Gluteal compartment syndrome
1. Introduction
Compartment syndrome is a true surgical emergency.
It is caused by increasing tissue pressure which prevents capillary blood flow, leading to ischemia in muscle and nerve tissue.
If not treated, tissue necrosis with permanent loss of function may occur.
Compartment syndrome may occur as a result of:
- high-energy limb injuries
- crushing injuries
- reperfusion injury
- burns
Compartment syndrome occurs in:
- fascial compartments below the elbow
- fascial compartments below the knee
- rarely, above the elbow and knee
Treatment of compartment syndrome requires surgical release of the closed osteo-fascial compartments.
2. Definition
Compartment syndrome is characterized by a rise in pressure within a closed fascial compartment, sufficient to prevent effective capillary perfusion in muscle and nerve tissue.
Normal tissue pressure is 0–10 mm Hg. The capillary filling pressure is essentially diastolic arterial pressure. When tissue pressure approaches the diastolic pressure, capillary blood flow ceases.
3. Diagnosis
Symptoms
Diagnosis requires a high index of suspicion and appreciation of progressively severe symptoms which include the following:
- unexpected pain with increasing analgesia requirement
- paresthesia
- progressive loss of sensation
- progressive loss of power
The diagnosis is difficult in patients with:
- head injury
- loss of consciousness for other reasons
- high spinal injury
- regional nerve blockade
Signs
The signs of an evolving compartment syndrome include:
- tenderness and swelling of the affected compartment
- increase in pain with passive muscle stretching
- compartmental muscle weakness
- later, sensory disturbance in the distribution of nerves traversing the compartment
- later, weakness of muscles innervated by nerves traversing the compartment
4. Principles
General treatment principles
Effective management of an impending or established compartment syndrome requires:
- recognition of the risk of, or actual compartment syndrome (symptoms and signs)
- understanding the pathophysiology
- intracompartmental pressure measurement
- recognition of the importance of early surgical treatment
- resources to manage the aftercare and rehabilitation requirements
Pathophysiology
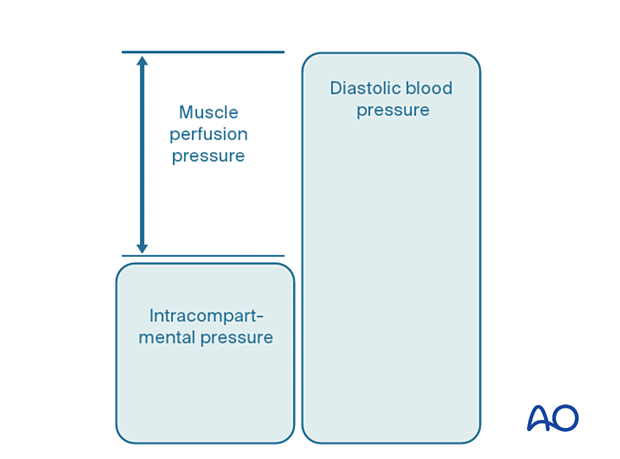
The most reliable measure of critical intracompartmental perfusion is the muscle perfusion pressure (MPP).
MPP is equal to the difference between diastolic blood pressure (dBP) and measured intramuscular pressure.
This difference in pressure reflects tissue perfusion more reliably than absolute intramuscular pressure.
When the muscle perfusion pressure is reduced to a level at which no capillary perfusion occurs, hypoxia leading to ischemia, and subsequent necrosis will occur.
The critical muscle perfusion pressure depends on the specific anatomical compartment affected.
Intracompartmental pressure measurement
When the clinical symptoms and signs of compartment syndrome are present, there is no benefit in measuring intracompartmental pressures, and an immediate fasciotomy should be performed.
