Recurrent osteomyelitis
1. Recurrent osteomyelitis
Principles
Neglected fracture-site infections may manifest themselves intermittently, with episodes of symptomatic inflammation (pain, redness, swelling and perhaps the development of a discharging sinus), separated by periods of reasonable comfort and function.
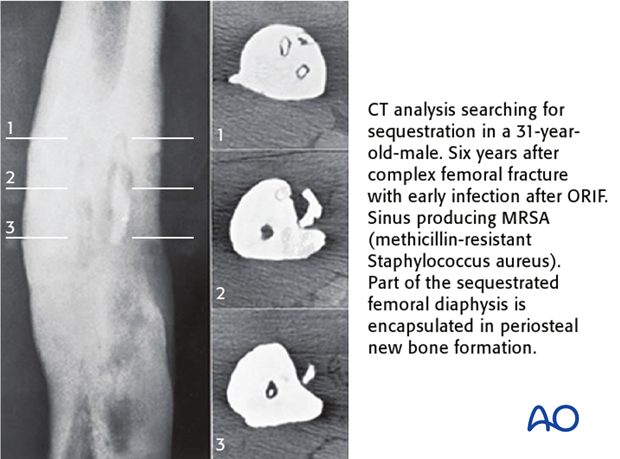
If the fracture is united and the patient is functional, the primary goal is to heal the infection. Recurrence is usually due to a persisting collection of biofilm bacteria, typically around fixation hardware, or to the presence of necrotic bone. A necrotic fragment (sequestrum) may lie adjacent to, or within, the previously fractured bone. If hardware is present, its removal is almost always essential. A sequestrum may be hidden under a retained plate, or be hard to find adjacent to an intramedullary nail. If a sinus is present, it will often lead to the source of recurrent infection. Cross-sectional imaging (CT, or MRI) helps to detect and locate sequestra and necrotic bone. It will be more informative after any hardware has been removed.
Treatment
Microbiological cultures of the infected tissues, (or PCR), are essential for correct identification of the responsible bacteria and appropriate choice of antibiotics. See General introduction.
Very occasionally, an early recurrence of infection can be aborted with prompt intensive antibiotic treatment. Perhaps the best guides for choosing an antibiotic, if available, are the results of cultures from previous recurrences. Such a trial of antibiotics should be considered, if a patient presents in the early stages of recurrence, prior to wound breakdown, or is not fit for surgical exploration.
If the infected fracture has not united (infected or septic non-union), two approaches can be followed:
- Treat infection first, then the nonunion (two stage approach)
- Treat infection and non-union simultaneously (single stage approach). More recently, authors have reported increasing success with the single stage approach.
Pearls
Whereas in acute haematogenous osteomyelitis, treatment with antibiotics alone can be considered, fracture wound infection always requires surgery, and antibiotics are to be regarded as adjuvant therapy.













