Lag screw fixation
1. Principles
Fracture type
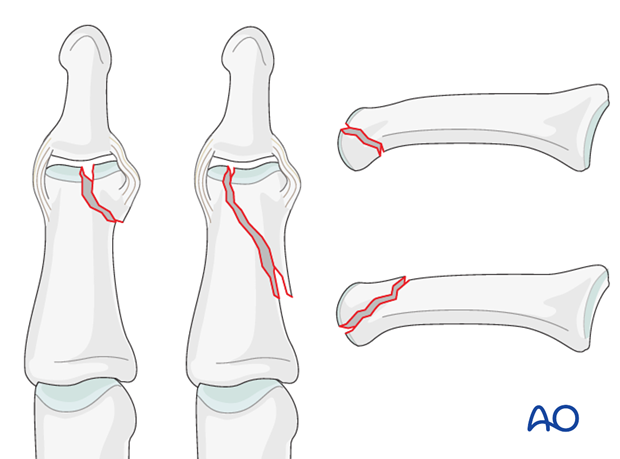
Unicondylar fractures of the middle phalanx can be transverse, short or long oblique, or comminuted. Typically they are the results of a sports injuries, caused by axial load combined with lateral angulation of the finger.
Condylar fractures tend to be very unstable and should usually be treated operatively. If conservative treatment is attempted, secondary displacement, leading to angulation of the finger, often ocurrs.
Short and long oblique fractures
Short oblique fractures typically originate in the intercondylar notch.
Long oblique fractures more often originate through one of the condyles, splitting proximally towards the diaphyseal cortex on the side of the uninjured condyle.
Outcome of fractures of the middle phalanx is usually more favourable than in the proximal phalanx. This is largely due to the fact that limitation of DIP joint motion is not as great a problem as similar limitations in the PIP and MP joints.
However, since fragments in this segment are generally smaller than in the proximal phalanx, management and stabilization can be more of a challenge.
Consequences of malunion (pain or deformity), or of degenerative joint disease, at the DIP joint can well be dealt with by arthrodesis, which is a procedure with very predictable outcome.
Caveat
These fractures are rare, but difficult to treat. There is an increased risk of joint stiffness resulting from these fractures.
It is wise to use magnifying loupes in these procedures. Gentle and precise handling throughout the procedure is mandatory.
K-wire fixation
Percutaneous K-wire fixation is often used for fractures of the middle phalanx.
The advantages are
- technically easy
- minimal soft-tissue lesion
- affordable cost
- universal availability
However, there are some disadvantages which can sometimes be significant, such as
- less stable fixation
- no compression possible
- no early mobility
- may separate the fragments
- may irritate the skin
Anatomical reduction recommended
Although the DIP joint is very forgiving, articular fractures should be reduced anatomically, otherwise, the articular cartilage may be damaged, leading to painful degenerative joint disease and digital deformity. At the DIP joint, this can well be dealt with by arthrodesis, which is a procedure with very predictable outcome, without any major perturbances of the finger.
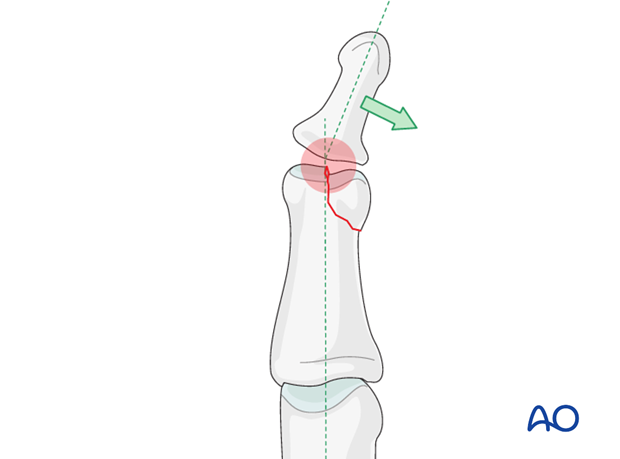
This illustration shows how even slight unicondylar depression may lead to angulation of the finger.
2. Approach
For this procedure a midaxial approach to the middle phalanx is normally used.

