Joint transfixation with K-wire
1. General considerations
Introduction
Transfixation of the DIP joint with a K-wire is indicated if the joint remains unstable after closed reduction.
Potential risks of percutaneous pinning
The commonest risk of percutaneous K-wire immobilization is infection.
Breakage of the K-wire at the level of the DIP joint can be avoided by using a wire of 1.6 or 1.8 mm diameter and counseling the patient to avoid stresses at the DIP joint. The fixation should be protected with a splint to reduce the risk of wire breakage.
2. Patient preparation
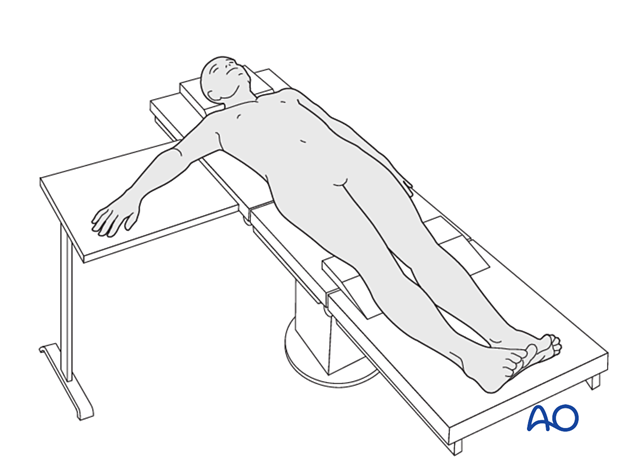
This procedure is usually performed with the patient in a supine position with the arm on a radiolucent side table.
3. Closed reduction
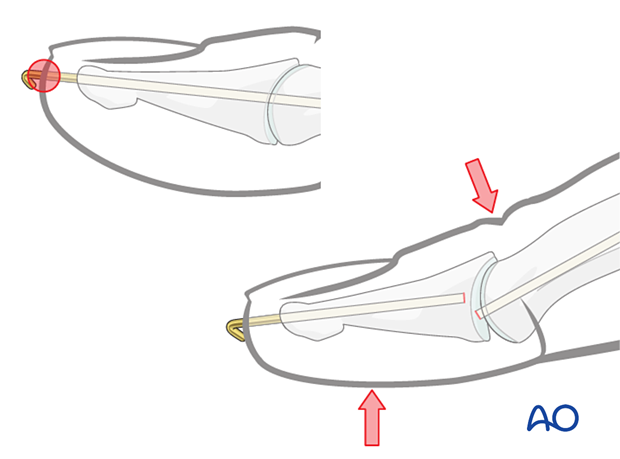
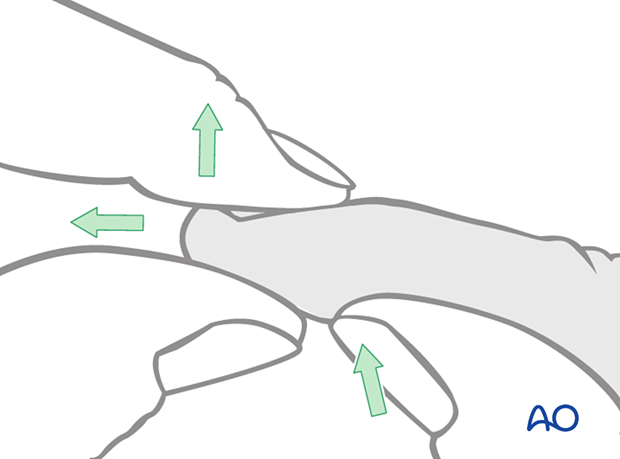
Reduction of dorsal subluxation
Most dorsal dislocations can be reduced by applying traction, flexion, and dorsal pressure on the base of the distal phalanx.
If the joint is stable after reduction, nonoperative treatment is usually indicated.
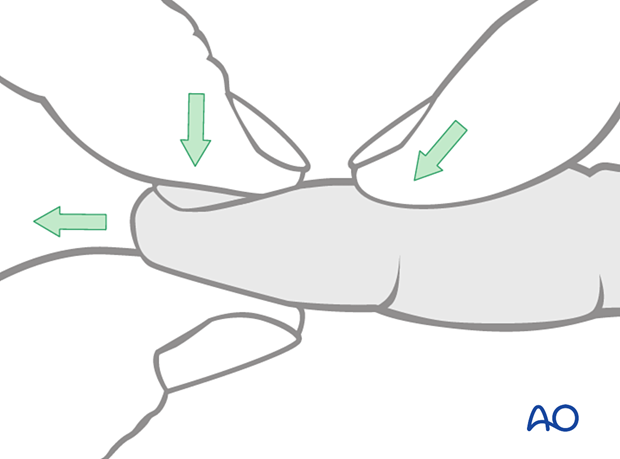
Reduction of palmar subluxation
In the case of a palmar dislocation, apply traction and extension. Then apply pressure with the thumb on the palmar aspect of the base of the distal phalanx.
