Compartment syndrome
1. Introduction
Principles
Compartment syndrome is a true surgical emergency. Failure to diagnose it and to institute urgent treatment by decompression usually results in major limb disability.
In compartment syndrome increasing tissue pressure prevents capillary blood flow and produces ischemia in muscle and nerve tissue. The process is progressive and leads to necrosis with permanent loss of function.
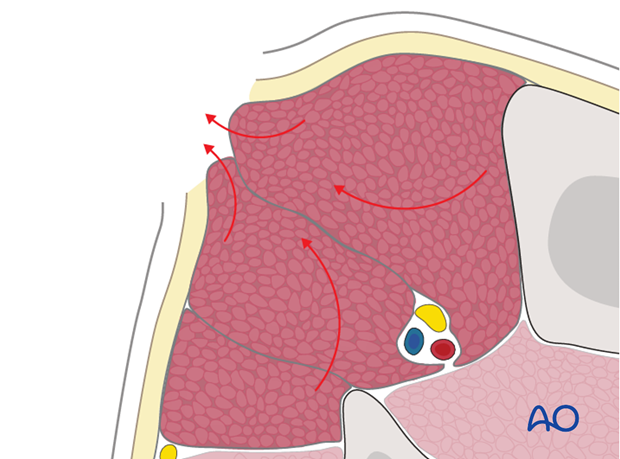
Treatment of compartment syndrome requires surgical release of the closed osteo-fascial compartment by wide and lengthy division of the skin and fascial envelope.
Incidence
Muscle compartment syndrome is a relatively common occurrence in the osteo-fascial compartments of the lower leg. It also may occur in other anatomical compartments. Other common sites are the forearm, thigh, foot and hand. Forearm compartment syndrome may also be associated with supracondylar humeral fractures in children. Muscular young adult males are at particular risk.
A meta-analysis of tibia shaft fractures has revealed that the overall risk of compartment syndrome following these injuries varied across studies from 2.7% –15.6%.
Causes
Muscle compartment syndrome occurs most commonly after high-energy limb injuries. However, it can occur after apparently trivial injuries, with or without fractures, or elective extremity surgery. Crushing injuries are at high risk of compartment syndrome. Certain other insults, such as burns, or prolonged compression (as may occur in a comatose, unprotected patient), may also cause muscle swelling and precipitate the syndrome.
A further cause can be edema from abnormal capillary permeability caused by reperfusion after prolonged ischemia. Tight bandages, splints, or casts can also elevate compartmental pressure and contribute to development of compartment syndrome.
Pathophysiology
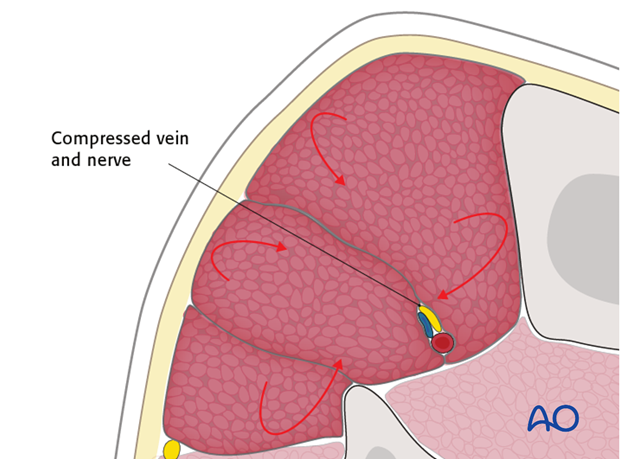
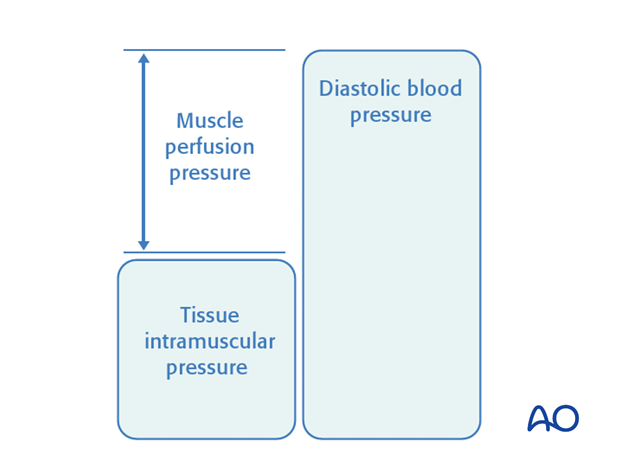
Compartment syndrome occurs when the pressure within a closed osteofascial muscle compartment rises above a critical level. This critical level is that tissue pressure which collapses the capillary bed and prevents low-pressure blood flow through the capillaries and into the venous drainage. Normal tissue pressure is 0-10 mm Hg. The capillary filling pressure is essentially diastolic arterial pressure. When tissue pressure approaches the diastolic pressure, capillary blood flow ceases. A number of studies have shown that:
- if diastolic arterial pressure is less than 30 mm Hg above tissue pressure, compartmental capillary blood flow is significantly obstructed and severe hypoxia occurs in muscle and nerve tissue.
