Patient assessment
1. Introduction
Hand surgery involves a multi-specialty approach to the assessment, treatment, and aftercare of hand trauma. Therefore, the specialized teams should be involved early on according to the specific injury requirements.
A diagnosis is made based on the history, the mechanism of the trauma, clinical examination, and by x-rays in 2 planes.
The outcome of injuries of the fingers may be assessed by three criteria:
- Functional return
- Clinical assessment
- Radiological healing
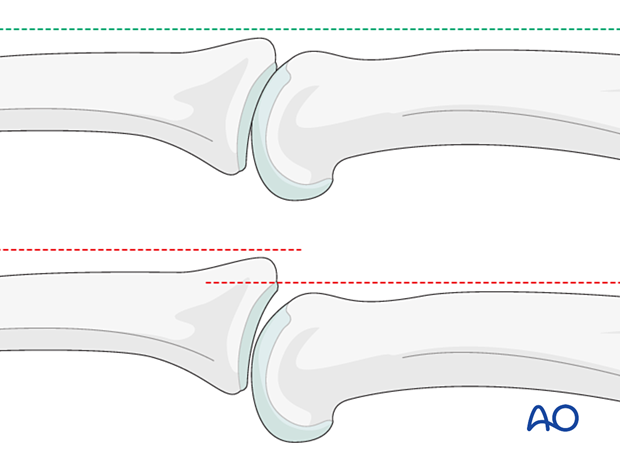
Recommendations for the definition of extraarticular phalangeal fracture displacement vary. In the following, the definitions of the important relevant displacement are:
- No malrotation is accepted
- >2 mm of translation or axial displacement
- >10° of angular displacement
- Freeland AE, Geissler WB, Weiss APC. Surgical treatment of common displaced and unstable fractures of the hand. Instr Course Lect. 2002:51:185–201.
2. Clinical assessment
Check for:
- Swelling
- Open wound
- Loss of sensation in the fingers (indicating nerve injuries)
- Perfusion (reperfusion of more than 2 seconds may indicate vascular injuries)

General assessment of hand and wrist
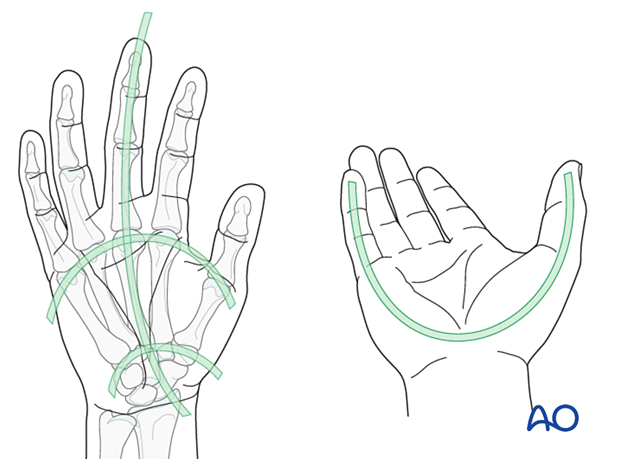
Check for anatomical architecture (position and relation) of the whole hand:
- Longitudinal arc
- Metacarpal arc
- Oblique arcs (with thumb in opposition)
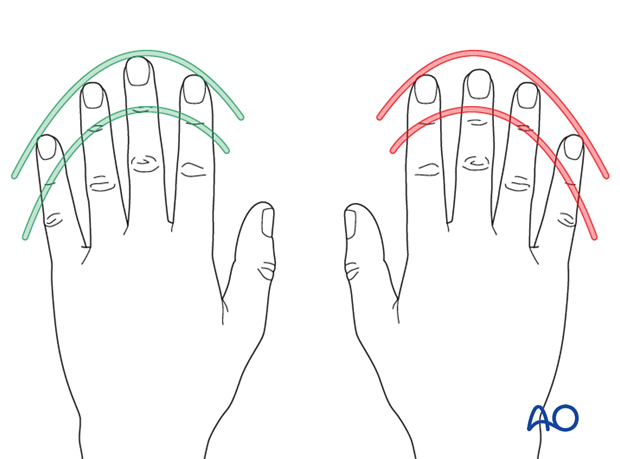
The tips of the flexed fingers should point to the scaphoid. Check for deviating or overlapping fingers. This will indicate malrotation.
The nails should be aligned.