3. Reduction
Visualization of the fracture
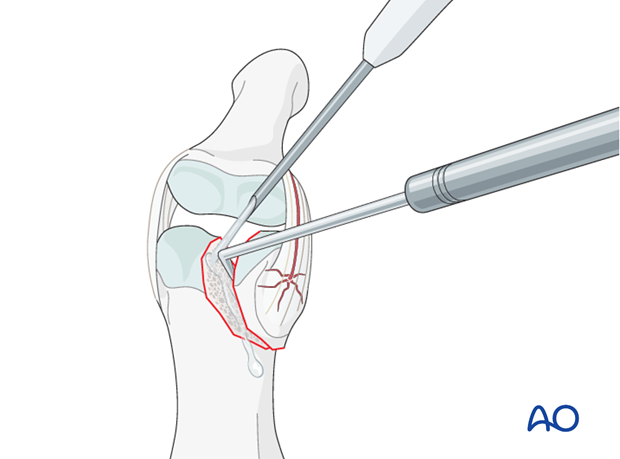
In order to gain a better view of the fracture, use a syringe to irrigate out blood clots with a jet of Ringer lactate.
Gently explore the fracture site to assess its geometry, using a dental pick. The pick can also be used carefully to reduce small fragments. Take great care to avoid comminution of any fragment.
It is important to maintain the vascularity of tiny fragments attached to the collateral ligament, in order to avoid osteonecrosis.
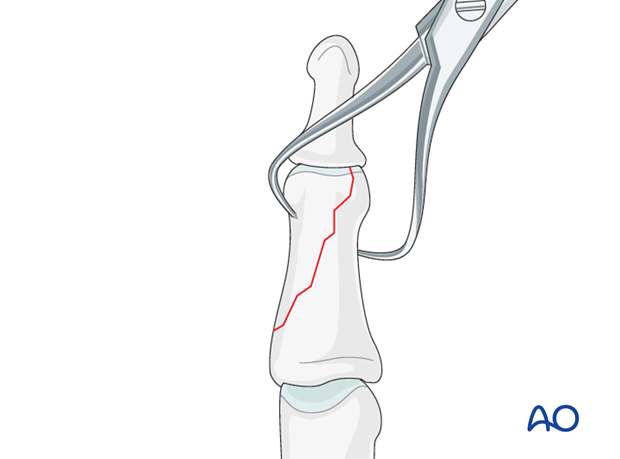
Indirect reduction
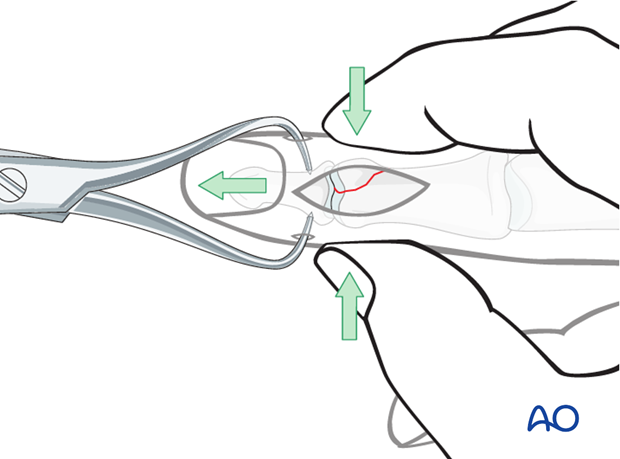
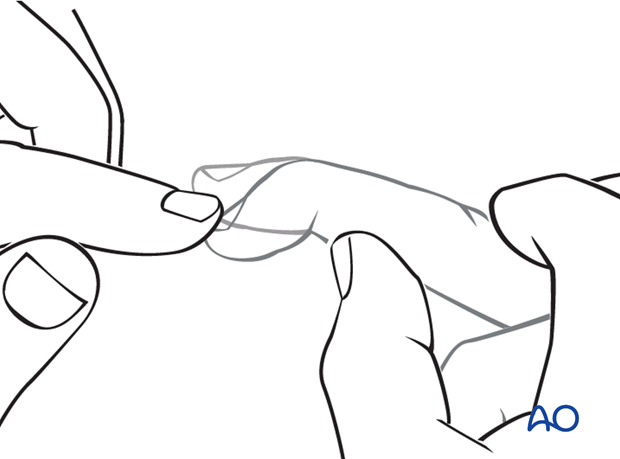
Reduction starts with traction in order to restore length.
Lateral pressure, exerted by the surgeon’s thumb and index finger, will then reduce the fracture.
Confirm reduction using image intensification.
Direct reduction of large fragments
A small pointed reduction forceps can be used for larger fragments gently to rock the fracture from side to side. Be careful not to apply excessive force as this can lead to fragmentation.
Confirm reduction using image intensification.
Note
Anatomical reduction is important to prevent chronic instability or posttraumatic degenerative joint disease.
4. Decision making
Different types of treatment are available for the various fracture types.