When it is difficult to confirm the diagnosis, intracompartmental pressure measurement is helpful:
- to confirm the diagnosis
- to monitor a compartment at risk of increasing pressures
- to avoid unnecessary fasciotomy
- to measure intracompartmental pressures after decompression if symptoms persist
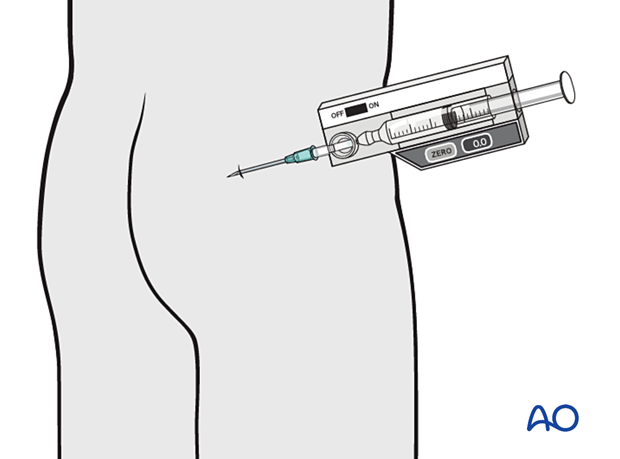
Compartment pressures should be measured at the area of maximal swelling or trauma. There are several techniques for the measurement of intracompartmental tissue pressure:
- commercially available intracompartmental pressure device
- large-bore needle and manometer
- electronic strain gauge
If the necessary equipment is not available for direct intracompartmental pressure measurement, then the diagnosis must be assumed if there is reasonable clinical suspicion, and fasciotomies must be performed.
Timing
Reversible ischemiaIn established muscle compartment syndrome, nerve and muscle tissue will become ischemic within less than two hours.
It is therefore of paramount importance that the intracompartmental pressure be released as an emergency intervention.
It is generally accepted that after 6–8 hours of inadequate muscle perfusion pressure (MPP), extensive muscle necrosis is inevitable. Release of the muscle compartments involved will not prevent severe muscle contracture.
Fasciotomy of compartments within which muscle necrosis has already happened has a high risk of infection.
Amputation may be required.
5. Compartmental anatomy
Muscular anatomy
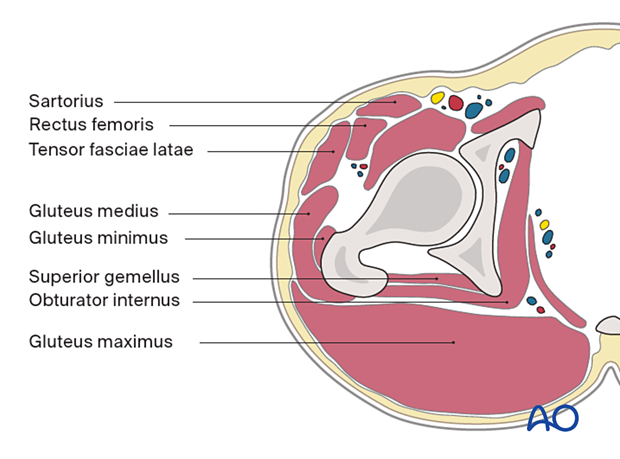
The muscles of the gluteal region comprise the following:
- Sartorius
- Rectus femoris
- Tensor fasciae latae
- Gluteus medius
- Gluteus minimus
- Superior gemellus
- Obturator internus
- Gluteus maximus
- Inferior gemellus
This cross section illustrates the muscular anatomy of the gluteal compartment at the level of the superior gemellus.
