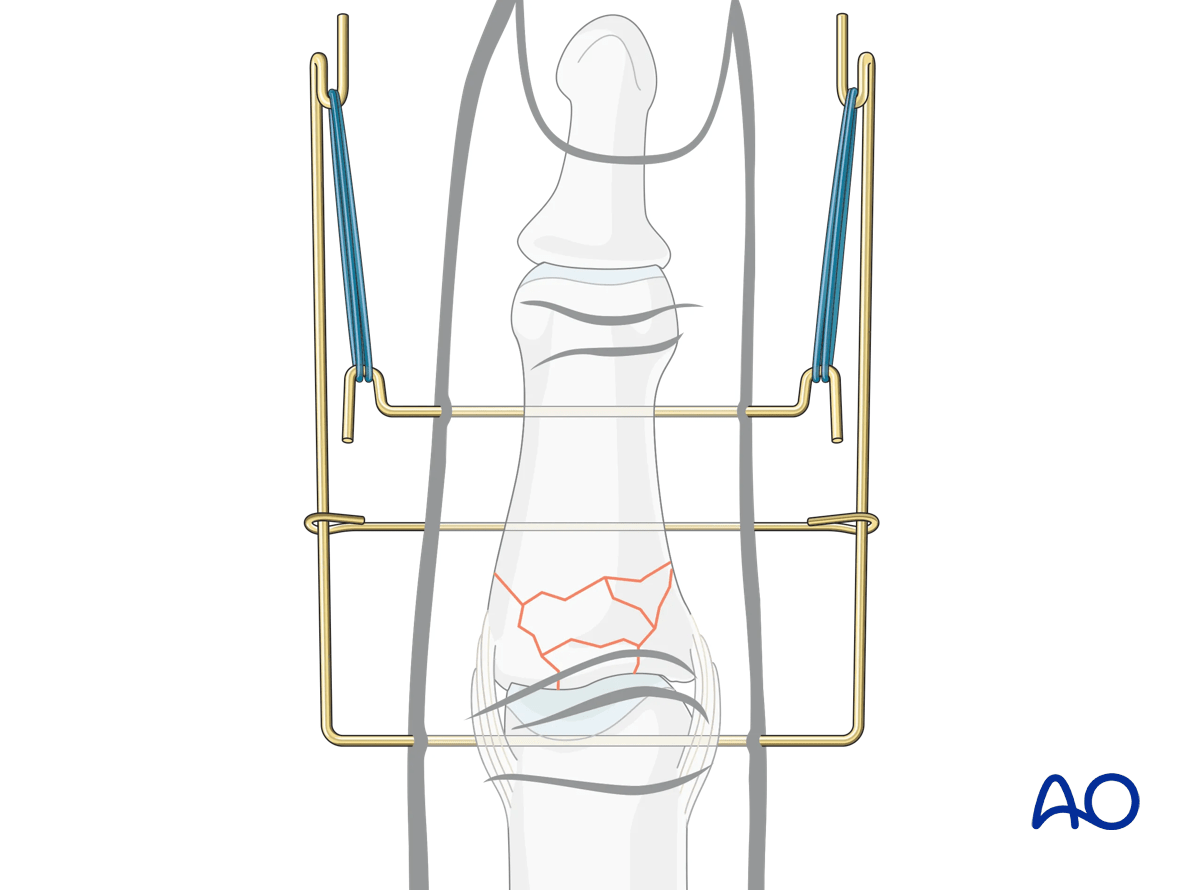
K-wire insertion
Insert the first K-wire (1.2 mm) in the center of rotation of the proximal phalangeal condylar block under image intensification.
Insert the second K-wire distal to the fracture up to the condyles of the middle phalanx parallel to the first K-wire.
Bending hooks
Bend both K-wires in a U-shape.
Leave at least 0.5 cm between the first bend and the skin.
