Ulnar and median nerve lesions
1. Introduction
Ulnar and median nerves are crucial structures in the hand, responsible for sensation and motor function. Their lesions can significantly impact daily activities and require prompt diagnosis and operative management.
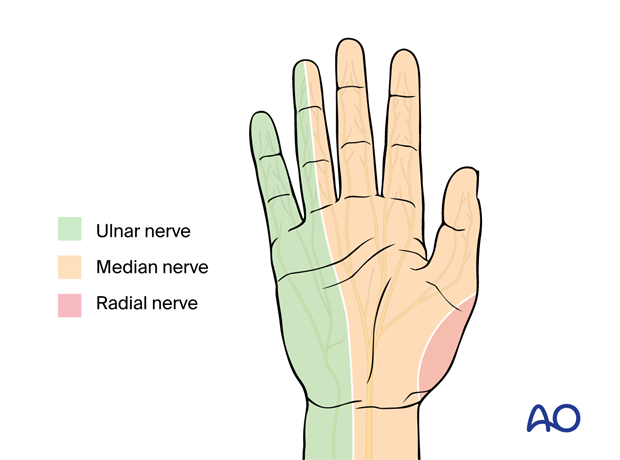
The ulnar nerve serves sensation on the ulnar side of the hand and motor function for power and pinch grip.
The median nerve serves sensation to the thumb and radial side of the hand and motor function for tripod grip.
Both nerves provide for opposition of the thumb.
If there is an injury at the carpal tunnel, symptoms will comprise loss of sensation and impairment of the motor branch of the median nerve to the thumb.
A more proximal median nerve injury including compression under the lacertus fibrosis (lacertus syndrome) will result in more motor impairment.
An isolated anterior interosseous nerve injury results in weakness of flexor carpi radialis (FCR), flexor pollicis longus (FPL), and flexor digitorum profundus (FDP) of the index.
2. Patient assessment
History
The following should be determined:
- Mechanism of injury
- Time of onset
- Sensory loss including numbness, tingling, pain
- Associated bone and soft-tissue injuries
Physical examination
- Assess the soft tissue injury for the likely site of digital nerve injury
- Observe for sensory deficits using light touch, temperature, and two-point discrimination for each nerve’s territory
- Assess for Tinel's sign
- Assess for carpal tunnel syndrome.
- Assess for Guyon’s canal syndrome.
- Assess for motor deficits.
The median nerve is particularly at risk of injury in perilunate and lunate dislocations, and distal radial fractures. Acute carpal tunnel syndrome can be a feature of these injuries.
The ulnar nerve is particularly at risk of injury in fractures of the hamate (Guyon’s canal syndrome).
Assessment of ulnar nerve motor deficits
Check the power of abductor digiti minimi …
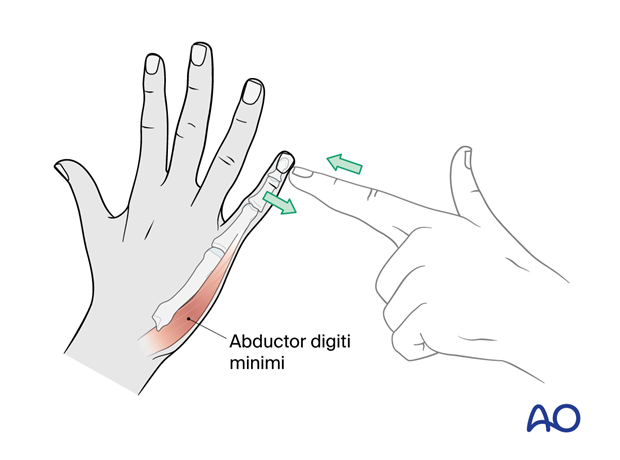
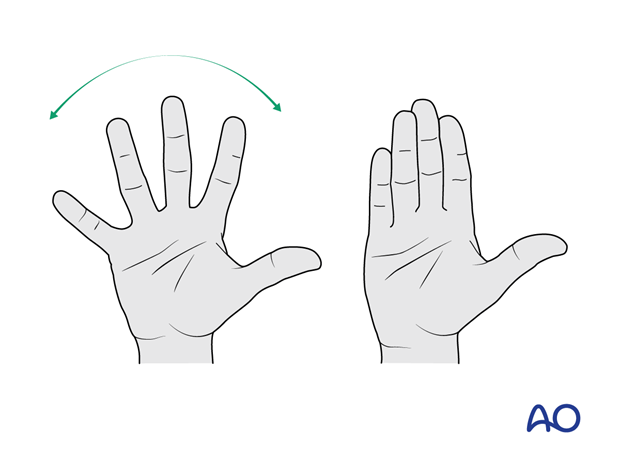
… and the interossei.
