Simple fracture of the diaphysis and distal end segment
Definition
Simple fractures of the shaft and tuft are classified by the AO/OTA as 78.2–5.3.2A, where 2–5 indicates the finger involved.
Fractures may be transverse or short oblique.
Further characteristics
Fractures of the distal phalanx are the most common fractures in the hand.
Most fractures of the distal phalangeal diaphysis are closed and either undisplaced or minimally displaced.
Transverse fractures are often unstable, and in open fractures, the nail bed is often folded into the fracture.
Most of these fractures result from direct impact or crush injuries with associated soft-tissue (nail bed or pulp) lacerations.
Common complications of these injuries are:
- Altered sensibility (numbness, hyperesthesia, tenderness)
- Cold hypersensitivity (cold intolerance)
- Restriction of DIP joint movement
- Nail growth abnormalities
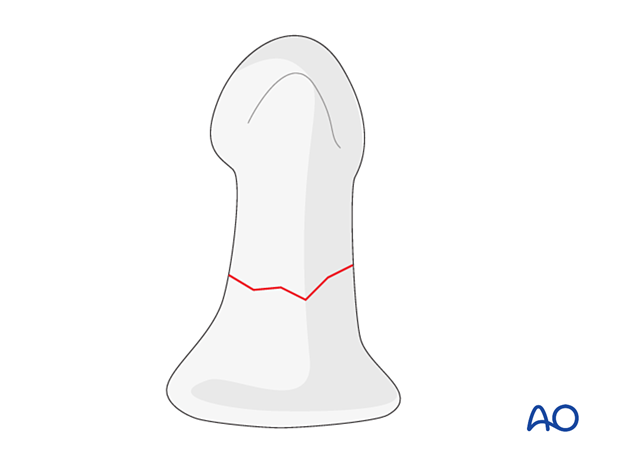
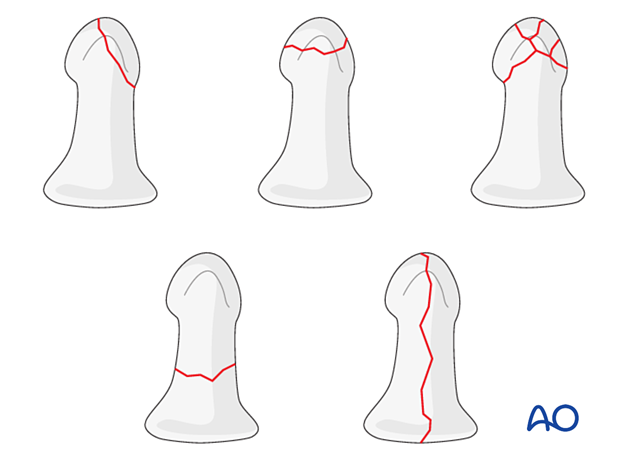
Classification of distal phalangeal fractures (after Schneider)
Schneider divides distal phalangeal fractures into tuft, shaft, and articular fractures.
Tuft fractures include
- Simple fractures
- Comminuted fractures
Shaft fractures include
- Transverse fractures
- Longitudinal fractures (may extend to involve the DIP joint)
Articular fractures include
- Palmar (flexor digitorum profundus avulsion fractures)
- Dorsal (extensor avulsion, mallet fractures)
Imaging
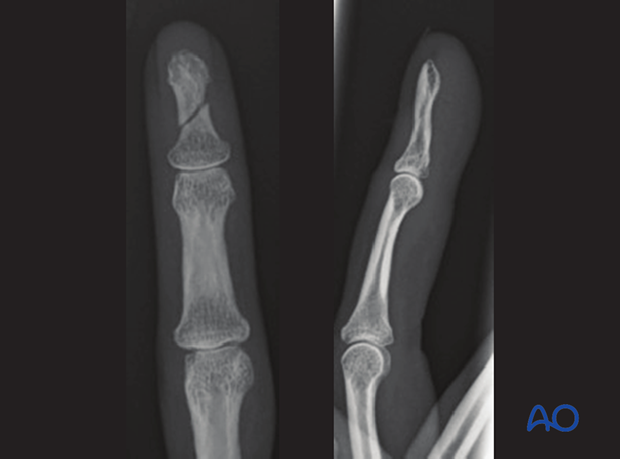
AP and lateral view x-rays of an oblique shaft fracture