Nonoperative treatment
1. General considerations
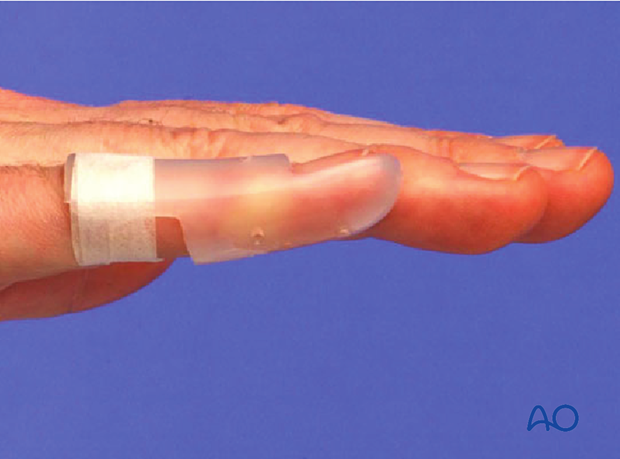
Nonoperative treatment is based on immobilization of the DIP joint in extension, leaving the PIP joint free.
Nail bed injuries may need repair and reduction of the nail plate into the nail fold.
AO Teaching video
Removable finger splint using synthetic
2. Closed reduction
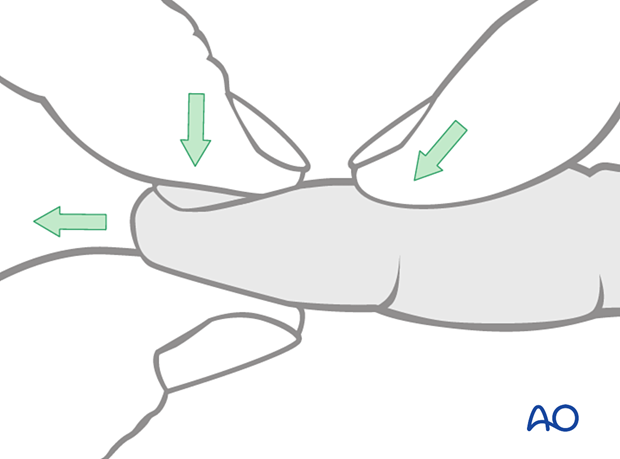
Reduction of dorsal subluxation
Most dorsal dislocations can be reduced by applying traction, flexion, and dorsal pressure on the base of the distal phalanx.
If the joint is stable after reduction, nonoperative treatment is usually indicated.
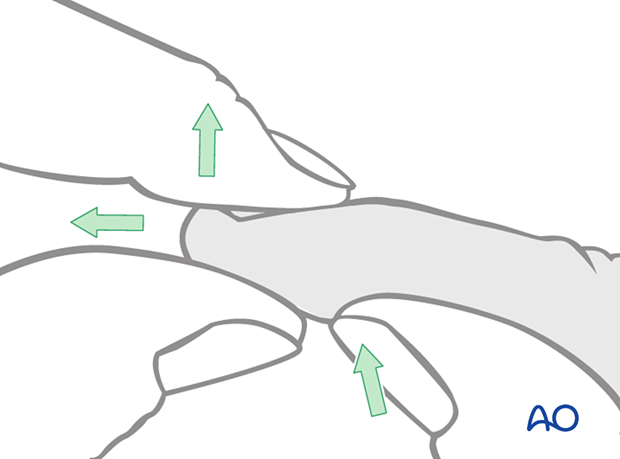
Reduction of palmar subluxation
In the case of a palmar dislocation, apply traction and extension. Then apply pressure with the thumb on the palmar aspect of the base of the distal phalanx.
Rarely, the terminal extensor tendon, or the flexor digitorum profundus, may be interposed in the DIP joint. This is an indication for ORIF.
If the joint is stable after reduction, nonoperative treatment is usually indicated.