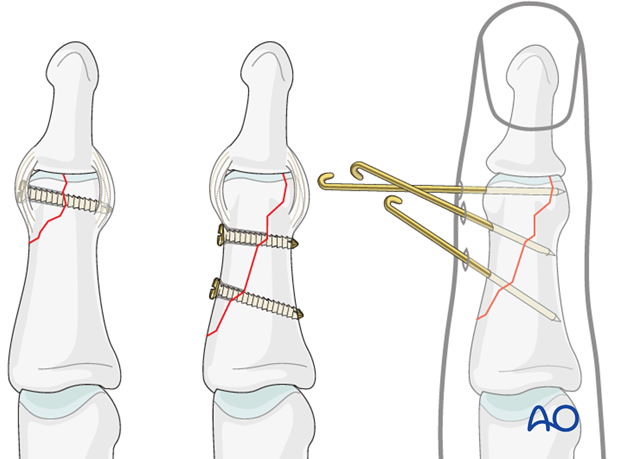
Short oblique fractures
Fixation with one lag screw, or a percutaneous K-wire, is recommended.
Long oblique fractures
Fixation with 2 lag screws is recommended. One or more K-wires is another option, although concerns about instability exist.
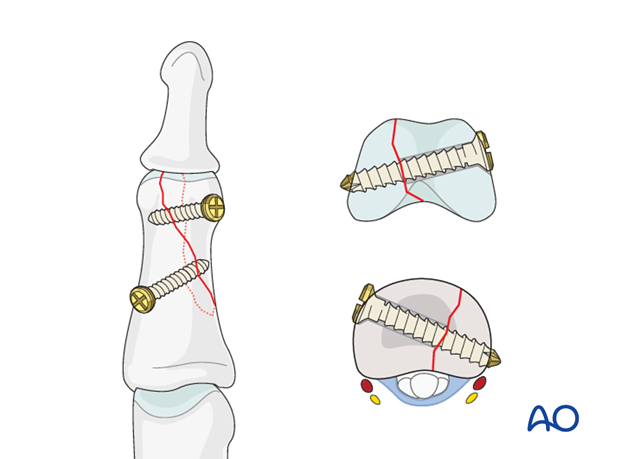
Planning screw placement
Large fragments
In large fragments, all screws can be placed safely proximal to the collateral ligament of the DIP joint.
Small fragments
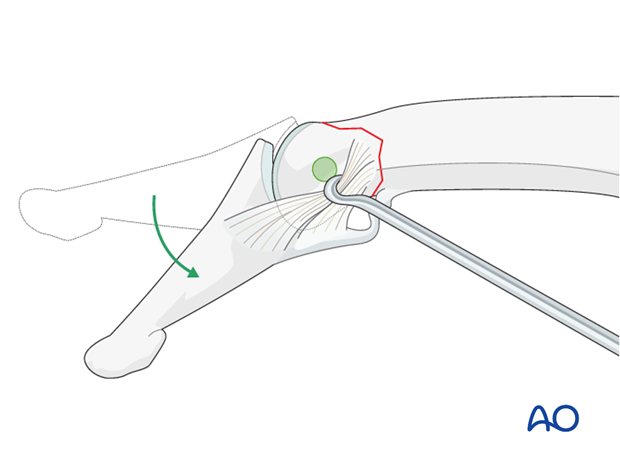
If only one screw can be inserted into a small fragment, it will have to be placed within the joint cavity, but through the nonarticular face of the condyle, distal to the collateral ligament.
The lateral aspect of the phalangeal head, which is safe for screw placement, can be approached by flexing the DIP joint.
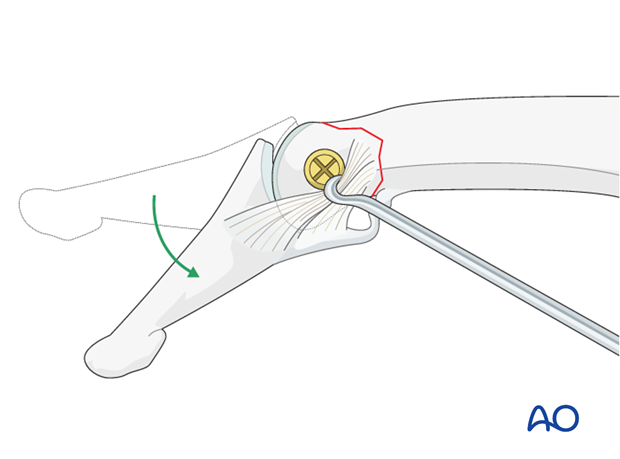
5. Small fragment fixation
Determining screw size
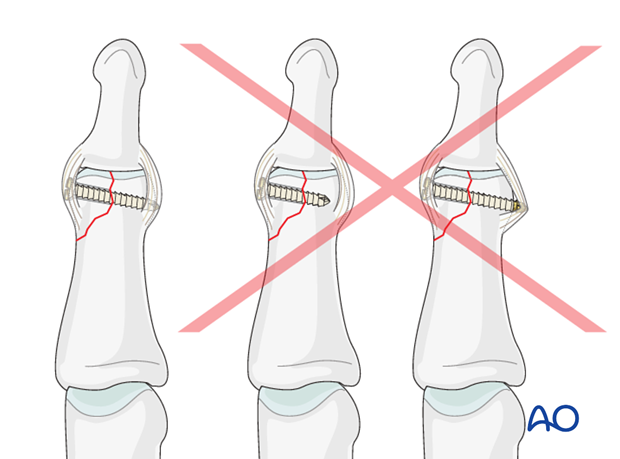
Screw length needs to be adequate for the screw just to penetrate the opposite cortex.
