Nonoperative treatment
1. General considerations
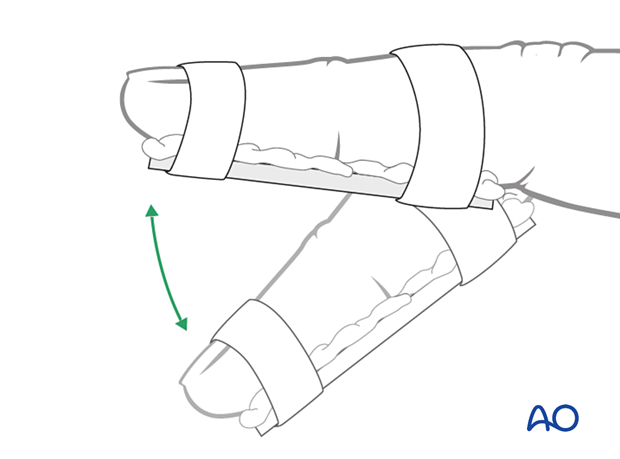
Nonoperative treatment is based on immobilization of the DIP joint in extension, leaving the PIP joint free.
2. Splinting
The DIP should be splinted distally from the PIP joint.
Dorsal splint vs palmar splint
Using a dorsal splint has the advantage of leaving the patient with the ability to pinch while the digit is immobilized.
However, proponents of palmar splinting argue that the palmar aspect is better cushioned than the dorsal and, thereby, can tolerate the splint better.
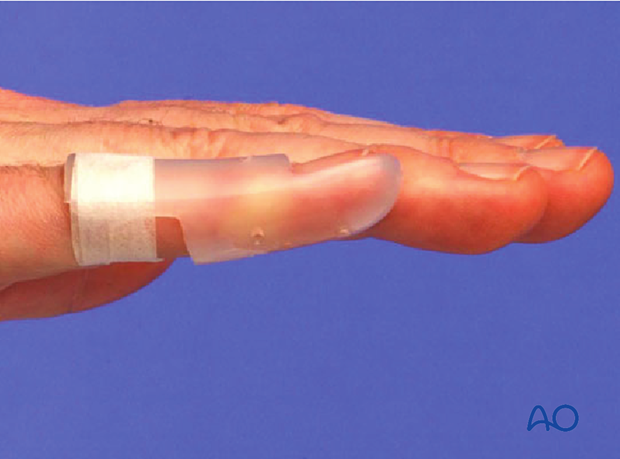
Contoured custom thermoplastic splint
The advantage of a custom thermoplastic splint is that it is adapted better to the shape of the finger and is easier to change.
3. Duration of immobilization
In the case of bony avulsion injuries, an x-ray should be performed with the splint applied to confirm that no displacement has occurred. The splint must be worn for at least 5 weeks when an x-ray is taken to check for bone healing.
In the case of a disruption of the tendon, the DIP joint should be immobilized in extension for 8 weeks. It must be impressed on the patient that the DIP joint must be kept in extension at all times, even when the splint is taken off for cleaning. It must be kept in mind that the vascularity of this area is precarious, even in healthy patients, and healing is slow–any shorter period of immobilization risks rerupture. Joint stiffness is unusual after these injuries.
Outcome
Frequently, patients may complain of a dorsal prominence and loss of the last 10°–20° extension of the DIP joint. Dorsal tenderness rarely persists for more than a month or so after the removal of the splint.
4. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Management of swelling
The arm should be actively elevated to help reduce any swelling.
Cleaning
Removal of the splint and skincare must be performed by the patient at weekly intervals.
Instruct the patient to keep the finger in extension by pinching it with the thumb when the splint is taken off for cleaning or by pressing the tip of the finger onto a tabletop.
Any flexing of the finger may disrupt the healing process.

Mobilization
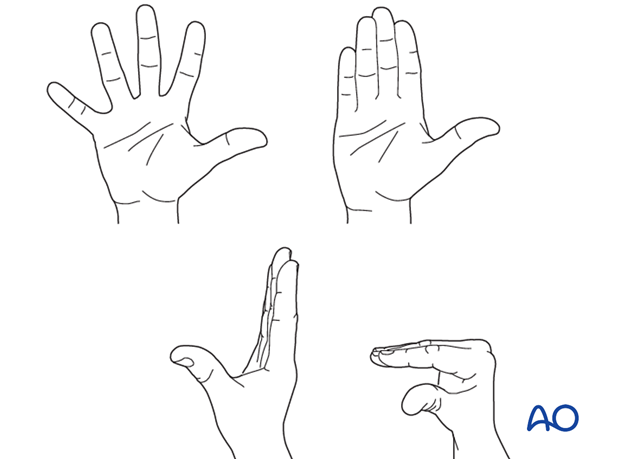
Hand therapy is recommended to prevent soft-tissue atrophy and joint contracture (typically extension of MCP joint and flexion of PIP joint), which leads to a poor outcome, and subsequent treatment is difficult.
Functional exercises of the nonimmobilized joints should be started immediately to keep uninjured joints mobile.
Follow-up
X-ray controls have to be performed immediately after the splint has been applied.
After 5 weeks, an x-ray without the splint is taken to confirm healing. Splinting can then usually be discontinued, and active mobilization is initiated.
If, after 8 weeks, x-rays confirm healing and the patient is painless, full loading can be permitted.