Assess for proximal ulnar nerve lesions by examining for loss of function of the FDP of the 4th and 5th fingers and flexor carpi ulnaris (FCU).
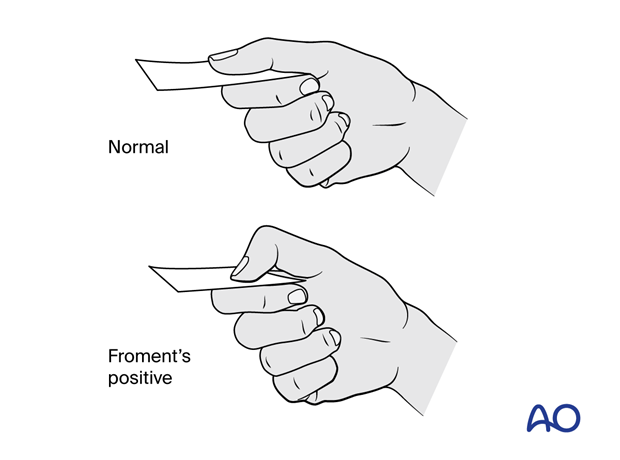
Check for Froment’s sign. There will be a hyperflexion of the IP joint during key pinch because the thumb adductor is weak, and pinch is done by hyperflexing the thumb tip (median nerve). If the adductor pollicis is weak, Froment’s sign is positive.
Assessment of distal median nerve motor deficits
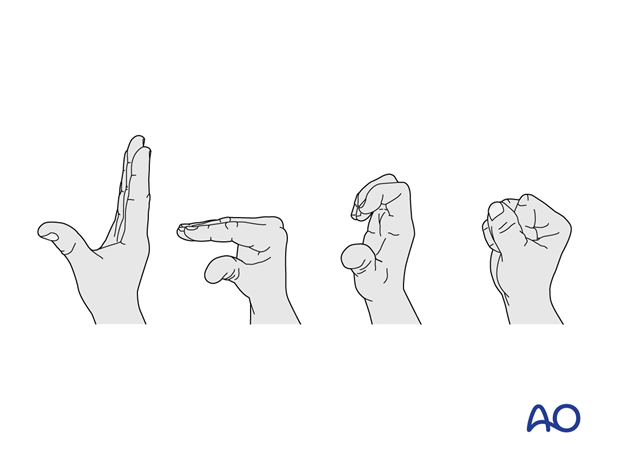
Assess the power of tripod grip.
Weakness of the opponens pollicis or FDP of the index and middle fingers or both will result in weakness of tripod or pinch grip.
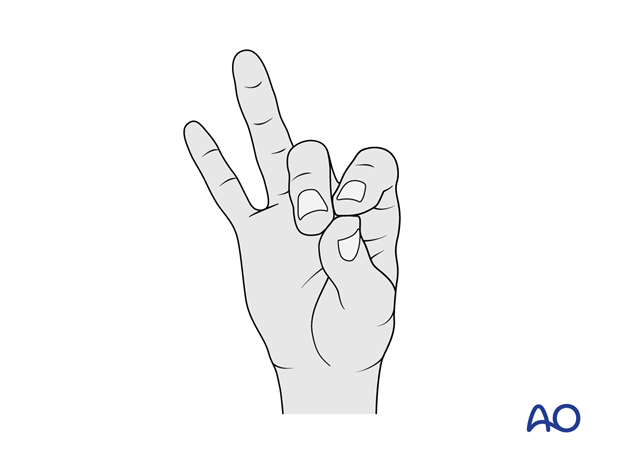
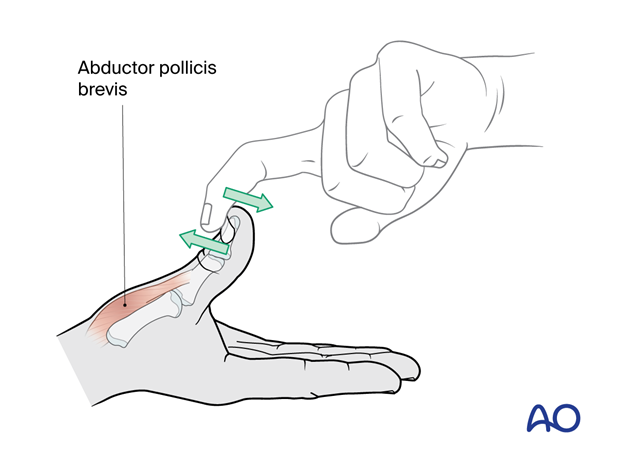
Check the power of the abductor pollicis brevis (APB) by abducting the thumb against resistance.