The critical measurement is muscle perfusion pressure (MPP), the difference between diastolic blood pressure (dBP) and measured intramuscular tissue pressure. (MPP has also been called ΔP, to indicate the difference between diastolic blood pressure and intramuscular pressure.) This difference in pressure reflects tissue perfusion far more reliably than the absolute intramuscular pressure.
Muscle tolerates short periods of hypoxia, but after a few hours, progressive necrosis begins.
An arterial injury may cause compartmental tissue ischemia. After blood flow is restored, capillaries leak and ischemic muscle swells. Reperfusion injury is another cause of compartment syndrome.
2. Diagnosis
Symptoms
The diagnosis of this severe complication rests on two factors: a high index of suspicion and a thorough understanding of its variable clinical presentation.
In a conscious and alert patient, there will be unrelenting, worsening pain, greater than expected for the particular injury, and not related to limb position.
Commonly there is a relatively pain-free interval, perhaps a few hours following fracture treatment, before such pain develops.
The level of pain can often be judged by increasing requests for ever-stronger analgesia, or increasing use of patient-controlled analgesia (PCA) systems. Any nerve traversing the involved compartment will become hypoxic, often causing numbness and tingling in the nerve distribution. After some hours, ischemic nerves cease to function and the pain resolves.
Signs
Clinical signs of an impending muscle compartment syndrome include tenderness and induration of the affected compartment, increase in the pain on passive muscle stretching, possible sensory (and later motor) deficit in the territory of a nerve traversing the compartment and muscle weakness.
The presence of a distal pulse does not exclude compartment syndrome, because in a normotensive patient the muscle pressure rarely exceeds the systolic level.
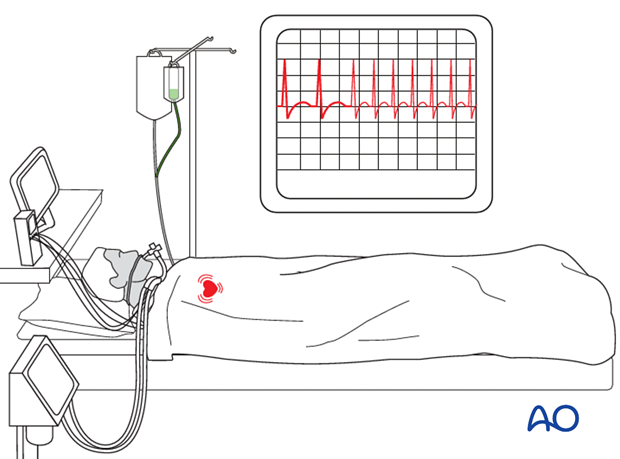
In an unconscious, drugged, or intoxicated patient, it is easy to miss a compartment syndrome. Any visible limb swelling becomes a vital clue as does persistent, unexplained tachycardia. For such patients, direct tissue pressure measurement is very helpful for diagnosis.