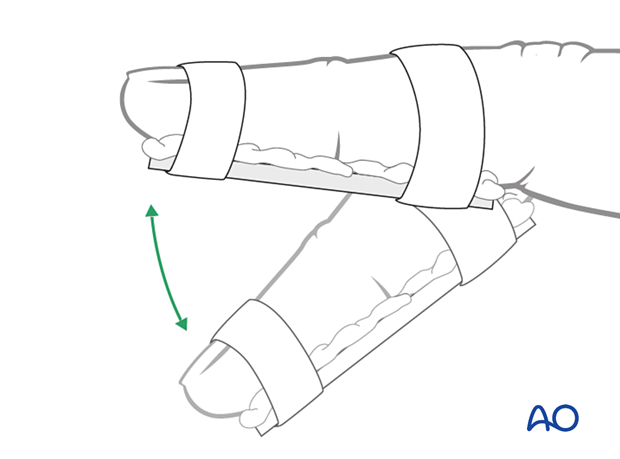
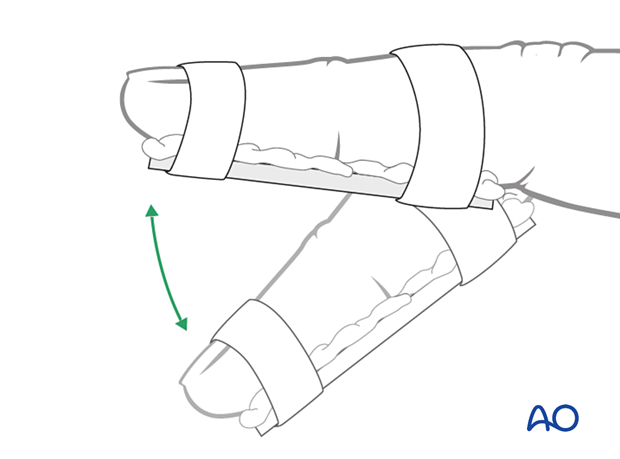
3. Splinting
The DIP should be splinted distally from the PIP joint.
Dorsal splint vs palmar splint
Using a dorsal splint has the advantage of leaving the patient with the ability to pinch while the digit is immobilized.
However, proponents of palmar splinting argue that the palmar aspect is better cushioned than the dorsal and, thereby, can tolerate the splint better.
Contoured custom thermoplastic splint
The advantage of a custom thermoplastic splint is that it is adapted better to the shape of the finger and is easier to change.
4. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Management of swelling
The arm should be actively elevated to help reduce any swelling.
Cleaning
Removal of the splint and skincare must be performed by the patient at weekly intervals.
Mobilization
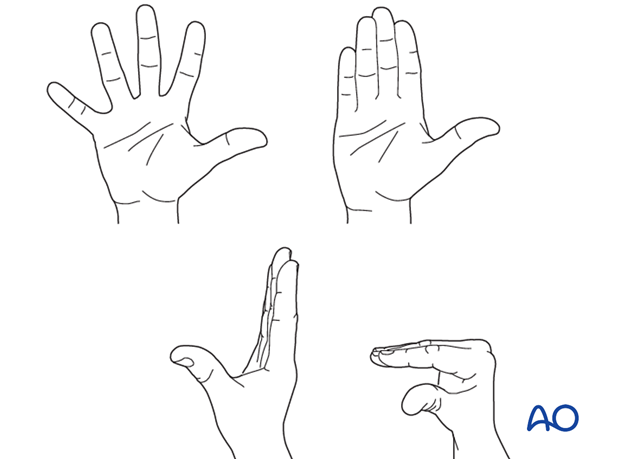
Hand therapy is recommended to prevent soft-tissue atrophy and joint contracture (typically extension of MCP joint and flexion of PIP joint), which leads to a poor outcome, and subsequent treatment is difficult.
Functional exercises of the nonimmobilized joints should be started immediately to keep uninjured joints mobile.
Follow-up
X-ray checks of joint position must be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week and, if necessary, after 2 weeks.
Immobilization is continued until about 4 weeks after the injury. At that time, an x-ray may be taken to confirm healing. Splinting can then usually be discontinued, and active mobilization is initiated.
In the absence of pain during functional activities, full manual loading can be permitted. In case of doubt, an x-ray to confirm healing and consolidation, which would be expected by 8 weeks, should be taken.