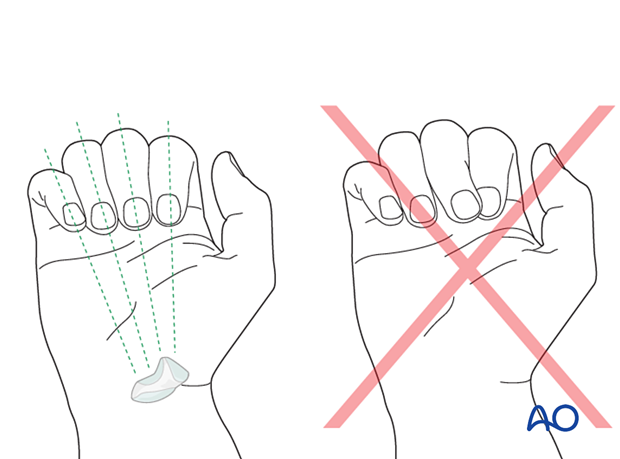
Flexing the fingers shows some overlap of the tip of the ring finger with the little finger which indicates rotational malalignment.

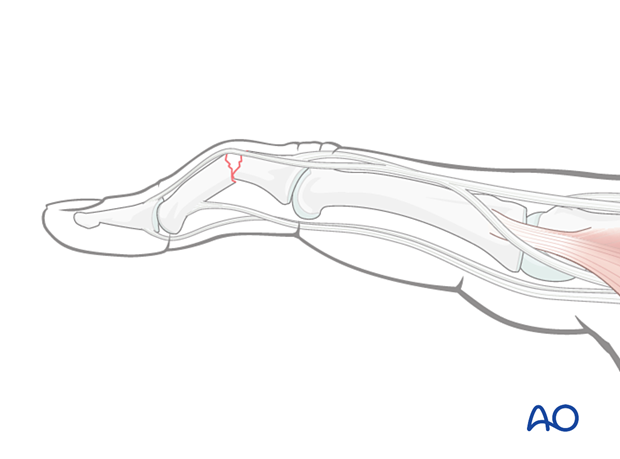
Assessment of the middle phalanx
Check for shortening of a finger. An interrupted arch of the DIP joints indicates shortening.
Check for deformity of a phalanx. In a fracture situation, the distal fragment may be pulled into flexion.
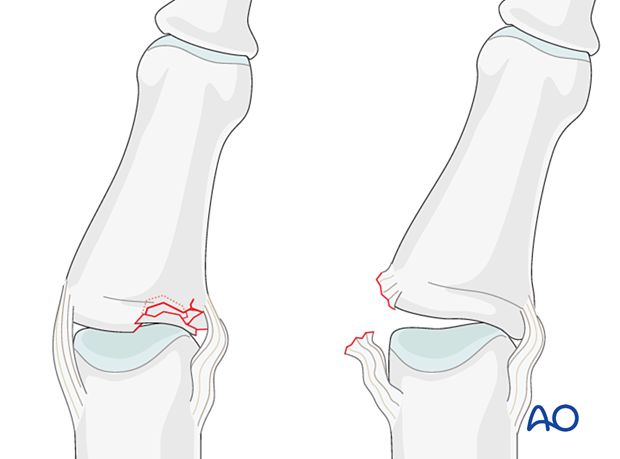
Lateral stress test
Check the MCP, PIP, and DIP joint stability (varus/valgus stress test). Compare this with the contralateral finger.
Lack of lateral stability indicates injury of the collateral ligaments or their bony attachments.
A typical sign of collateral ligament injuries is abnormal lateral mobility of the PIP joint, persisting after reduction of the dislocation, when the patient can flex and extend the finger.

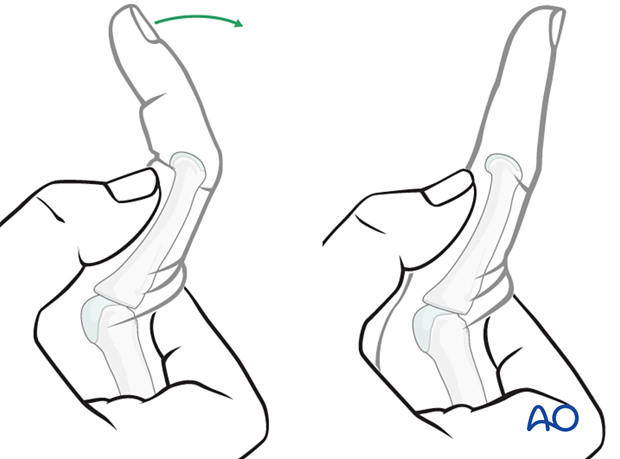
Lateral (varus/valgus) stress test showing lateral joint instability. This should be performed with slight joint flexion (ca 20°).