Investigation
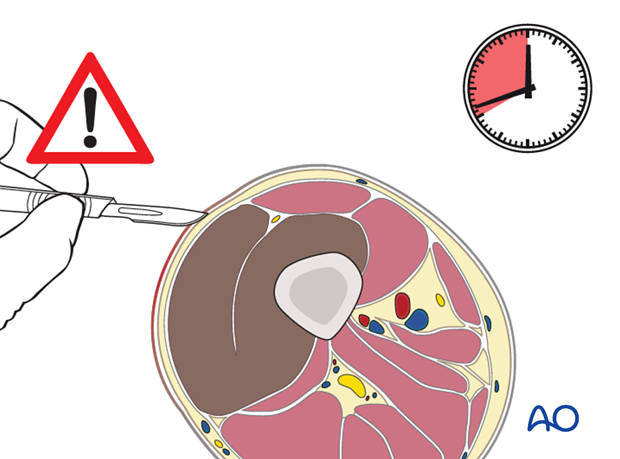
Intra-compartmental pressure measurement
When compartment syndrome is obvious, there is usually no benefit from measuring pressures and immediate fasciotomy can be undertaken.
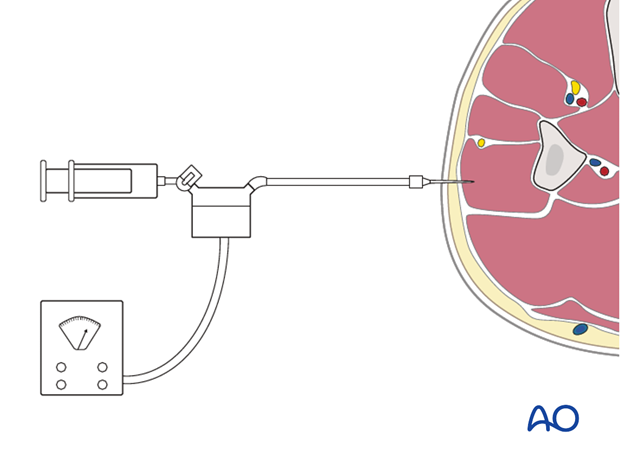
When the diagnosis is unclear, or possibly absent, compartment pressure measurement may be confirmatory, or prevent unnecessary fasciotomy. Various techniques are now available to measure the intra-compartmental tissue pressure.
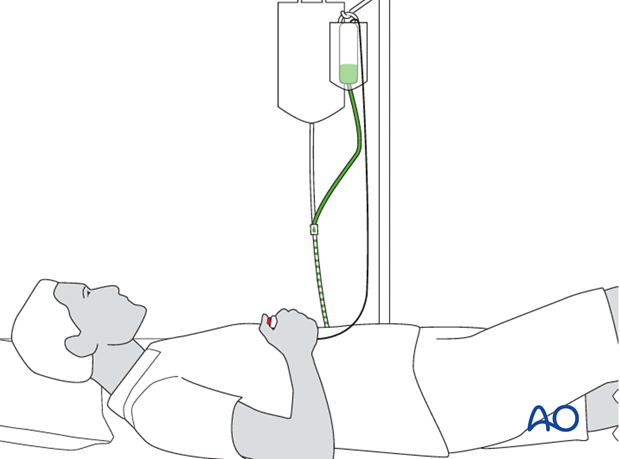
All trauma surgeons should adopt a technique that is available for them and their teams. This might involve use of a commercially available compartmental pressure device, a mercury manometer, large-bore needle and connecting tubing (after Whitesides), or an electronic strain gauge used for physiologic monitoring in ICU, or the OR.
If the necessary equipment is not available for direct pressure measurement within the muscle compartment, then the diagnosis must be assumed if there is a reasonable clinical suspicion.
