Antegrade nailing approach to the femoral shaft with piriformis entry point
1. General considerations
Most femoral nailing procedures are performed with antegrade nailing position. It is extremely successful and utilizes minimally invasive techniques.
The piriformis entry point is used for straight nails.
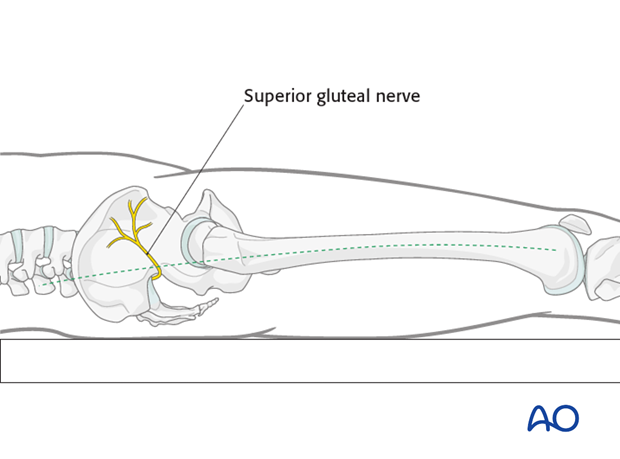
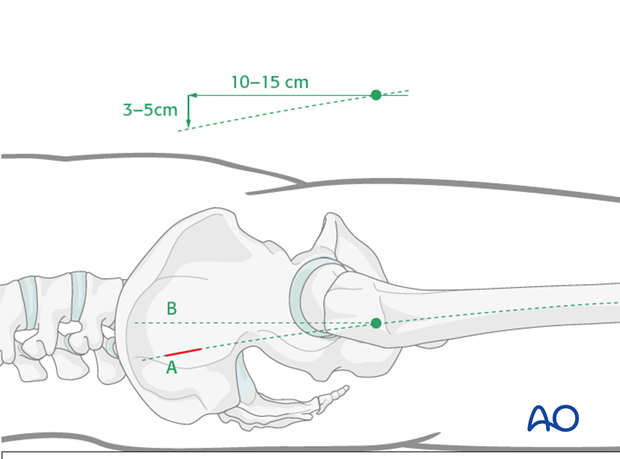
Generally, draping should always be applied up to the pelvic rim, to find the correct individual location for the skin incision.
Care should be taken to make the skin incision in line with the curved axis (dashed line) of the femoral canal to minimize the risk of injury to the superior gluteal nerve.
Another reason to make the skin incision in line with the bow of the femur is to minimize the risk of eccentric reaming of the proximal fragment, leading to the risk of perforation of the posterior femoral shaft cortex.
The correct position for the piriformis fossa entry point is just medial to the tip of the greater trochanter. In certain cases, the greater trochanter may be curved and medialized. It may then be necessary to ream through the medial tip of the greater trochanter.
If the first guide wire is not in line with the femoral canal, eccentric nail placement may result. This may ultimately cause an iatrogenic femoral neck fracture when the nail is inserted, because the oblique insertion increases stress upon the femoral neck.
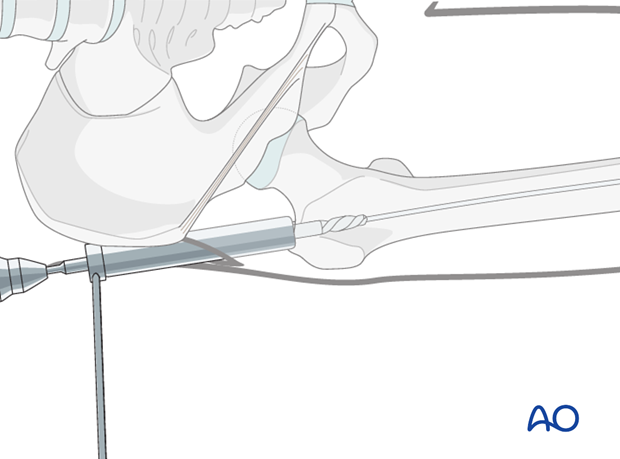
2. Skin incision
To locate the site of the skin incision, the tip of the greater trochanter and the axis of the femur are marked with the help of the image intensifier and by palpating the trochanter.
A 3-5 cm incision is made 10-15 cm proximal to the tip of the greater trochanter on the proximal extension of the anatomical femoral bow (A).
(B) marks a horizontal line drawn from the top of the greater trochanter, which represents an incorrect skin incision.
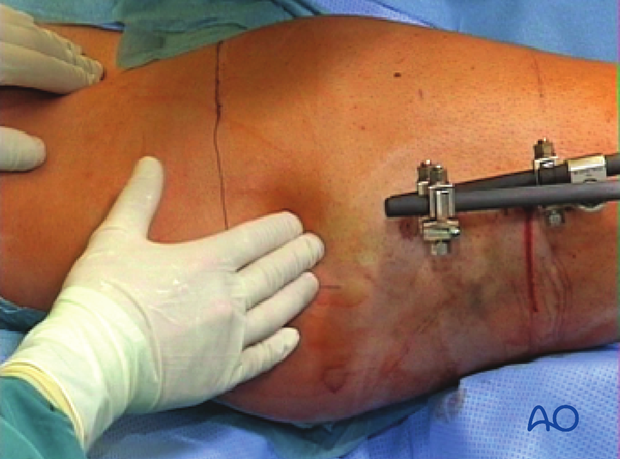
The external fixator is maintaining the reduction for femoral nailing.