3. Management
- Preoperative splinting is used to immobilize the injured hand to prevent further nerve retraction and promote healing.
- Associated fractures and dislocations should be addressed before the management of the nerve lesion. Surgical approaches should be selected to address both fracture and nerve injury management.
- Exploration and primary nerve repair are indicated for complete lacerations and transections.
- Neurolysis is used to release scar tissue compressing the nerve.
- Nerve grafting is used if primary repair of a large gap is not possible.
Coaptation (nerve repair)
Most commonly coaptation is performed using operating microscope or loupe magnification.
The size of sutures used depends on the size of the nerve and surgeon’s preference.
Generally, an epineural repair is performed. Proximal injuries may allow for a fascicular repair, while this is not an option for distal injuries.
Fascicular repair together with epineural repair may improve reinnervation.
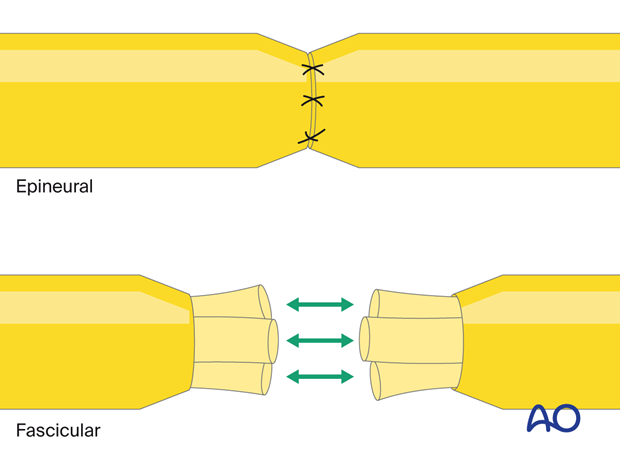
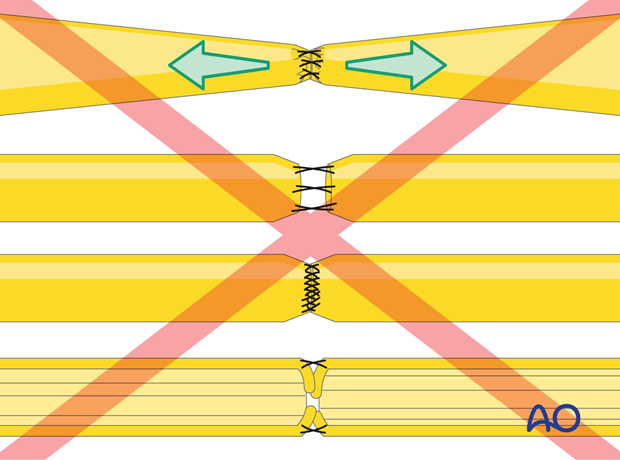
The following considerations should be considered for optimal nerve coaptation:
- The ends should have enough laxity for apposition without tension.
- There should be no gap at the repair site.
- The least number of sutures that allow for adequate approximation (2–4) should be used.
- Avoid epineural tissue interposition at the coaptation site.
Some centers use fibrin glue instead of sutures.