Keep in mind that at the apex of the fragment, the minimal distance between the screw head and the fracture line must be at least equal to the diameter of the screw head. If necessary, a screw of smaller diameter will have to be chosen.

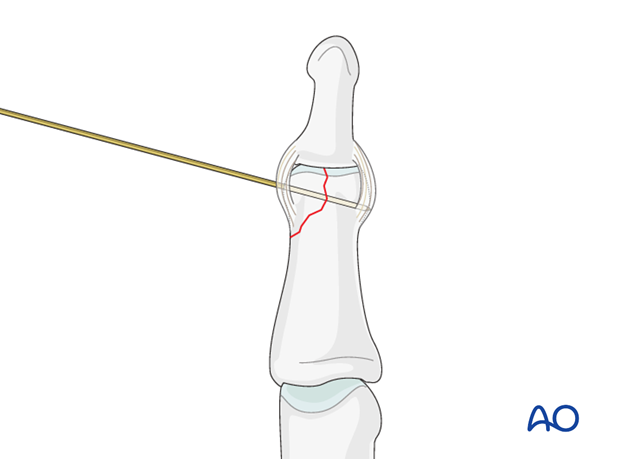
Prepare for drilling
Approach the outer surface of the phalangeal head by flexing the DIP joint.
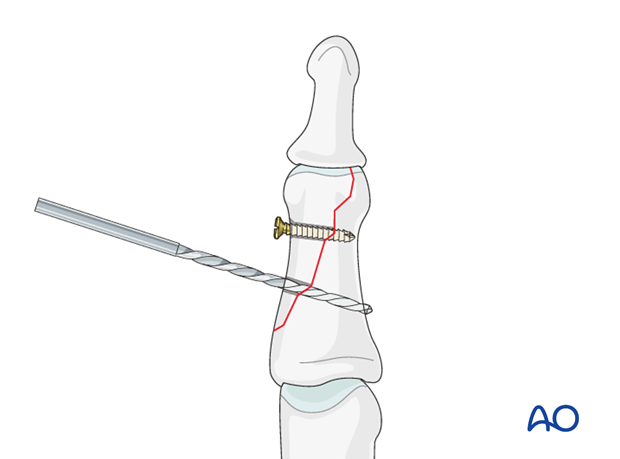
Drilling
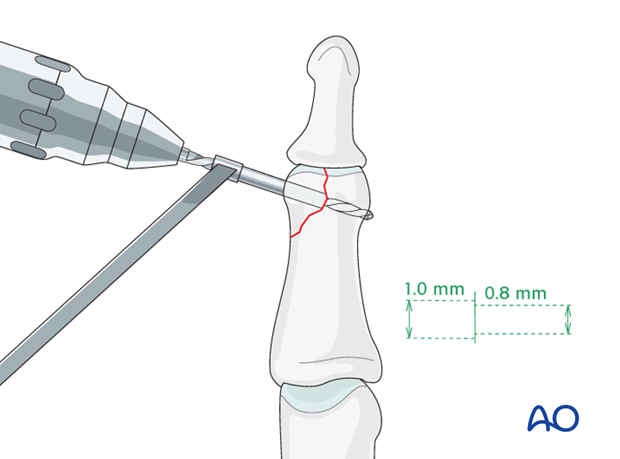
Drill a gliding hole for a 1.0 mm screw, as perpendicularly to the fracture plane as possible, using a 1.0 mm drill bit.
Use a 0.8 mm drill bit to drill a thread hole in the opposite fragment, just through the far (trans) cortex.
Note
Be careful to select appropriately-sized instruments. The use of too large drill bits or screws may result in fragmentation.
Screw length pitfalls
Ensure that a screw of the correct length is used.
- Too short screws do not have enough threads to engage the cortex properly. This problem increases when self-tapping screws are used due to the geometry of their tip.
