Complications and technical failures
1. General considerations
The most frequent complications are related to soft-tissue problems including tendon adhesions, intraarticular fibrosis, and scarring around implants and the surgical site. Attention to careful soft-tissue management and early rehabilitation including mobilization and appropriate splintage are all relevant to prevention of these problems.
Common complications of these injuries are:
- Malunion
- Nonunion
- Infection (general complication)
- Tendon adhesion
- Soft-tissue contractures
Malunion and nonunion may cause subsequent degenerative changes in the associated joints.
Soft-tissue adhesions and contractures will cause restriction of movement and may promote instability at the affected joints.
If symptoms become functionally intrusive, revision surgery may be indicated.
2. Malunion
Consequences of malunion
Malunion is usually a consequence of inaccurate reduction and ineffective fixation.
It strongly affects the balance of flexor and extensor mechanisms and biomechanical relations of the hand. For example:
- Angulation may result in loss of grip strength.
- Rotation is usually associated with an oblique or spiral fracture and may result in loss of length leading to reduction of dexterity.
- Rotational malalignment will also compromise palmar grip, resulting in weakness due to conflict with neighboring fingers.
It is crucial to confirm any alteration of alignment, especially angulation, rotation, and length.
Prevention
- Anatomical reduction
- Stable fixation
- Intraoperative assessment of construct stability
- Postoperative radiological assessment of reduction and fixation
Management of malunion
- Corrective osteotomy
- Bone graft application, if necessary
- Stable internal fixation
If an osteotomy is indicated, consider correction of rotational malalignment at a different site to avoid further soft-tissue damage.
3. Nonunion
Signs for nonunion are pain and nonbridging healing on x-ray or CT in a period of 6–9 months after treatment.

