Nonoperative treatment
1. General considerations
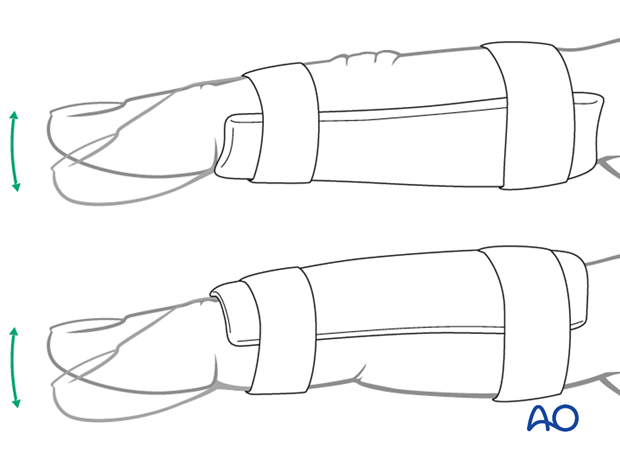
Dorsal avulsion fractures may be treated nonoperatively with a finger splint leaving the DIP and MCP joints free for active mobilization.
Either a dorsal or palmar application can be performed. The palmar splint provides more stability to the PIP joint.
2. Reduction of dislocation
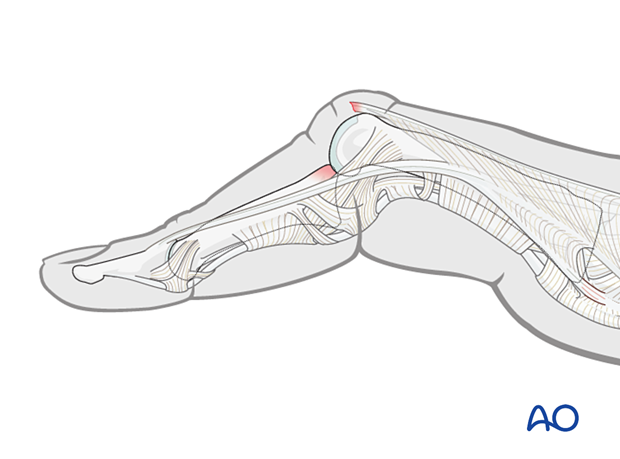
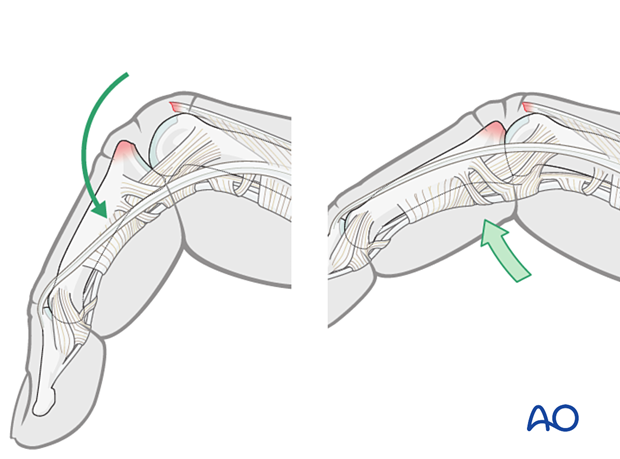
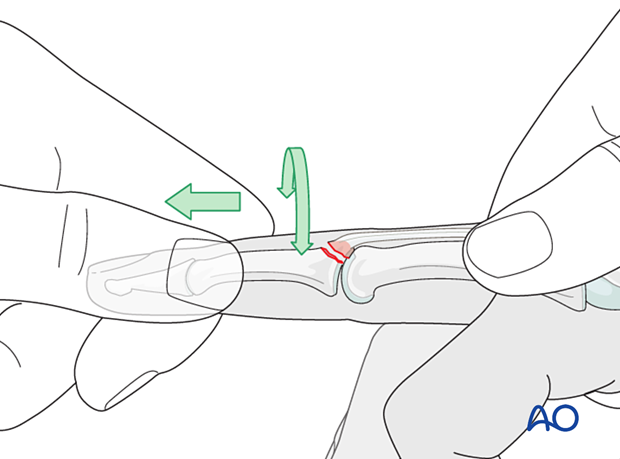
Dislocation usually occurs as a hyperflexion deformity.