- Too long screws endanger the soft tissues, especially tendons, ligaments and neurovascular structures. With self-tapping screws, the cutting flutes are especially dangerous, and great care has to be taken that the flutes do not protrude beyond the cortical surface.
Insert lag screw
Insert the lag screw and gently tighten it to compress the fracture.
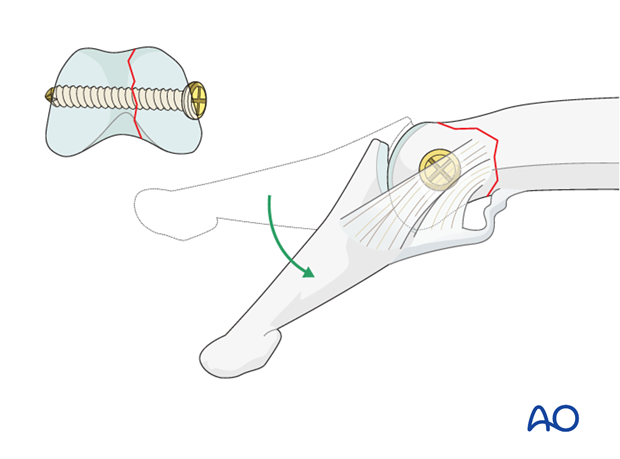
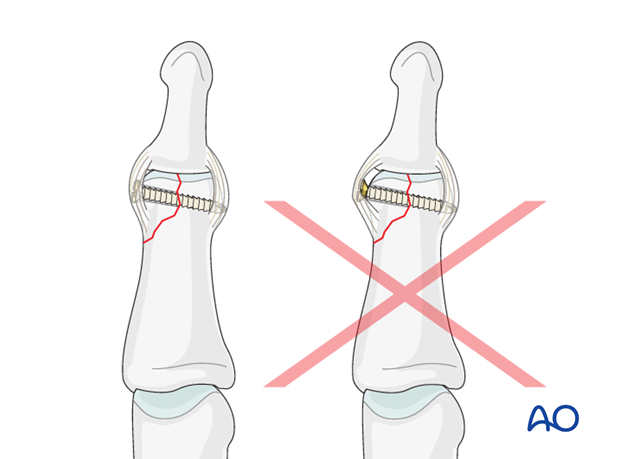
Pitfall: protruding screw head
A protruding screw head can cause ligament irritation and eventual joint stiffness.
In order to avoid such protrusion, slightly enlarge the entrance to the screw hole in order partially to sink the screw head. Do not attempt to countersink with too large a tool, and be careful not to overtighten the screw, to avoid fragmentation.
Alternative fixation: K-wire
As alternative fixation of a small-fragment fracture, a K-wire can be used.
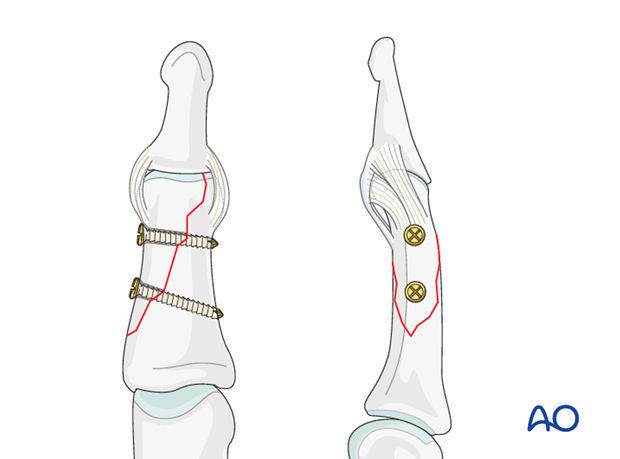
6. Large fragment fixation
Preliminary fixation (large fragments)
Long oblique fractures can be preliminarily fixed by inserting a K-wire. Be careful to place it in such a way that it will not conflict with later screw placement.
Avoid inserting a K-wire into small fragments, as they are in danger of fragmentation.
