Distal, unicondylar
Fracture type
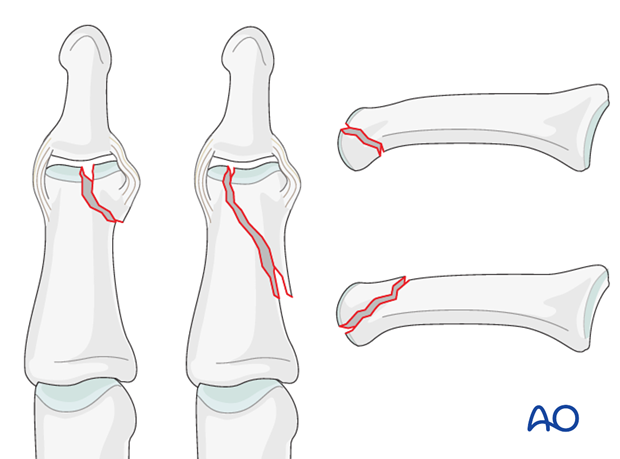
Unicondylar fractures of the middle phalanx can be transverse, oblique, (short or long), or comminuted. Typically they are the results of an axial load combined with lateral angulation of the finger.
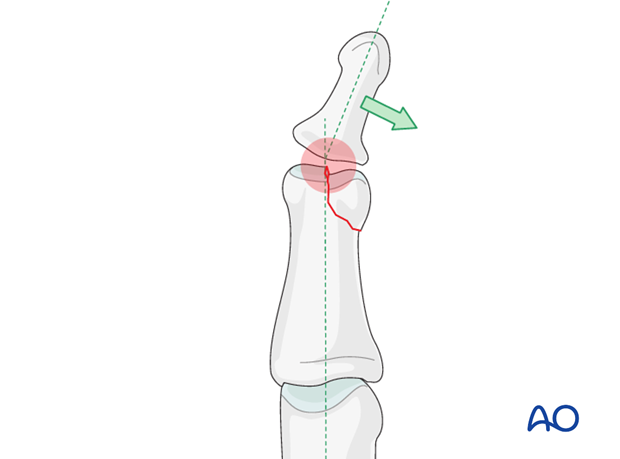
Condylar fractures tend to be unstable and need to be treated operatively. If conservative treatment is attempted, secondary displacement, leading to angulation of the finger, often occurs
Short and long oblique fractures
Short oblique fractures usually originate in the intercondylar notch.
Long oblique fractures more often pass through one of the condyles, splitting proximally towards the diaphyseal cortex on the side of the uninjured condyle.
Caveat
These fractures are rare, but difficult to treat. There is an increased risk of joint stiffness resulting from these fractures.
It is wise to use magnifying loupes in these procedures. Gentle and precise handling throughout the procedure is mandatory.
Anatomical reduction recommended
Although the DIP joint is somewhat forgiving, every effort should be made to reduce articular fractures anatomically, lest digital deformity and degenerative joint disease follow. This is difficult to achieve nonoperatively.
This illustration shows how minimal unicondylar depression may lead to angulation of the finger. Arthrodesis of the DIP joint, however, is a procedure with an acceptable outcome, without any major finger disability.
Outcomes
Outcome of fractures of the middle phalanx is usually more favourable than those of the proximal phalanx. This is largely due to the fact that limitation of DIP joint motion is not such a disability as similar stiffness of the PIP and MCP joints.
Consequences of malunion, or degenerative joint disease (pain, deformity) at the DIP joint)can be dealt with by arthrodesis, which is usually a procedure with an acceptable outcome.