Use gentle passive lateral stress to detect instability. If instability is present, this may indicate an impaction fracture or, rarely, avulsion of a collateral ligament.
Recognizing detachment of the central slip
Early diagnosis of injuries is important. This is not always easy due to the swelling and often inconclusive x-rays.
Boutonnière deformity is an indication for central band avulsion.
Keep the PIP joint hyperextended. Passively flex the DIP joint.
If passive movement of the DIP joint is limited, this strongly indicates a central slip detachment.
Compare this with the uninjured hand.
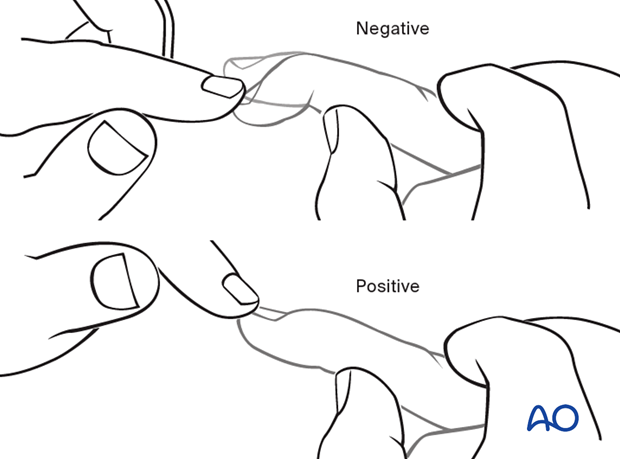
The PIP joint of the injured finger is flexed to 90° and, with the hand resting on a table, the finger is positioned over the edge of a table.
Hold the middle phalanx in position and ask the patient to extend the distal phalanx. The test is positive, if there is weak extension at the PIP joint with hyperextension at the DIP joint.
To recognize detachment of the central slip, ask the patient to extend the PIP joint with the MCP joint in hyperextension.
If the PIP joint can be fully extended in this position, the central slip is still attached, and nonoperative treatment may be indicated.
PIP stability check
Ask the patient to flex the finger under image intensification. Ultrasound may be helpful to evaluate the instability of the injury in a dynamic way. Passive lateral movement of the finger under image intensification will help to assess lateral stability.
3. Radiologic evaluation
X-rays
AP view of the whole hand and true lateral view of the finger are needed for diagnosis.
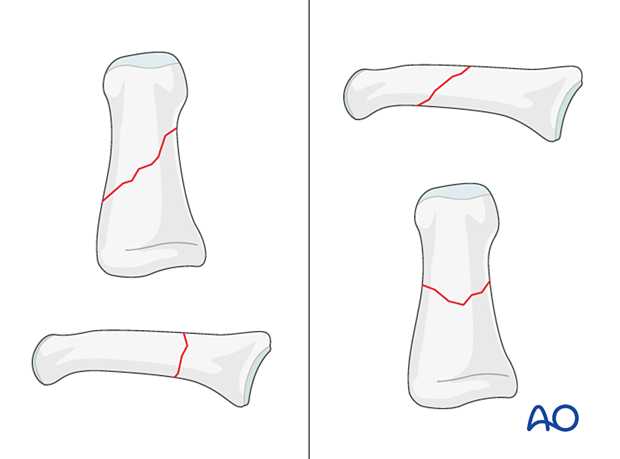
All views need to be inspected to get information about the fracture pattern, eg, the orientation of an oblique fracture plane.
These x-rays show an articular fracture of the 4th middle phalangeal head with extension in the shaft.

Obliquity of the fracture is possible either in the plane visible in the AP view or the plane visible in the lateral view. Always confirm the fracture configuration with views in both planes.