3. Treatment
Timing
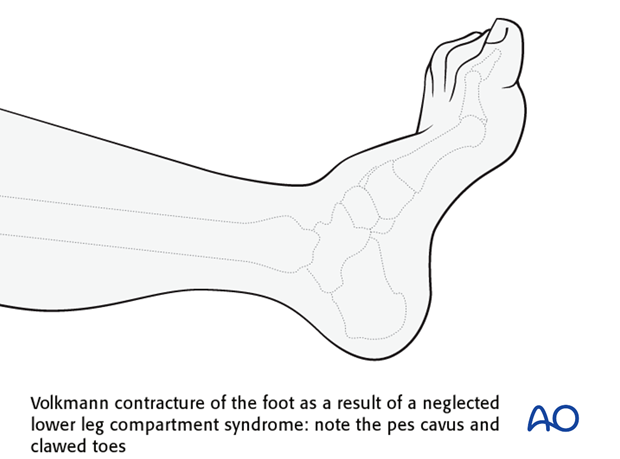
In established muscle compartment syndrome, the hypoxic muscle will become necrotic within hours. It is generally accepted that after 6-8 hours of inadequate muscle perfusion pressure (MPP), extensive muscle necrosis is likely and effective release of the muscle compartments involved is unlikely to avoid severe muscle contracture. Similarly any peripheral nerve passing through the compartment is likely to suffer permanent functional impairment.
It is therefore of paramount importance that the compartment hypertension be released as an emergency intervention.

If diagnosed within 8 hours
The only appropriate treatment is dermato-fasciotomy of all involved compartments.
Late diagnosis
There is some limited evidence in the published literature to suggest that in delayed cases, where there is already extensive muscle death, dermato-fasciotomy has a high risk of infection of the dead tissue, septicemia and, in some cases, death. There appears to be a high amputation rate in such cases (Finkelstein JA, Hunter GA, Hu RW. (1996) Lower limb compartment syndrome: course after delayed fasciotomy. J Trauma. Mar;40(3):342-4.)
Where recognition of an established compartment syndrome is delayed for more than 8-10 hours after probable onset, the decision to perform a dermato-fasciotomy requires judgment by the most experienced surgeon available. This situation is common after mass disasters (e.g. earthquake). Exposure of partially necrotic muscle produces a wound with high risk of infection.
Fracture fixation
If fracture stability is important for adequate care of the injured limb, particularly if a compartment syndrome has damaged the local muscles, this can be provided temporarily by external fixation, with minimal additional surgical trauma. Alternatively, internal fixation with an intramedullary nail, or a plate, can be undertaken to achieve immediate definitive stabilization, if appropriate. After stabilization, the fasciotomy wounds are left open, as discussed next.
Aftercare
Delayed surgical closure
Once any skeletal injury is under control, the fasciotomy wound(s) healthy and the swelling of the soft tissues has sufficiently regressed, consideration must be given to achieving skin coverage.
The simplest and safest technique is to cover the healthy soft-tissue defect with a split skin graft. At a later date, when the limb contours have returned to normal, the grafted area can be excised and secondary skin closure performed without tension.
It is tempting to the surgeon to try early secondary skin suture, rather than skin-graft coverage, once the swelling has subsided. This is only permissible if it can be achieved without any skin tension; it is inadvisable in smokers, who have impaired capacity for soft-tissue healing.
Fasciotomy wounds tend to contract and become difficult to close. Careful use of elastic retention sutures (elastic vessel loop woven through skin staples) can help to counteract skin contraction, and be tightened progressively as swelling resolves. This can help to reduce the size of the defect to be covered.
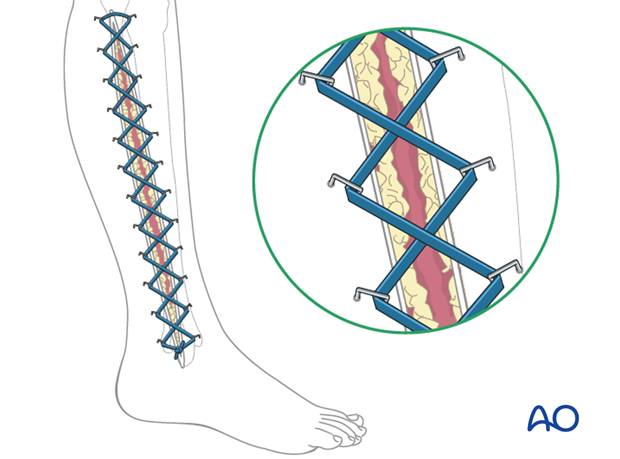
Postoperative splintage
It is important to splint the limb in a neutral, or functional, position, particularly if any muscle damage has occurred and contractures could therefore develop.