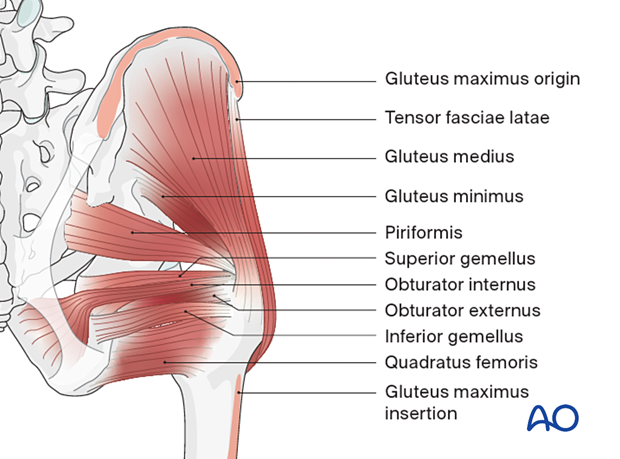
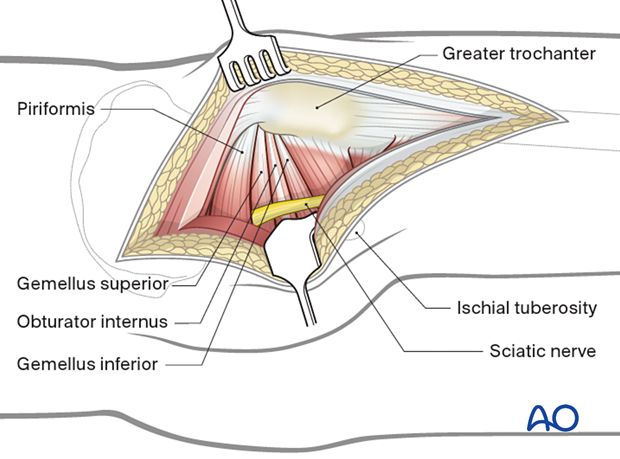
This posterior view shows that the gluteus maximus has been removed so as to better visualize the underlying muscles:
- Tensor fasciae latae
- Gluteus medius
- Gluteus minimus
- Piriformis
- Superior gemellus
- Obturator internus
- Obturator externus
- Inferior gemellus
- Quadratus femoris
Neurovascular anatomy
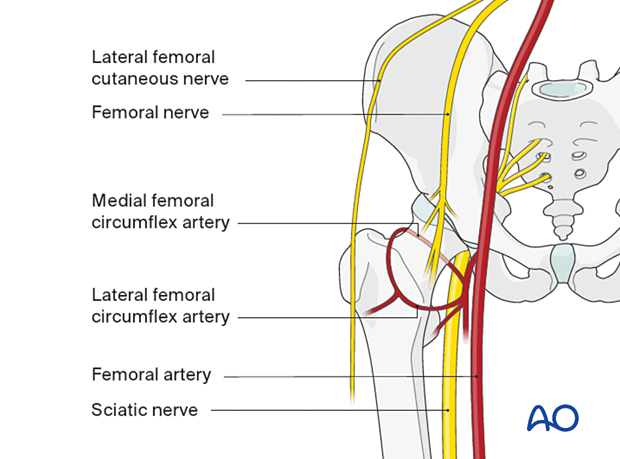
This illustration shows the neurovascular anatomy of the anterior aspect of the pelvis and upper thigh:
- Lateral femoral cutaneous nerve
- Femoral nerve
- Medial femoral circumflex artery
- Lateral femoral circumflex artery
- Femoral artery
- Sciatic nerve
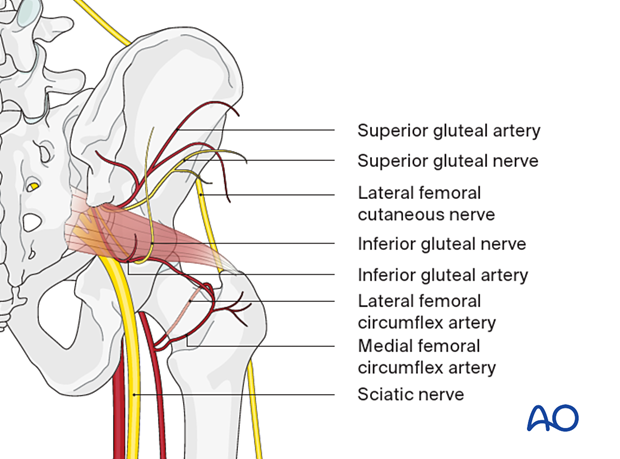
This illustration shows the neurovascular anatomy of the gluteal region:
- Superior gluteal artery
- Superior gluteal nerve
- Lateral femoral cutaneous nerve
- Inferior gluteal nerve
- Inferior gluteal artery
- Lateral femoral circumflex artery
- Medial femoral circumflex artery
- Sciatic nerve
6. Fasciotomies