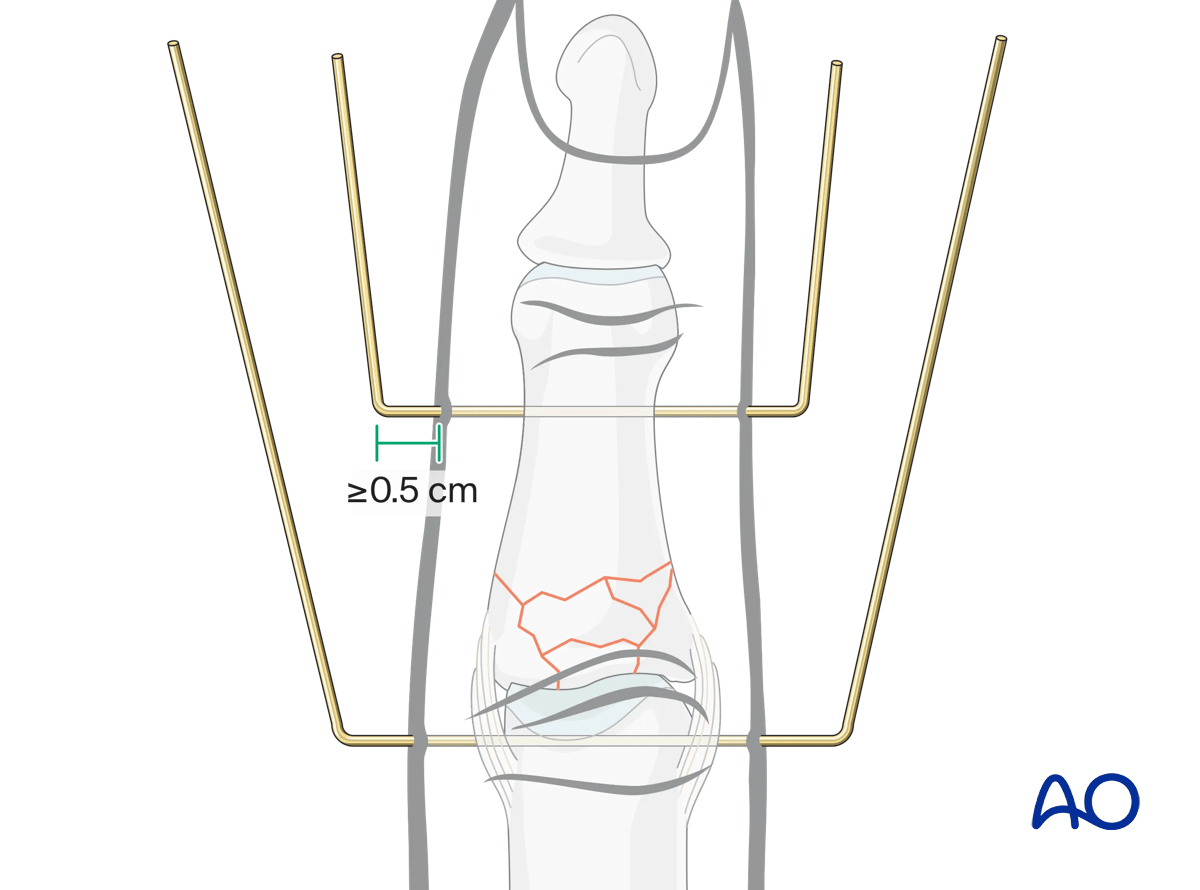
Create hooks, open proximally, on each end of the second K-wire close to the skin insertion.
Create hooks, open distally, on each end of the first K-wire so that they will be at least 2.5 cm distal to the second K-wire hooks.