Rarely, the terminal extensor tendon, or the flexor digitorum profundus, may be interposed in the DIP joint. This is an indication for ORIF.
If the joint is stable after reduction, nonoperative treatment is usually indicated.
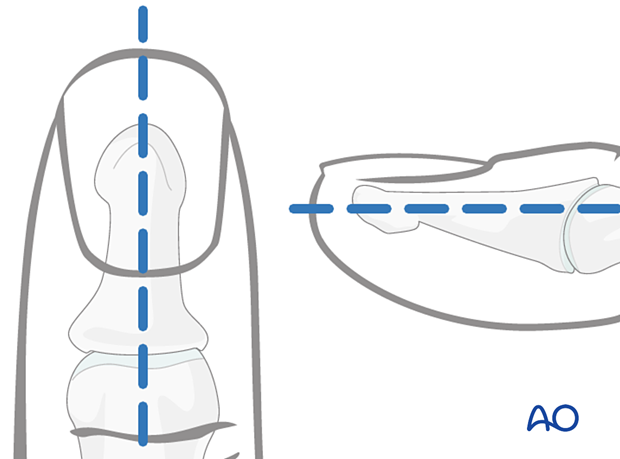
4. Marking K-wire track
To avoid unnecessary radiation from image intensification, mark the planned track of the K-wire on the distal phalanx in both the AP and the lateral aspects.
5. Fixation
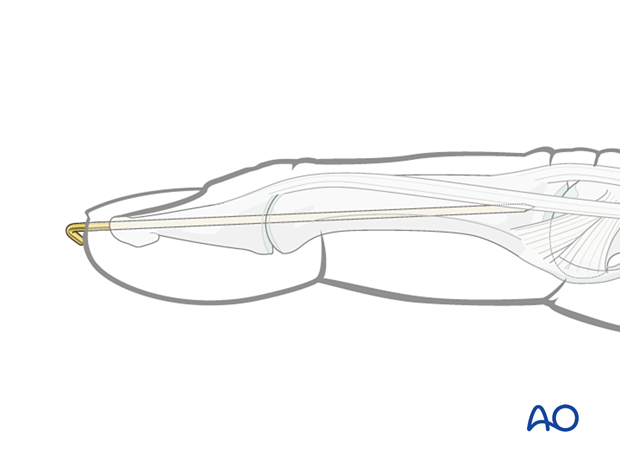
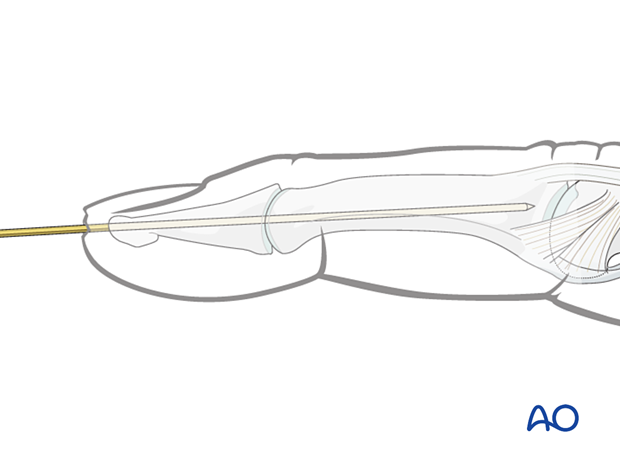
Closed reduction with K-wire
Insert the K-wire through the tip of the distal phalanx up to the DIP.
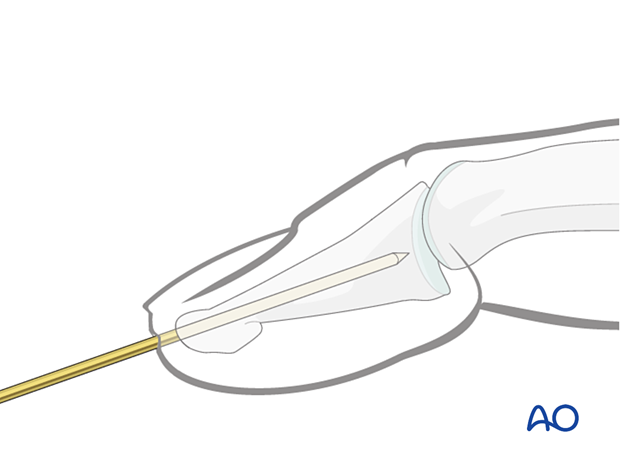
Carefully reduce the joint by extending the DIP joint.
Confirm DIP joint reduction with an image intensifier in the lateral view.