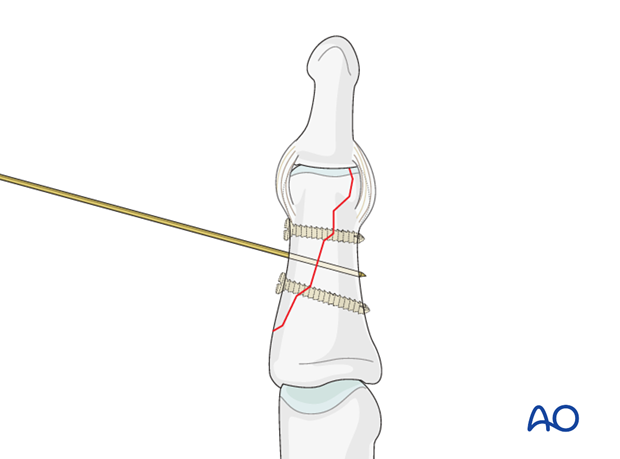
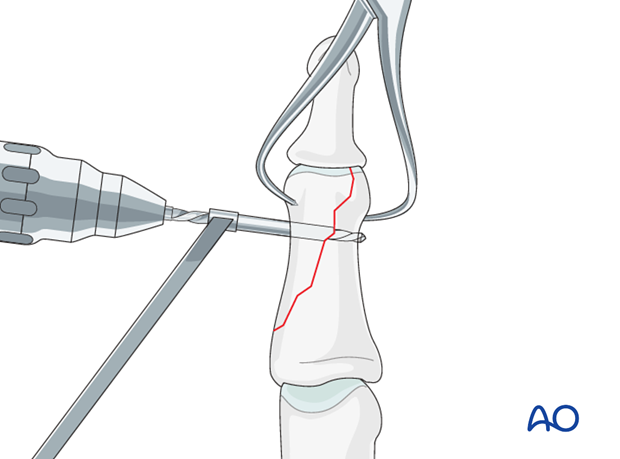
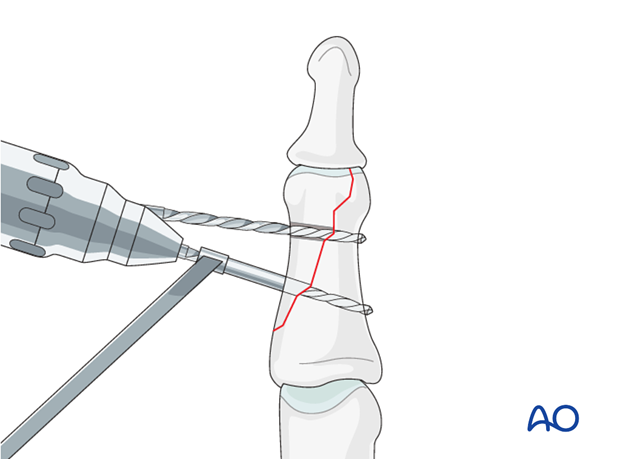
Drilling and alternative preliminary fixation
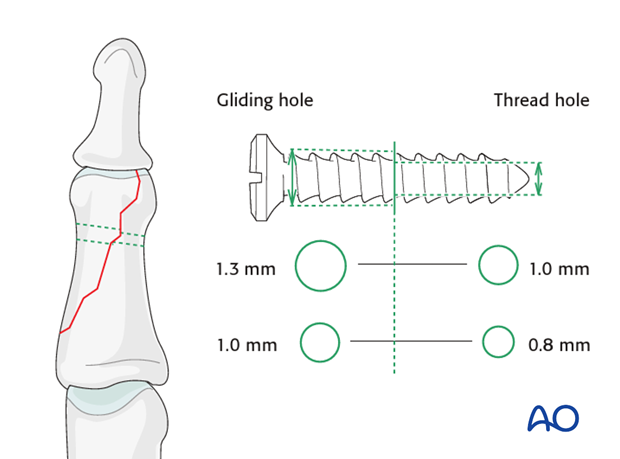
Leaving the reduction forceps in place, drill a gliding hole as perpendicularly to the fracture plane as possible, using a 1.3 (or 1.0) mm drill bit for a 1.3 (or 1.0) mm screw. Insert a 1.3 (or 1.0) mm drill sleeve into the gliding hole.
Use a 1.0 (or 0.8) mm drill bit to drill a thread hole in the opposite fragment, just through the far (trans) cortex.
Leave the drill bit in the drill hole, preliminarily to hold the reduction if no K-wire has already been used for this purpose.
Remove the reduction forceps.
Screw size selection
The exact size of the diameter of the screw used will be determined by the fragment size and the fracture configuration.
The various gliding hole and thread hole drill sizes for different screws are illustrated here.
Screw length pitfalls
Ensure that a screw of the correct length is used.
- Too short screws do not have enough threads to engage the cortex properly. This problem increases when self-tapping screws are used due to the geometry of their tip
- Too long screws endanger the soft tissues, especially tendons and neurovascular structures. With self-tapping screws, the cutting flutes are especially dangerous, and great care has to be taken that the flutes do not protrude beyond the cortical surface.