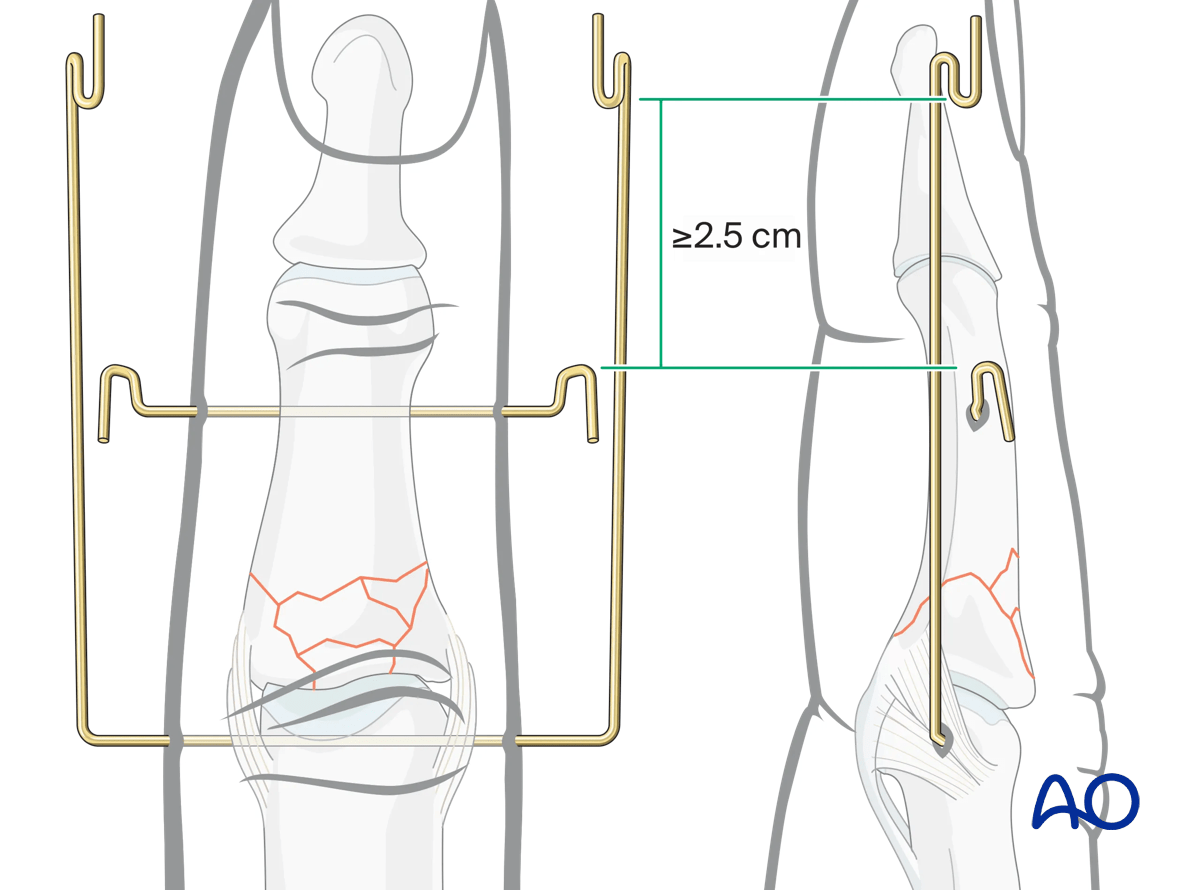
This will then allow for distraction with dental rubber bands.