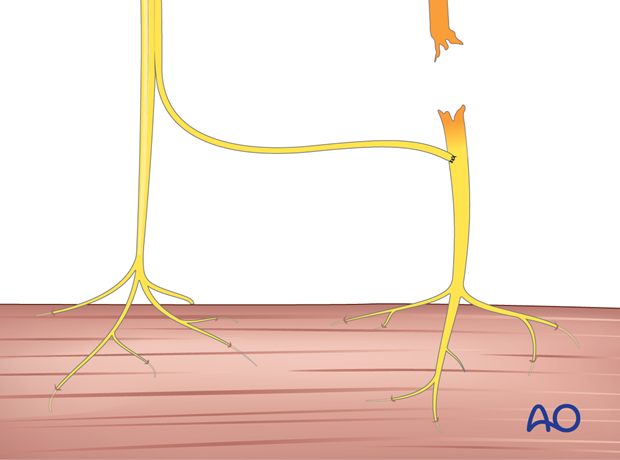
If the nerves cannot be coapted without tension, nerve graft should be considered.
Alternatively, vein graft or synthetic neurotubes may be used.
Nerve grafting
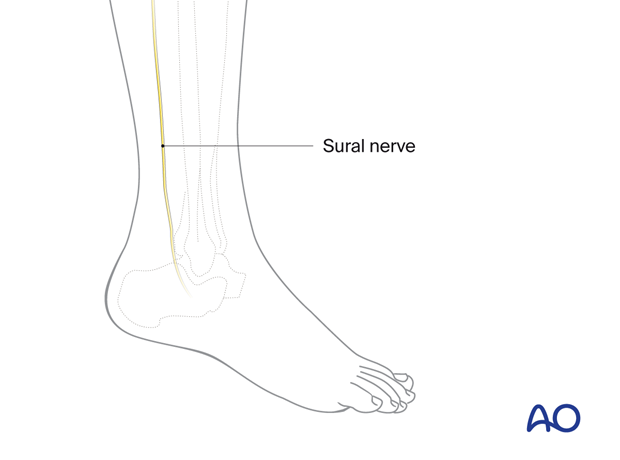
Sensory nerves are routinely used for grafting, as they cause less functional deficits. The most common sensory nerve used is the sural nerve.
Other options are the medial or lateral antebrachial nerves.
The selected nerve is harvested.
4. Healing and Rehabilitation
Nerve regeneration is a slow process, averaging 1 mm/day.
Functional recovery can be enhanced by a specialized hand habilitation program. This would include:
- Rehabilitation of the fracture and dislocation should follow the usual principles.
- Sensory retraining; techniques to enhance the restoration of protective sensation followed by discriminatory sensation
- Occupational therapy to address functional limitations and return to daily activities
In cases of absent motor reinnervation after repair of proximal motor nerves, consider referring the patient to a peripheral nerve surgeon for evaluation of selective nerve transfer surgery which should be performed within 10–12 month post injury.
5. References
- Jaquet JB, Luijsterburg AJ, Kalmijn S, et al. Median, ulnar, and combined median-ulnar nerve injuries: functional outcome and return to productivity. J Trauma. 2001 Oct;51(4):687–692.
- Jaquet JB, Kalmijn S, Kuypers PD, et al. Early psychological stress after forearm nerve injuries: a predictor for long-term functional outcome and return to productivity. Ann Plast Surg. 2002 Jul;49(1):82–90.
- Jones NF, Machado GR. Tendon transfers for radial, median, and ulnar nerve injuries: current surgical techniques. Clin Plast Surg. 2011 Oct;38(4):621–642.
- Kilinc A, Ben Slama S, Dubert T, et al. Résultats de la réparation primaire des plaies du nerf médian et du nerf ulnaire au poignet [Results of primary repair of injuries to the median and ulnar nerves at the wrist]. Chir Main. 2009 Apr;28(2):87–92. French.
- Murovic JA. Upper-extremity peripheral nerve injuries: a Louisiana State University Health Sciences Center literature review with comparison of the operative outcomes of 1837 Louisiana State University Health Sciences Center median, radial, and ulnar nerve lesions. Neurosurgery. 2009 Oct;65(4 Suppl):A11–17.
- Nouraei MH, Hosseini A, Salek S, et al. Median and ulnar nerve injuries; what causes different repair outcomes? Adv Biomed Res. 2015 Sep 28;4:215.
- Ruijs AC, Jaquet JB, Kalmijn S, et al. Median and ulnar nerve injuries: a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plast Reconstr Surg. 2005 Aug;116(2):484–494; discussion 495-496.
- Tan RES, Jeyaratnam S, Lim AYT. Updates in peripheral nerve surgery of the upper extremity: diagnosis and treatment options. Ann Transl Med. 2023 Oct 25;11(11):391.