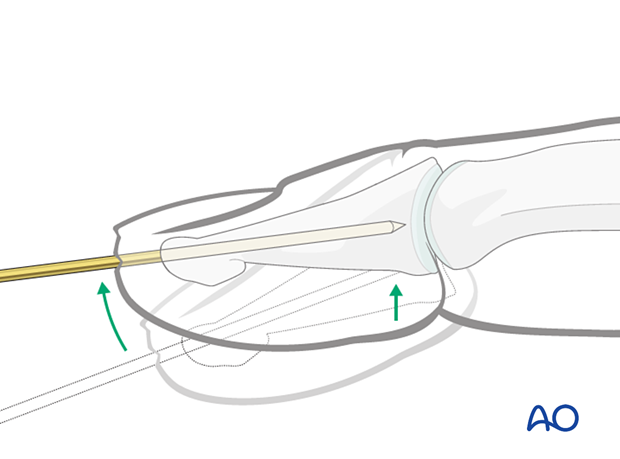
Joint transfixation
Advance the K-wire across the DIP joint into the middle phalanx as far as its base. Be careful not to penetrate the PIP joint.
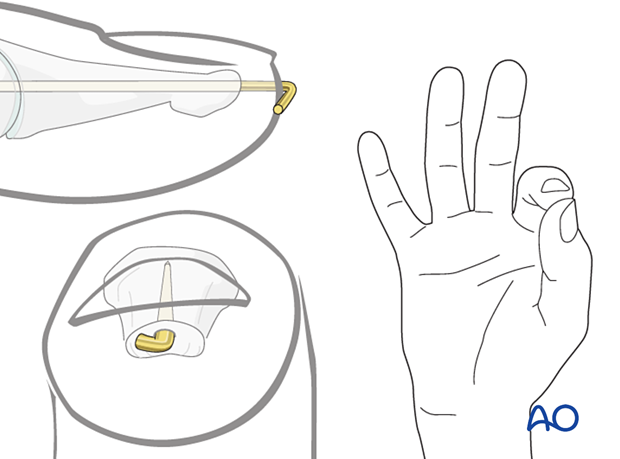
Cutting the K-wire
Cut the K-wire so that it protrudes through the skin. Bend its end to form an L-configuration to prevent catching on clothing, etc. The tip of the bent wire can be rotated towards the ulnar side to avoid interfering with pinch grip, which involves the radial side of the pulp.
Leaving the K-wire to protrude through the skin in this way has the advantage of its being easy to remove. The disadvantages are patient discomfort and risk of pin-track infection.
Make sure that the bent end does not irritate or compress the skin.
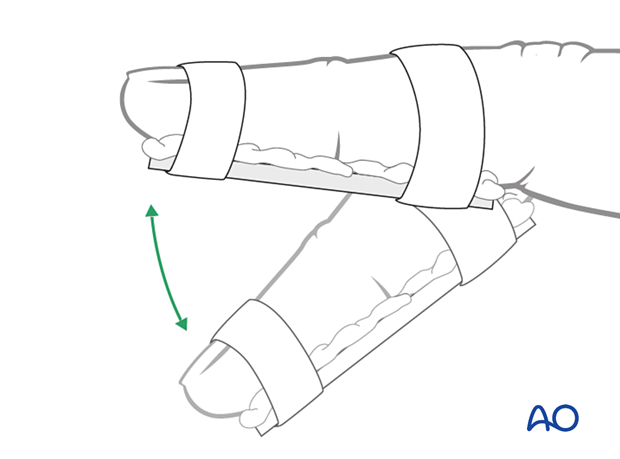
6. Immobilization
The fixation should be protected with a splint, leaving the PIP joint mobile, to reduce the risk of wire breakage.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Management of swelling
The arm should be actively elevated to help reduce any swelling.
Mobilization
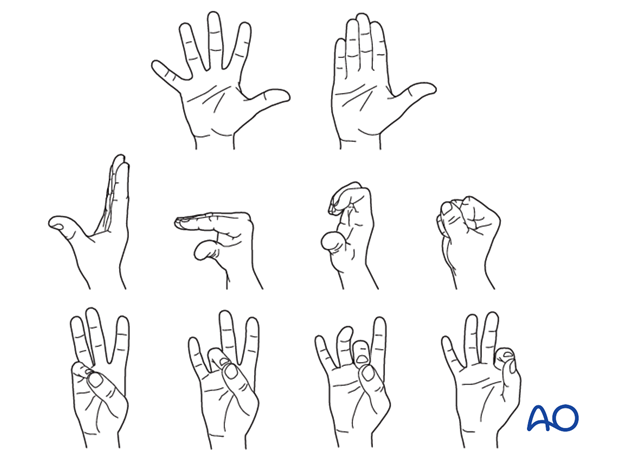
Hand therapy is recommended to prevent soft-tissue atrophy and joint contracture (typically extension of MCP joint and flexion of PIP joint), which leads to a poor outcome, and subsequent treatment is difficult.
Functional exercises of the nonimmobilized joints should be started immediately to keep uninjured joints mobile.
Active motion of the DIP joint is permitted after removal of the K-wire. Passive motion should be postponed for 8–10 weeks to avoid the risk of recurrent mallet deformity.
K-wire removal
After dorsal dislocation, the K-wire can be removed after 4–6 weeks.
After palmar dislocation, the K-wire can be removed after 6–8 weeks.