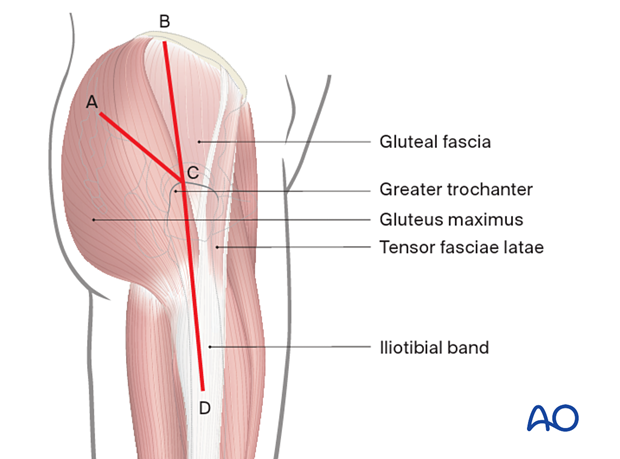
Two surgical approaches may be used to perform the necessary fasciotomies.
- The Kocher-Langenbeck follows the lines A-C-D
- The Gibson approach follows the lines B-C-D
We will illustrate the use of the Kocher-Langenbeck approach to the gluteal region.
7. Kocher-Langenbeck approach to the gluteal region
Introduction
The Kocher-Langenbeck approach is an approach to the lateral and posterior musculature of the hip.
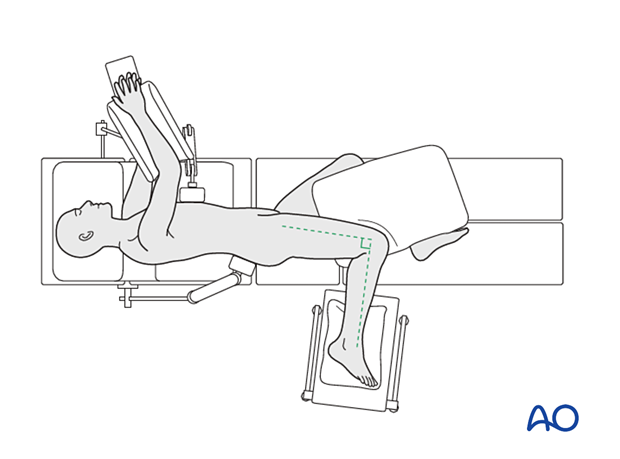
To manage compartment syndrome of the gluteal region, the Kocher-Langenbeck approach is performed in the lateral position.
Pelvic and acetabular surgical exposure – Kocher-Langenbeck approach – lateral
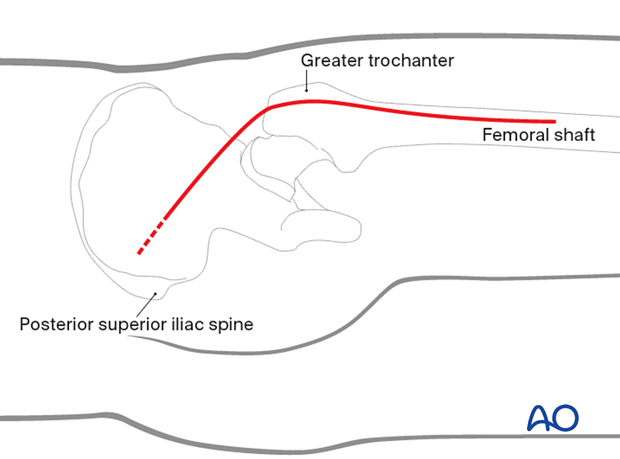
Skin incision
The bony landmarks used are:
- Posterior superior iliac spine
- Greater trochanter
- Femoral shaft
The skin incision is started distal and lateral to the posterior superior iliac spine. A more proximal extension (indicated by the dashed line) may improve exposure in obese or muscular patients.