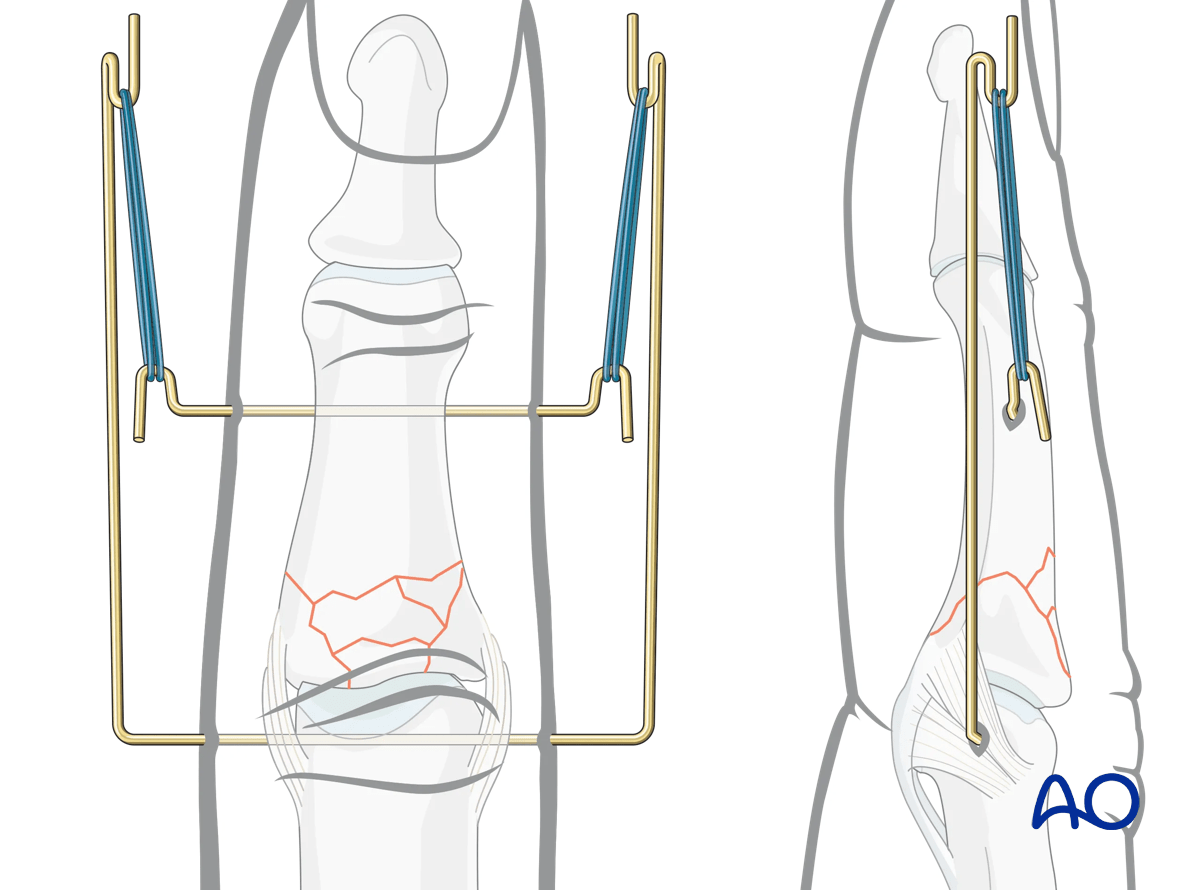
Option: third K-wire to prevent dorsal dislocation
Optionally, to control dorsal dislocation forces on the PIP joint, a third K-wire (1.0 mm) may be inserted in the middle phalanx to act as a fulcrum.
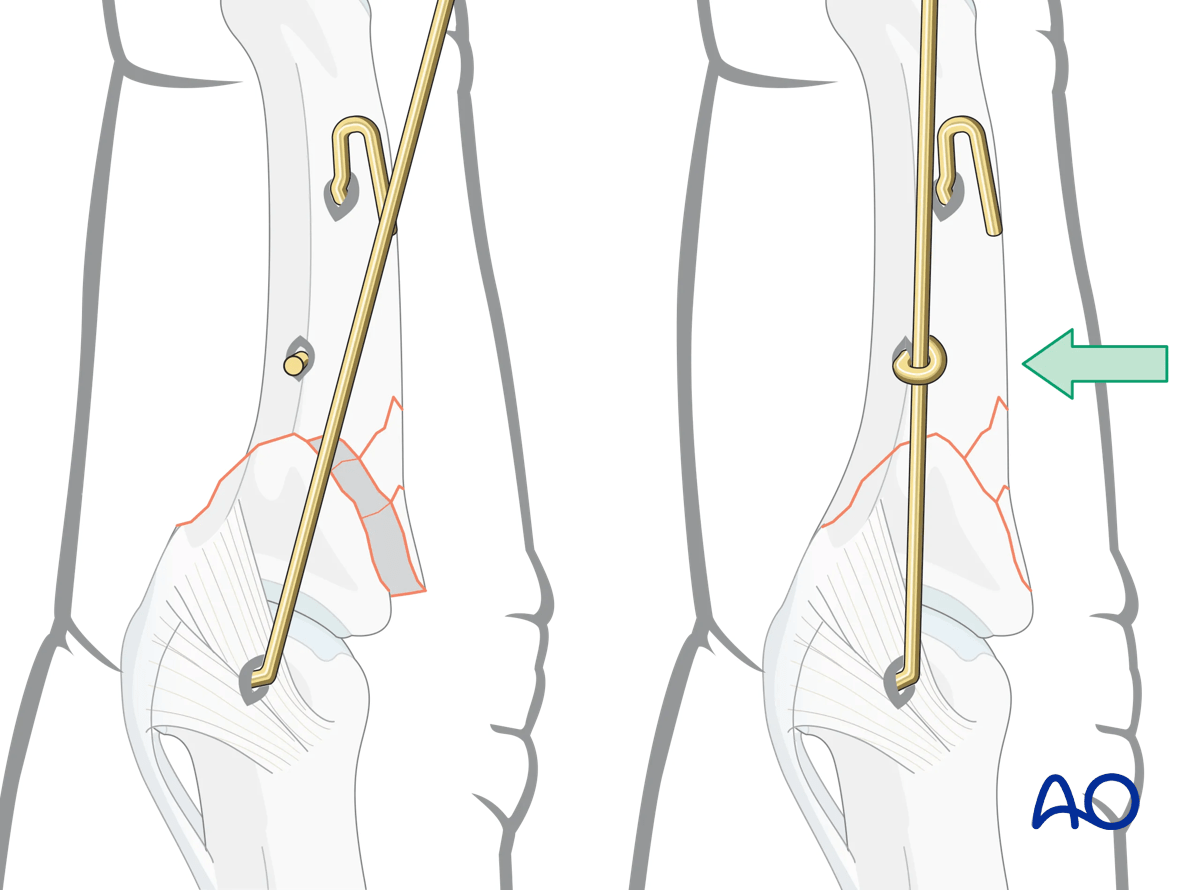
Insert it just distal to the fracture zone parallel to the other K-wires and palmar to the legs of the first K-wire.
Bend the ends around the legs of the first K-wire.
5. Final assessment
Check the construct and joint movement with an image intensifier.
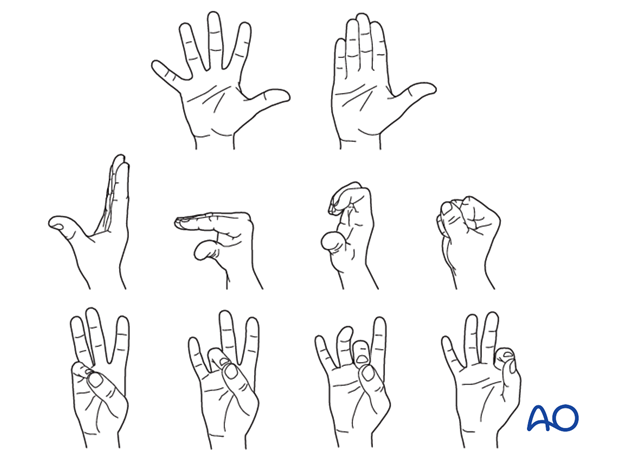
The awake patient should move the PIP joint through a range of motion.
6. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Mobilization
The patient should be instructed to begin active motion (flexion and extension) immediately after surgery to prevent joint stiffness.
Functional exercises of the unaffected joints should be started immediately to keep them mobile.
Pin-site care
Proper pin insertionTo prevent postoperative complications, pin-insertion technique is more important than any pin-care protocol:
- Correct placement of pins (see safe zones) avoiding ligaments and tendon
- Correct insertion of pins (eg, trajectory, depth) avoiding heat necrosis
- Extending skin incisions to release soft-tissue tension around the pin insertion (see inspection and treatment of skin incisions)
Various aftercare protocols to prevent pin-track infection have been established by experts worldwide. Therefore, no standard protocol for pin-site care can be stated here. Nevertheless, the following points are recommended:
- The aftercare should follow the same protocol until removal of the external fixator.