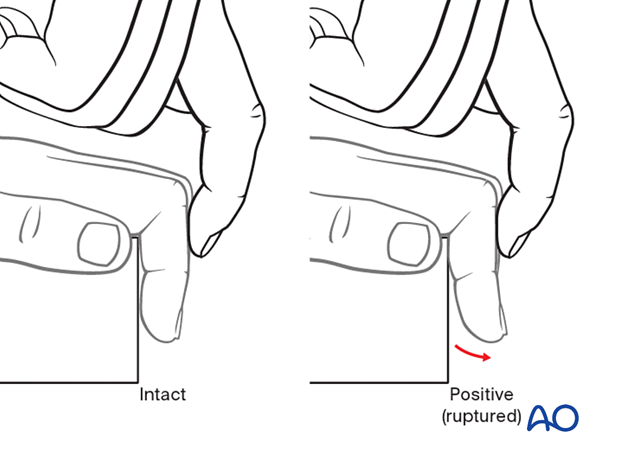
Ultrasound
Ultrasound evaluation may help define suspected ligament and tendon injuries.
This image shows an avulsion of the volar plate from the proximal phalanx.
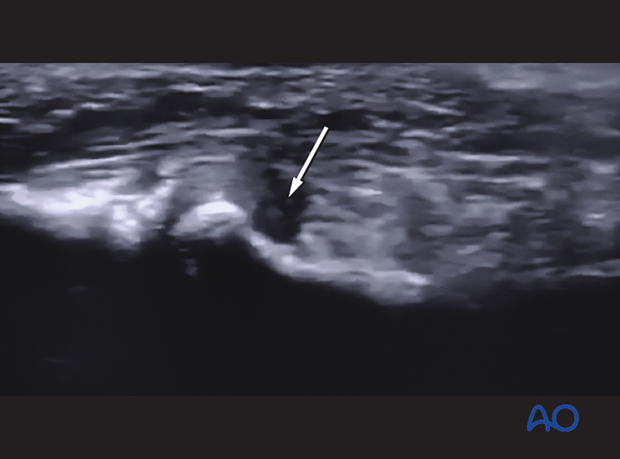
This video shows the same soft-tissue lesion under active motion of the PIP joint.

CT imaging
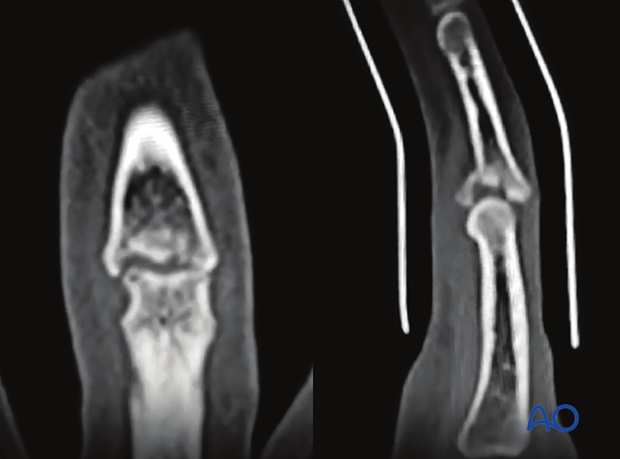
CT imaging is helpful to assess impacted intraarticular fractures, to evaluate the fragmentation and plan for reconstruction.
Coronal and sagittal CT views of the middle phalangeal base showing an articular fracture with central impaction.
MRI
Isolated ligamentous injuries may be seen in an MRI.
4. Recognizing subluxation
Often, a subluxation is not immediately apparent on the lateral view. In the lateral x-ray, look for the characteristic “V” sign of diverging joint surfaces, which indicates this injury.
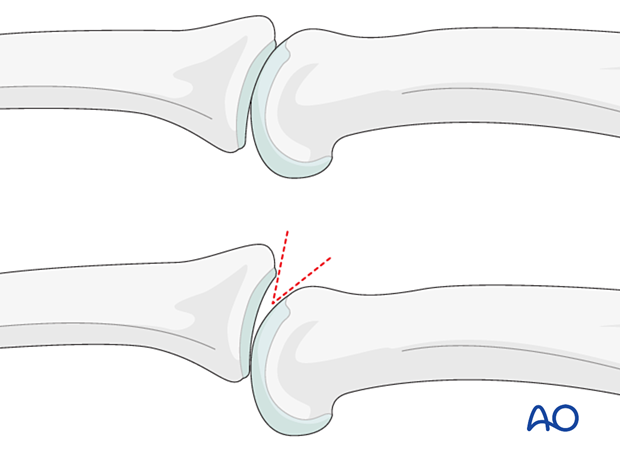
In the lateral view, the dorsal cortical profiles of the proximal and middle phalanges should be collinear. Any axial malalignment is a clear indication of subluxation.