The incision is continued to the greater trochanter and curved distally in line with the lateral aspect of the femoral shaft.
The incision ends at the mid third of the thigh.
Superficial surgical dissection
Fascial incisionAfter dividing the subcutaneous tissues, sharply incise:
- The gluteus maximus muscle
- The iliotibial band
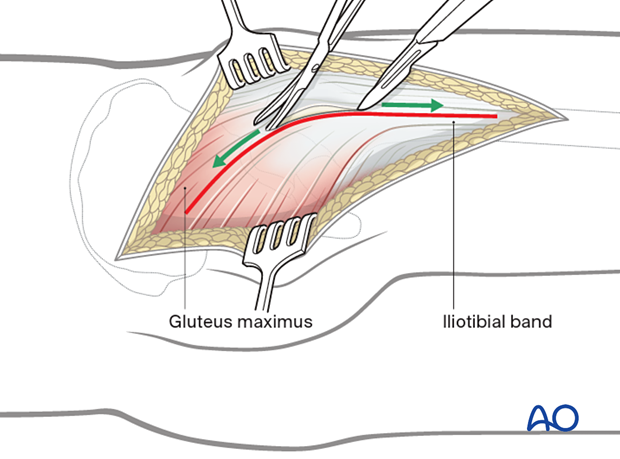
The gluteus maximus is split in line with its fibers, starting at the greater trochanter in a proximal direction up to the crossing of the first neurovascular bundle.
The iliotibial band is incised in line with its fibers up to the mid third of the thigh.
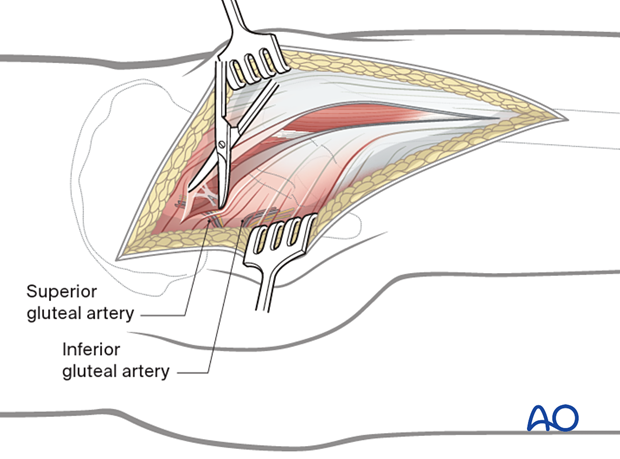
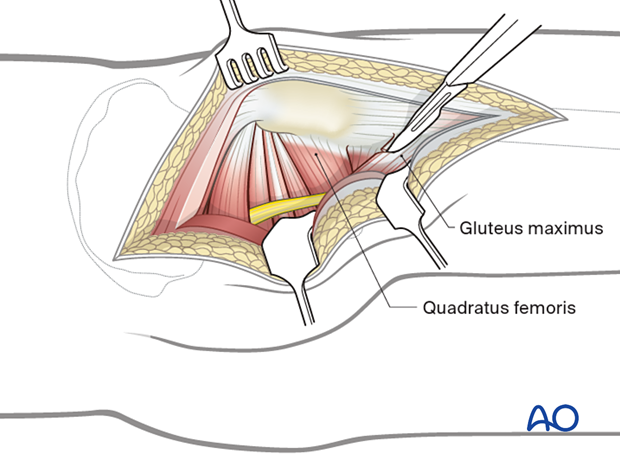
Deep dissection
The fascia of the gluteus medius and minimus can now be incised longitudinally in their mid-substance. It is safer to perform the fasciotomy through the anterior third of these muscles to minimize the risk of damaging the superior gluteal artery and nerve.
