Palmar approach to the DIP joint
1. Indications
The palmar approach to the distal interphalangeal (DIP) joint is indicated for avulsion fractures of the palmar base of the distal phalanx caused by the insertion of the profundus tendon.
AO teaching video
Finger, Distal Interphalangeal Joint (DIP), Palmar Approach
This video shows the palmar approach to the DIP joint.
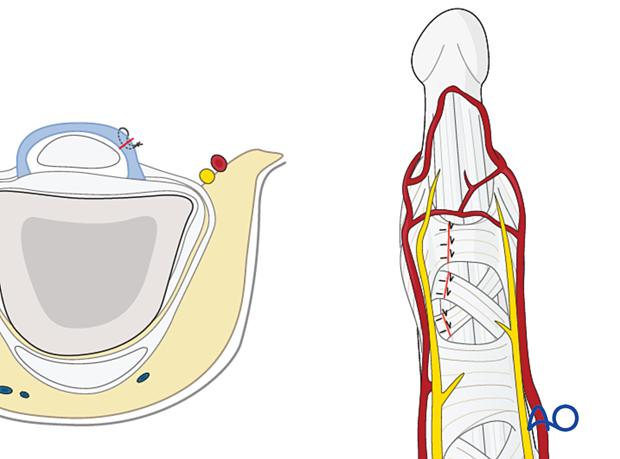
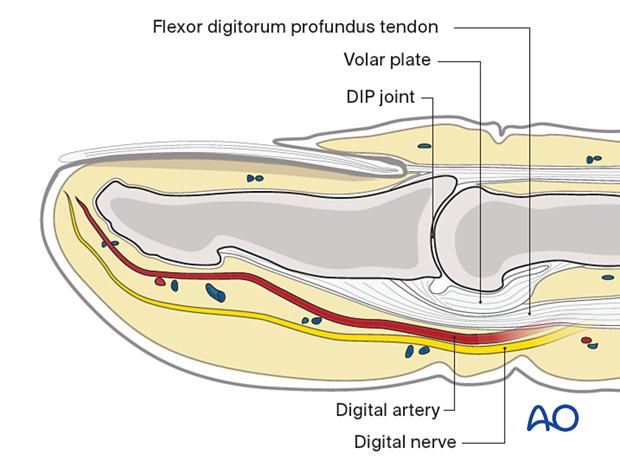
2. Surgical anatomy
The base of the distal phalanx has a prominent dorsal crest at the insertion of the extensor tendon. The tendon is also adherent to the DIP joint capsule.
On the palmar surface is the insertion of the flexor digitorum profundus tendon. This is also adherent to the volar plate.
The flexor tendon occupies the whole width of the base of the distal phalanx. It is made up of two different fibers. The superficial fibers attach to the lateral aspects of the phalanx. The deep fibers run centrally and attach more distal in the palmar aspect of the phalanx.
The volar plate is very flexible, allowing hyperextension of the DIP joint and pulp-to-pulp pinch.
The vascularity of the extensor tendons is more precarious than that of the flexor tendons. This prolongs extensor tendon healing time.
The digital nerve and artery should be identified and protected.
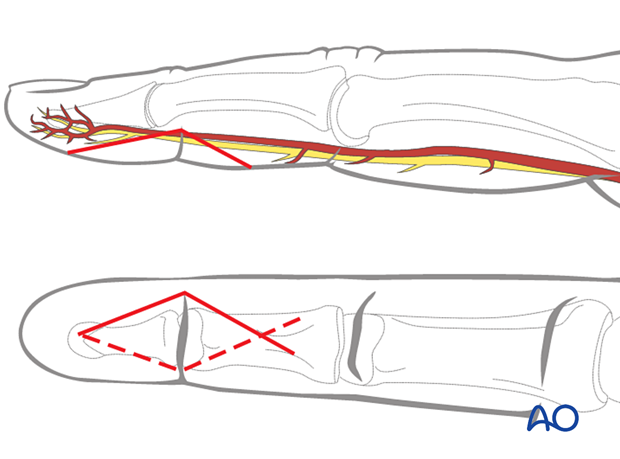
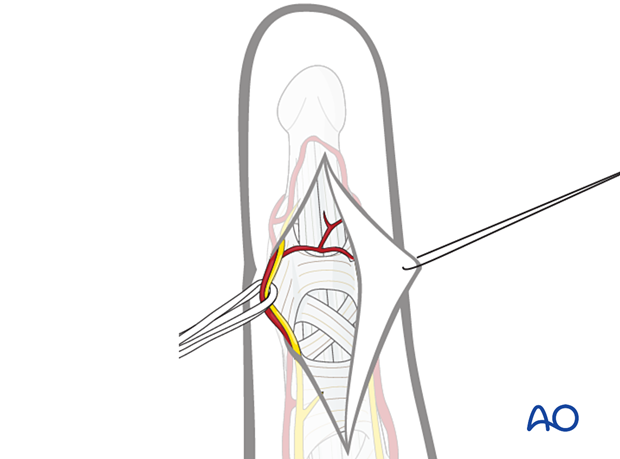
3. Skin incision
Make a carefully planned palmar angled skin incision (Bruner zigzag), using the flexor skin crease as a guide, as illustrated. The apex of the angle should be at the distal flexor crease, level with the DIP joint.