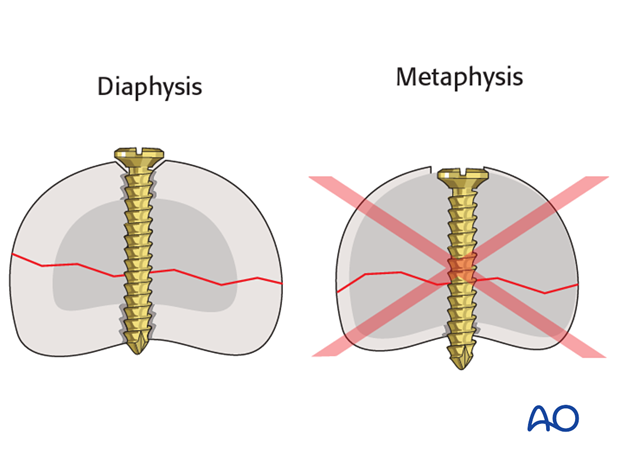
No countersinking in the metaphysis
Do not countersink the screws in the metaphysis as its cortex is very thin.
If countersinking is attempted, all purchase and compression may be lost due to screw-head breakthrough.
Drill for proximal screw
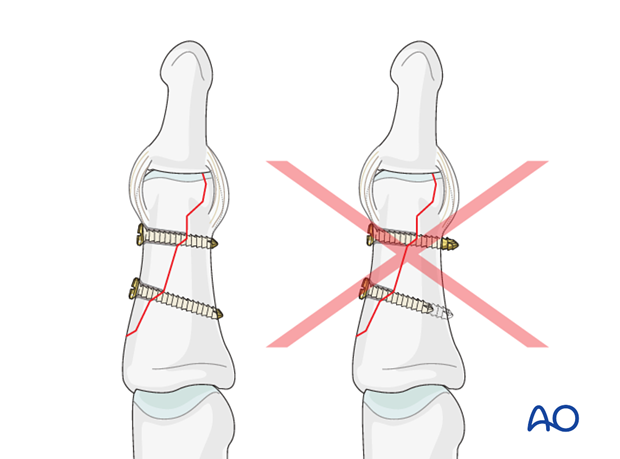
Towards the proximal apex of the fracture line, drill a gliding hole for a second lag screw. This screw, too, should be placed as perpendicularly to the fracture plane as possible, using a 1.3 (or 1.0) mm drill bit for a 1.3 (or 1.0) mm screw. Insert a 1.3 (or 1.0) mm drill sleeve into the gliding hole.
Use a 1.0 (or 0.8) mm drill bit to drill a thread hole in the opposite fragment, just through the far (trans) cortex.
Insert distal screw
Insert the distal lag screw. Do not completely tighten it at this time. The screw should penetrate the opposite cortex.
Insert proximal lag screw
Now insert the proximal lag screw. This screw, too, should penetrate the opposite cortex.
Alternate tightening of the two lag screws helps to avoid tilting of the fragment and applies even compression forces over the whole fracture surface.
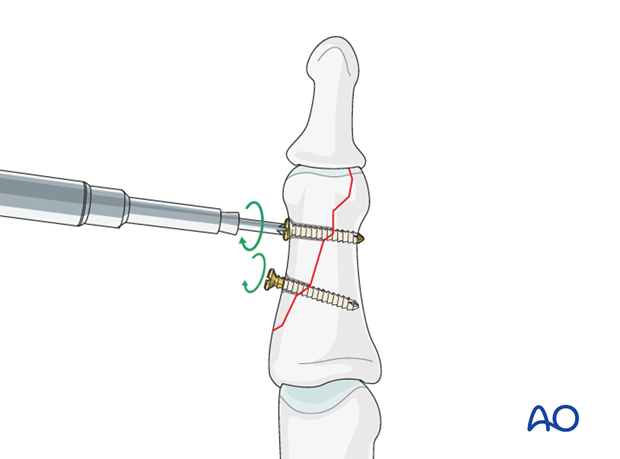
Check using image intensification. The reduction must be anatomical.