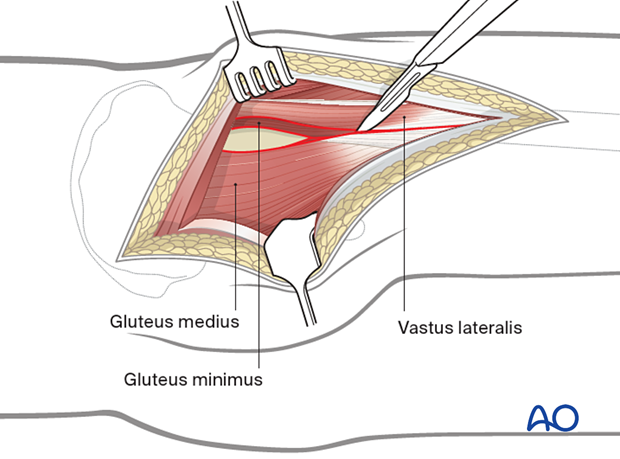
The insertions of the piriformis, the gemelli, and the obturator internus muscle are exposed.
The sciatic nerve (see illustration) lies posterior to the gemelli and obturator internus muscles, and passes either anterior, posterior, or through the piriformis muscle, between the greater trochanter and the ischial tuberosity. Be aware that anatomic variants do exist. In the majority of individuals (around 85%), the sciatic nerve and its peroneal branch pass under the piriformis muscle before exiting the greater sciatic notch. There can be variations, with the peroneal division or the entire sciatic nerve sometimes passing through or above the piriformis muscle.
The gluteus maximus can be detached 1 cm from its insertion into the gluteal tuberosity of the femur.
Detachment can be done partially or completely.
This results in less tension in, and easier mobilization of the gluteus maximus muscle.
Individual muscles in this deep group can be independently released or decompressed if needed.
- The sciatic nerve must be visualized at all times to avoid traction or direct injury to the nerve.
- Care must be taken to avoid traction or direct injury of the superior gluteal artery or nerve in the posterior part of this dissection.
Temporary soft-tissue management
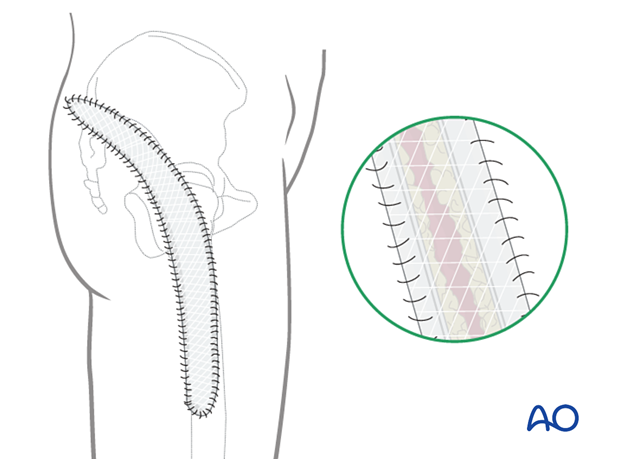
After a fasciotomy or fasciotomies have been performed, skin edges retract and can become difficult to close. Careful use of elastic retention sutures (elastic vessel loops woven through skin staples) can help counteract excessive skin contraction while still allowing the decompressed muscles to swell without any undue tension over them. Temporary coverage of the wounds can be obtained with either a wound vacuum-assisted closure (VAC) device or coverage with saline-soaked gauze bandages. These dressings or the wound VAC can be kept on until the patient returns for an attempt at secondary closure.
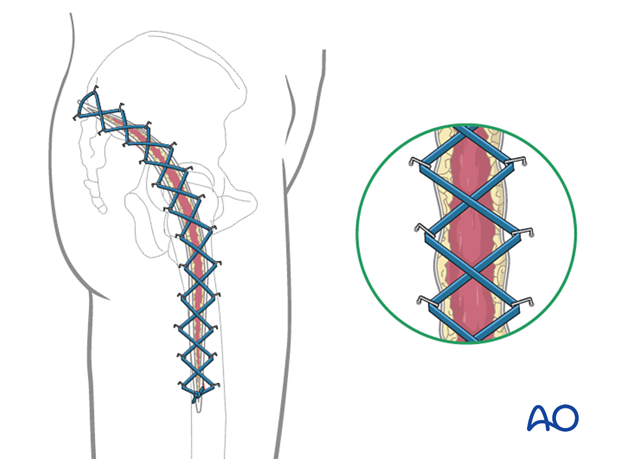
Delayed soft-tissue management: primary closure
If the swelling of the limb adequately decreases upon subsequent return to the operating room, primary closure of the fasciotomy wounds can occur. It is important not to perform primary closure if there is any concern about persistent swelling; secondary coverage options exist. In many instances, application of an incisional wound vac can enhance wound healing.