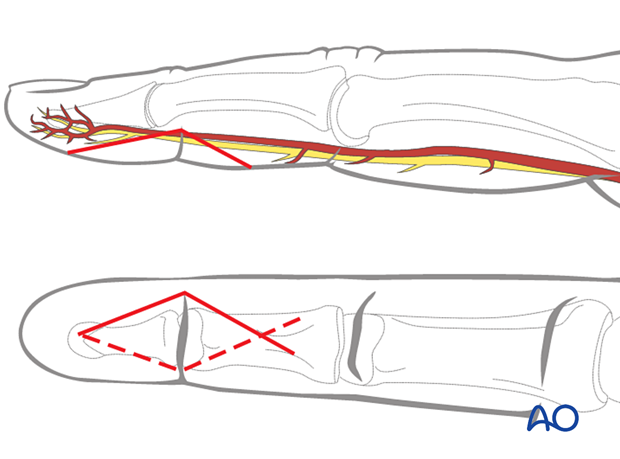
Elevate the angled skin flap by blunt dissection in the thin subcutaneous tissue, and retract the apex using a fine stitch. Identify and gently mobilize the digital arteries and nerves.
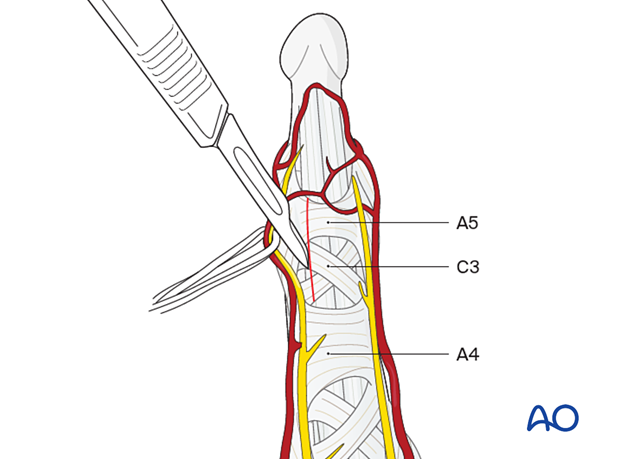
The flexor tendons and the C3 and A5 pulleys are now visible.
4. Blunt dissection
Make a blunt dissection of the pulp.
Divide the A5 and C3 pulleys laterally near their bony attachments, leaving enough for later reattachment (at least 2 mm).
Do not cut the A4 pulley, as it is essential for active finger flexion.
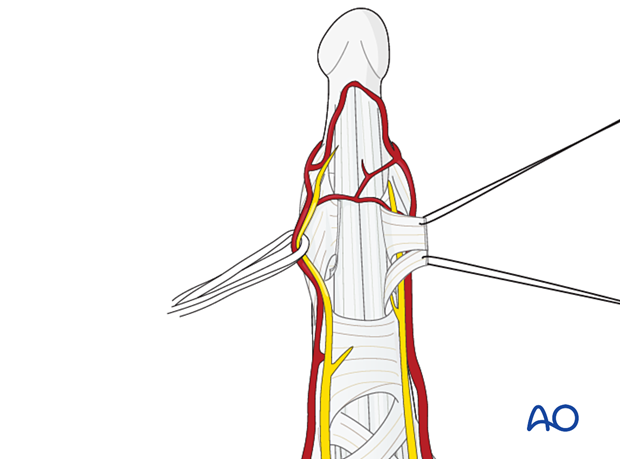
5. Elevation of the pulley flap
Elevate the pulley flap and retract it with a fine suture to expose the deep flexor tendon. By retraction of the tendon, the palmar aspect of the DIP joint and the distal phalanx is exposed.
6. Wound closure
Reattach the A5 and C3 pulleys using fine mattress sutures before skin closure.
Close the skin in a standard manner.