This can be reduced by increasing the deformity with some volarly applied pressure on the middle phalanx to reduce the joint. This keeps the collateral structures in tension and reduced the risk of soft-tissue interposition.
3. Fracture reduction
Reduction is achieved by applying longitudinal traction and extension to the finger.
Rotational malalignment should be corrected.
Any angular deviation can be checked by comparison with the adjacent fingers and must be reduced.
Check the reduction using image intensification.
If the fracture does not reduce, usually this is an indication of soft-tissue interposition and surgical treatment should be considered.
Stability evaluation
Confirm reduction with an image intensifier and check the joint stability by passive flexion and extension. This should show congruent movement compared with the adjacent joints.
If the central slip avulsion fragment can not be perfectly reduced and maintained throughout full range of motion, surgical treatment is necessary.
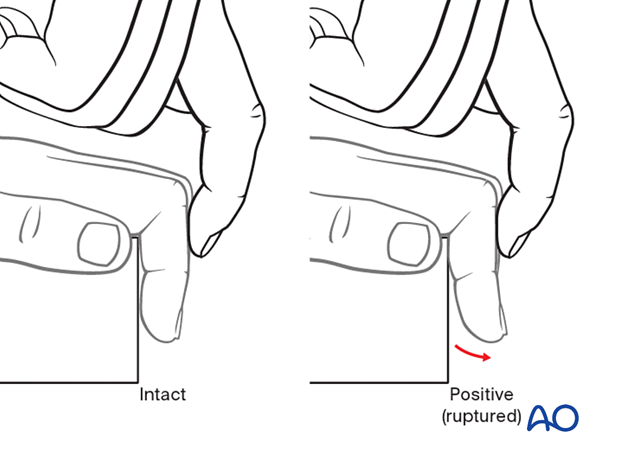
If there is no avulsion fragment visible in the x-ray, the central slip lesion should be assessed with the Elson test.
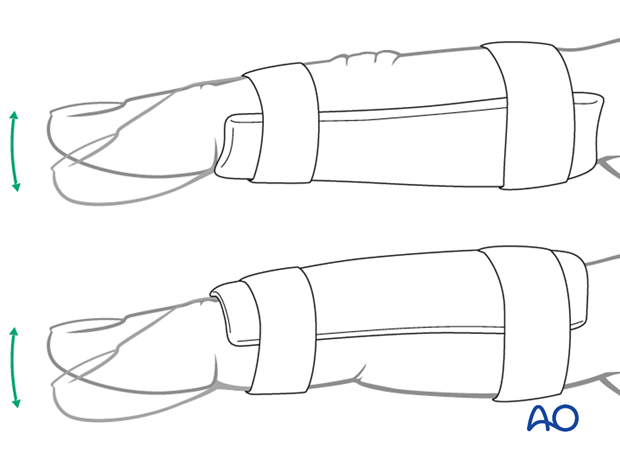
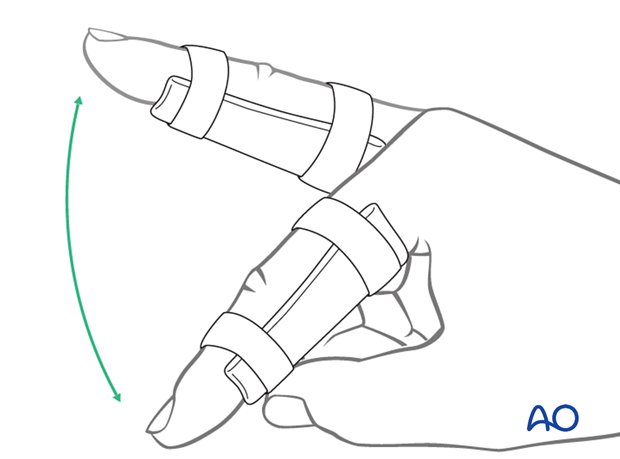
4. Application of finger splint
Finger splints can be created or purchased preshaped.
Apply the splint with the finger in extension.
Check with image intensification if there is remaining displacement.
5. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
The arm should be actively elevated to help reduce any swelling.