Prevention
- Gentle operation technique to avoid damage to bone, soft tissue, and vascular supply
- Intraoperative assessment of construct stability
- Postoperative radiological assessment of reduction and fixation
- WALANT (wide awake local anesthetic no tourniquet) techniques permit intraoperative assessment of stability and range of motion so that early rehabilitation can be started.
Concomitant injuries should be addressed at the same time as the fracture to improve stability.
Appropriate postoperative management will help to protect the fracture.
Management of nonunion
Treatment of nonunion includes:
- Nonunion resection
- Bone graft application
- Stable internal fixation
4. Volar rim and volar plate injuries in the proximal interphalangeal joint
Complications
In dislocation of the proximal interphalangeal (PIP) joint, ligaments are often ruptured. These soft-tissue injuries usually heal without reconstruction. However, collateral ligament and volar plate ruptures may need repair (anchor sutures or bone tunnels) if the joint remains unstable after reduction and fixation.
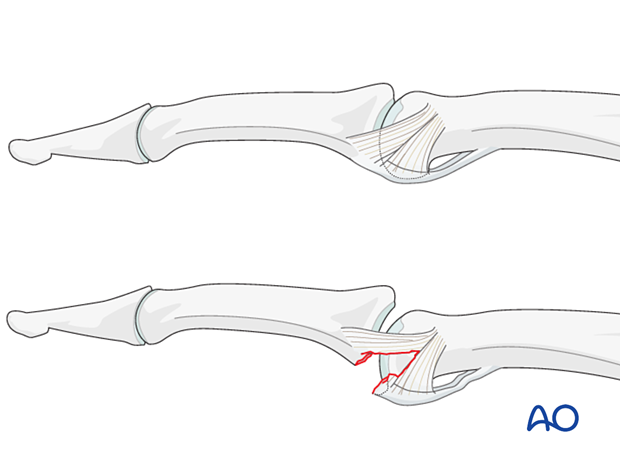
Management
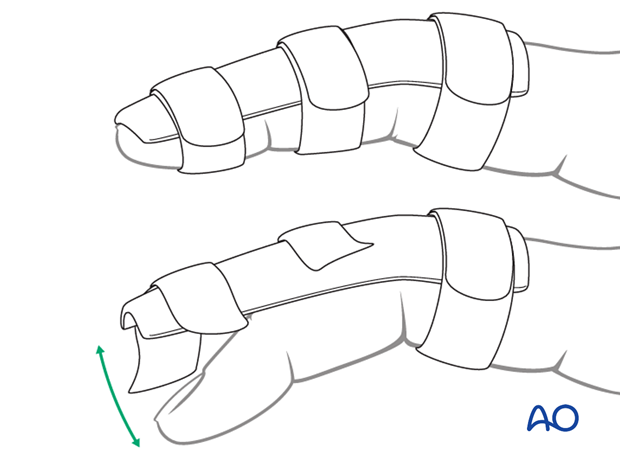
Volar plate avulsion fractures without radiological subluxation and small fragments <2 mm are treated preferably nonoperatively with an extension block splint. This would allow for some flexion of the joint to prevent stiffness.
Displaced large fragments (>30% of the articular surface) or fragments rotated more than 90º are an indication for reduction and fixation.
CT imaging is recommended to assess the true size of fracture fragments as they may be bigger than observed on an x-ray due to cartilaginous components.
Depending on the size of the fragment, the fracture is stabilized with lag-screw or K-wire fixation, suture anchor or bone tunneling, or cerclage wiring.
An extension block splint should be applied for 4 weeks to support the internal fixation.
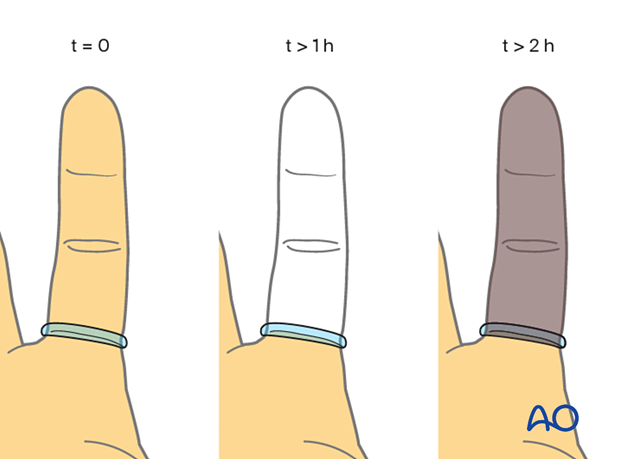
5. Small tourniquet removal
If a small tourniquet has been created with the finger of a glove, make sure to remove it at the end of the surgery.
Failure to do so may result in ischemia and subsequent loss of the finger!
6. Case of nonunion after K-wire fixation
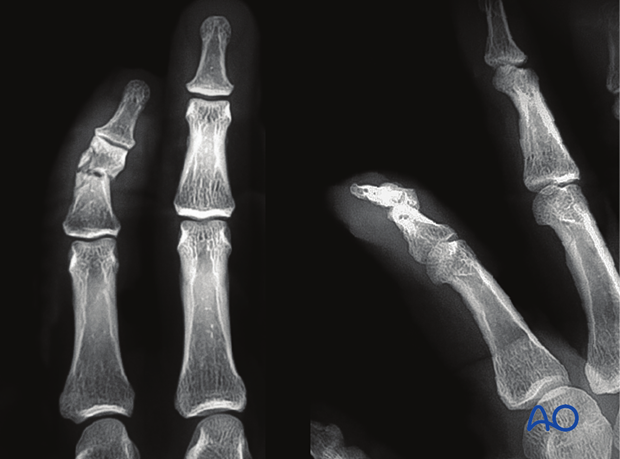
Postoperative AP x-ray of a middle phalangeal shaft fracture of the index finger incompletely stabilized with two K-wires.
This fixation has not provided resistance to rotational displacement.

Lateral x-ray

AP x-ray at 5 weeks postoperative.
Oligotrophic nonunion is likely because there is rotational instability at the fracture site.

AP and lateral x-rays at 16 weeks.
Nonunion with displacement and shortening of the middle phalanx is evident. Rotational deformity of the finger will be expected due to the obliquity of the fracture.

AP x-ray after revision surgery with strut plate fixation.
Axial alignment and rotational correction have been achieved.

AP and lateral x-rays of the healed fracture