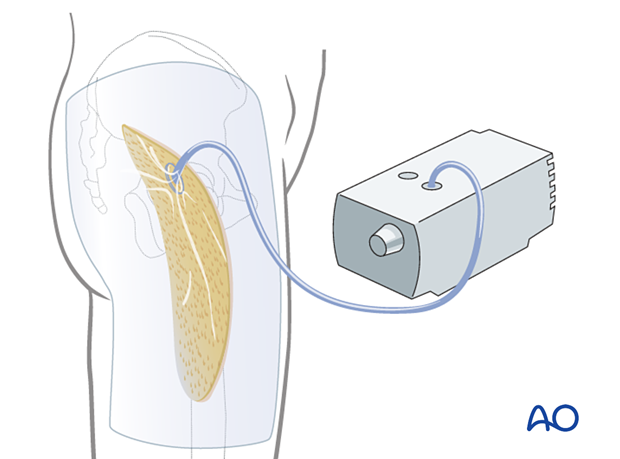
Delayed soft-tissue management: secondary coverage
If persistent swelling exists but wound closure is necessary, particularly for fractures that have been fixed, secondary wound coverage options are necessary. These include split thickness skin grafting, muscle flaps, or musculocutaneous flaps In many instances wound vacs are employed to enhance wound healing.
It is imperative to cover fractures that have been fixed in a timely manner so as to minimize the risk of subsequent infection.
8. Aftercare
Rehabilitation
Once wound healing has occurred, it is recommended to initiate range of motion exercises to minimize the development of contracture. Strengthening can begin at the discretion of the treating surgeon depending on the soft-tissue and bone injuries sustained.
9. References
General compartment syndrome references
Gourgiotis S, Villias C, Germanos S, et al Acute limb compartment syndrome: a review. J Surg Educ. 2007 64(3):178-86.
Mabee JR Compartment syndrome: a complication of acute extremity trauma. J Emerg Med.1994 12(5):651-6.
McQueen MM, Duckworth AD. The diagnosis of acute compartment syndrome: a review. Eur J Trauma Emerg Surg. 2014 Oct;40(5):521-8.
McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br. 2000 Mar;82(2):200-3.
Powell-Bowns MF, Littlechild JE, Yapp LZ, et al. Tibial shaft fractures - to monitor or not? a multi-centre 2 year comparative study assessing the diagnosis of compartment syndrome in patients with tibial diaphyseal fractures. Injury. 2021 Oct;52(10):3111-3116.
von Keudell AG, Weaver MJ, Appleton PT, et al. Diagnosis and treatment of acute extremity compartment syndrome. Lancet. 2015 Sep 26;386(10000):1299-1310.
Gluteal compartment syndrome
Diaz Dilernia F, Zaidenberg EE, Gamsie S, et al. Gluteal Compartment Syndrome Secondary to Pelvic Trauma. Case Rep Orthop. 2016;2016:2780295.
Gupta AK, Burgos MI, Lopez-Viego M, et al. Gluteal Compartment Syndrome After Prolonged Immobilization in Drug Abusers. Cureus. 2020 Aug 18;12(8):e9847.
Hinton JB, Heck VC, Ebraheim NA, et al. Compartment Syndrome of the Gluteal Region: A Rare Condition Requiring a High Index of Suspicion. J Orthop Case Rep. 2024 Jan;14(1):178-181.