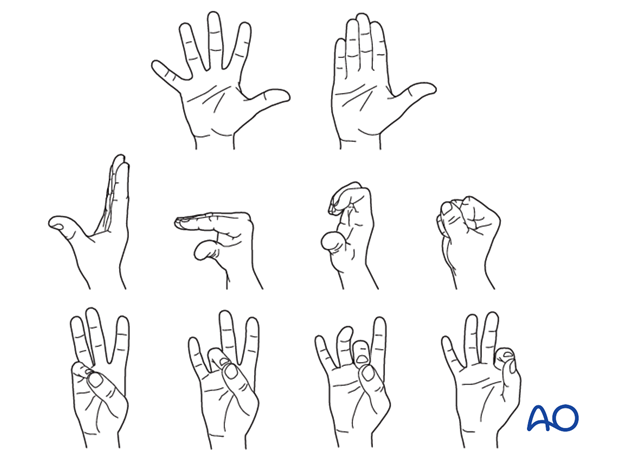
The patient should be instructed to immediately start mobilizing the DIP …
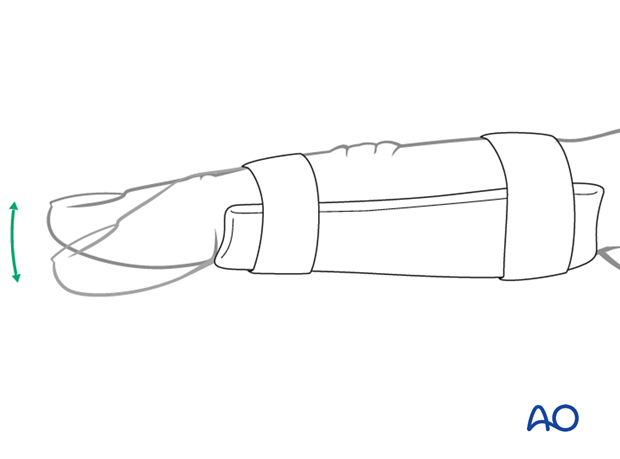
... and MCP joints to avoid extensor tendon adhesion and joint stiffness.
Cleaning
Removal of the splint and skincare must be performed by the patient at weekly intervals.
Instruct the patient to keep the finger in extension by pinching it with the thumb when the splint is taken off for cleaning or by pressing the tip of the finger onto a tabletop.
Any flexing of the finger may disrupt the healing process.

Follow-up
X-ray checks of joint position must be performed immediately after the splint has been applied.
Follow-up x-rays in the splint should be taken after 1 week and, if necessary, after 2 weeks. A final x-ray can be taken at the expected fracture consolidation.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
Immobilization in a splint is continued until about 4–6 weeks after the injury. At that time, an x-ray may be taken to confirm healing, and range of motion should be pain-free.
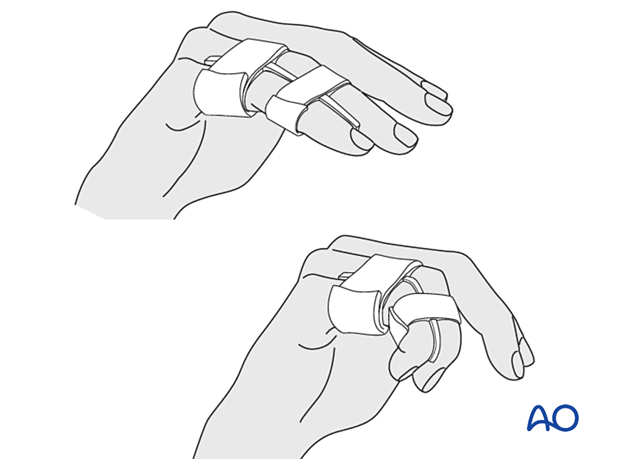
Buddy strapping
Buddy strapping to the adjacent finger, to neutralize lateral and rotational forces on the finger may be applied after splint removal during rehabilitation to start with full mobilization.
Mobilization
Functional exercises are recommended.
In the absence of pain during functional activities, full manual loading can be permitted. In case of doubt, an x-ray to confirm healing and consolidation, which would be expected by 8 weeks, should be taken.