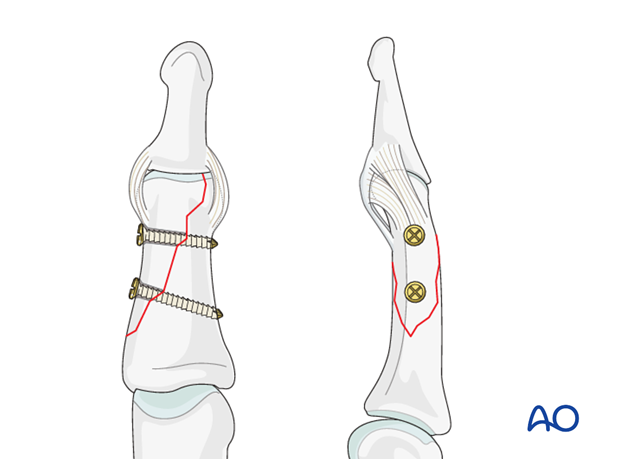
Check stability
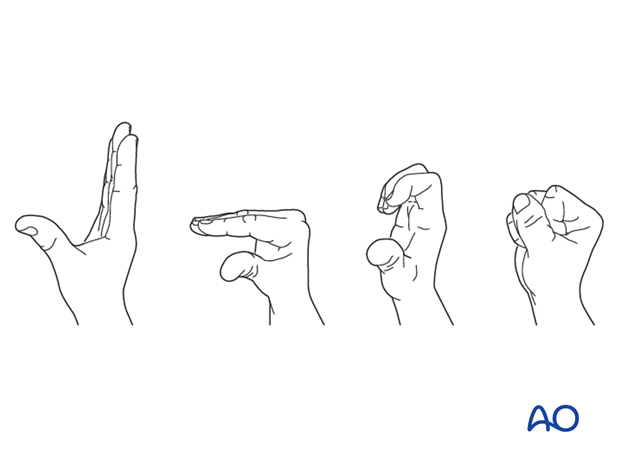
Check stability of the fixation by passive flexion and extension of the DIP joint, and by applying gentle lateral and rotational motion. This will help to determine stability in order to establish strategies for rehabilitation.
Caveat: Changing fracture plane
Hastings and Weiss described a fracture type in which the fracture plane changes between the condylar and metaphyseal zones.
In such a fracture configuration, it is important to observe that all the lag screws are inserted as perpendicularly to the local fracture plane as possible.
Be careful to confirm correct fracture planes under direct vision and in different radiographic views.
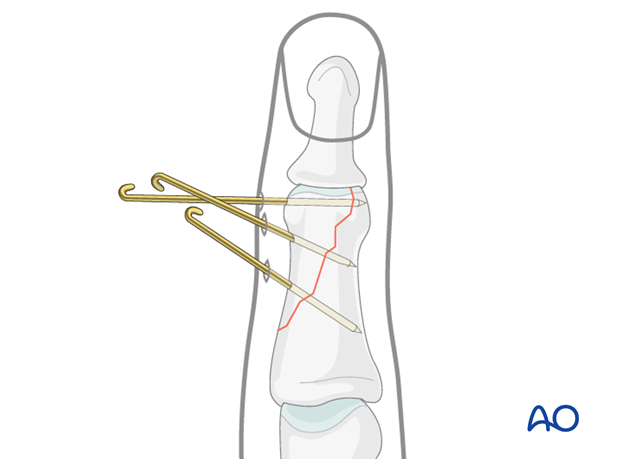
7. Alternative K-wire fixation
Comminuted fractures
Percutaneous K-wire fixation can be an easy-to-perform and cost-efficient alternative to lag screw fixation. However, the disadvantages of K-wire fixation remain, most notably less stability, lacking compression and the risk of displacement.
For K-wire fixation, introduce 2-3 unthreaded K-wires percutaneously, ensuring that they cross the fracture plane as perpendicularly as possible. To reduce the risk of displacement, insert the K-wires at diverging angles.
Confirm reduction using image intensification.
Cut the K-wire outside of the skin and bend them.
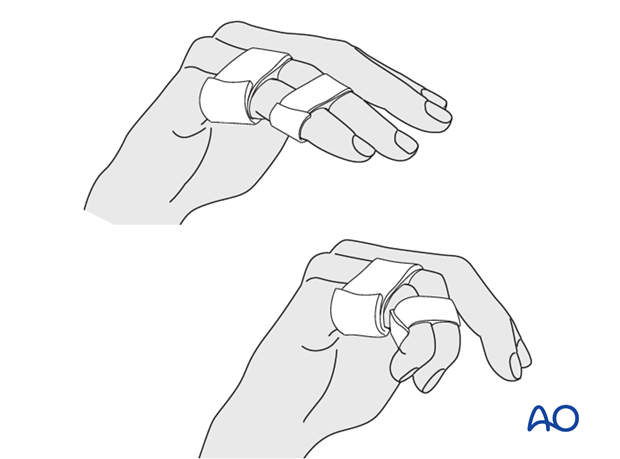
8. Aftertreatment
Postoperatively
Protect the digit with buddy strapping to the adjacent finger, to neutralize lateral forces on the finger.
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
After K-wire fixation
After K-wire fixation, the DIP joint has to be immobilized in extension, leaving the PIP joint free. Either an alumaform splint, or a custom-made thermoplastic splint can be used.
Remove K-wires after 3 weeks, keeping the splint for an additional 2 weeks.
Follow up
See the patient 5 days and 10 days after surgery.
Functional exercises
The patient can begin active motion (flexion and extension) immediately after surgery.
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.