- The pin-insertion sites should be kept clean. Any crusts or exudates should be removed. The pins may be cleaned with saline and/or disinfectant solution/alcohol. The frequency of cleaning depends on the circumstances and varies from daily to weekly but should be done in moderation.
- No ointments or antibiotic solutions are recommended for routine pin-site care.
- Dressings are not usually necessary once wound drainage has ceased.
- Pin-insertion sites need not be protected for showering or bathing with clean water.
The patient or the carer should learn and apply the cleaning routine.
In case of pin loosening or pin-track infection, the following steps need to be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for a microbiological study to guide appropriate antibiotic treatment if necessary.
Before changing to a definitive internal fixation an infected pin track needs to heal. Otherwise, infection will result.
Follow-up
The external fixator may be removed with local anesthesia after 6 weeks. Check with x-rays for fracture consolidation and congruency.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
7. Case
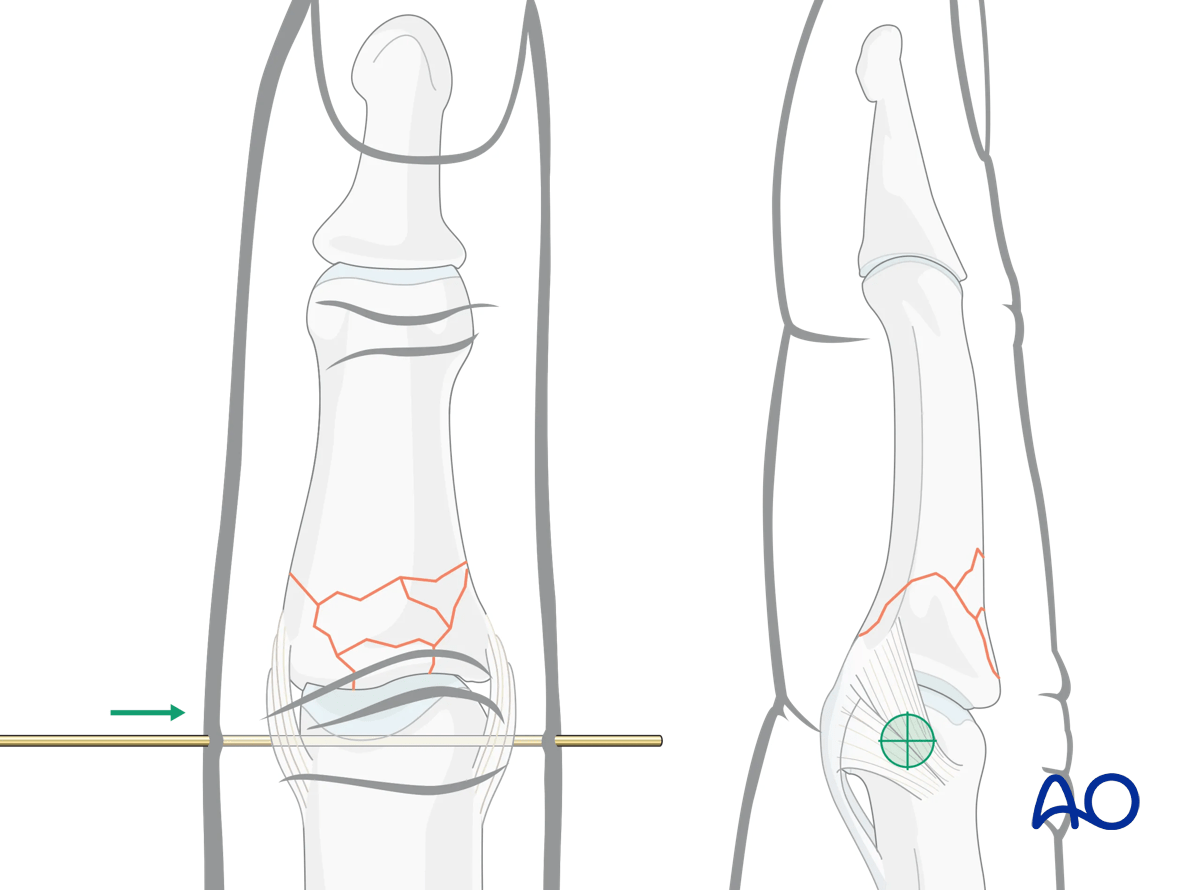
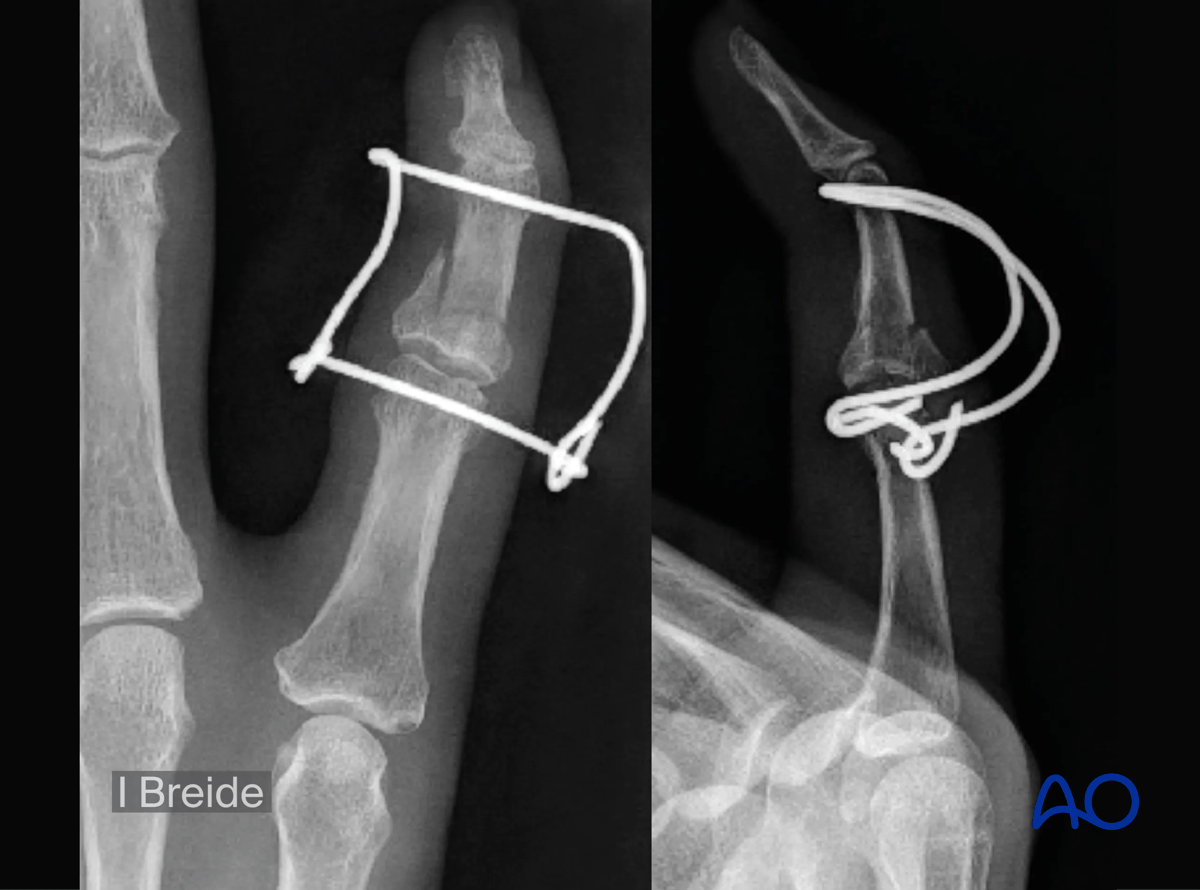
AP and lateral x-ray of a pilon fracture of the 5th middle phalangeal base.

Stabilization with a parabolic (Fibonacci type) dynamic external fixator
Clinical assessment with active motion of the PIP joint by the awake patient