If in doubt whether to make the incision ten or fifteen cm proximal to the tip of the greater trochanter (eg, in an obese patient), the correct entry point may be assessed with a K-wire and the AP view of the hip.
In cases of morbid obesity, it may be necessary to make the incision even further proximally (up to 20 cm (lower skin line)).

3. Deep dissection
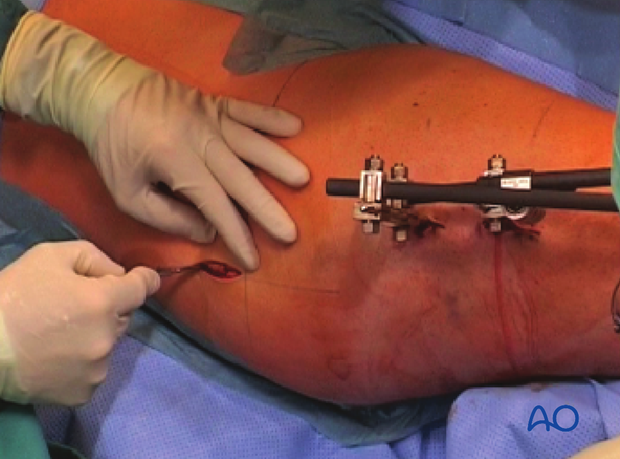
The fascia is opened with scissors and the gluteus muscle is split along its fibers.
(Image shows external fixator used as temporary fixation device.)
Dissection is carried down to bone.
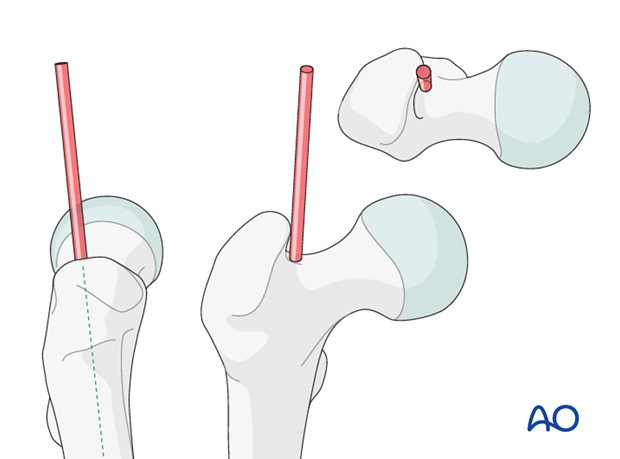
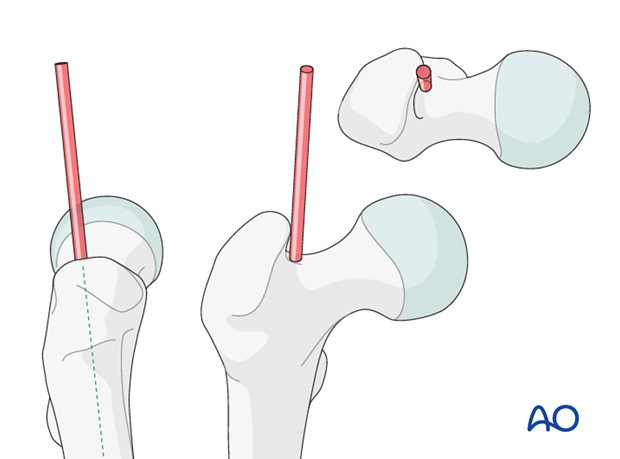
4. Determination of entry point and guide-wire insertion
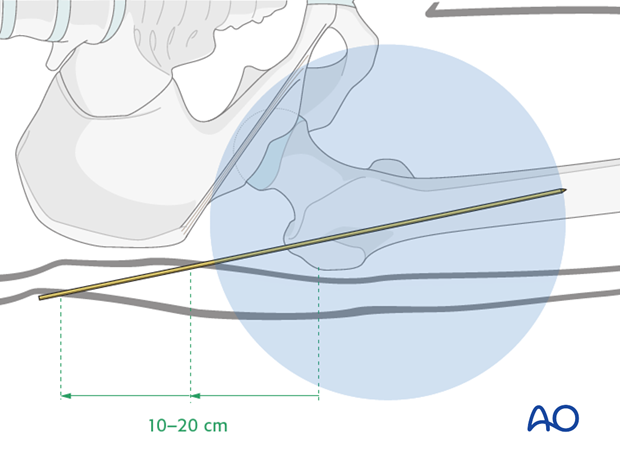
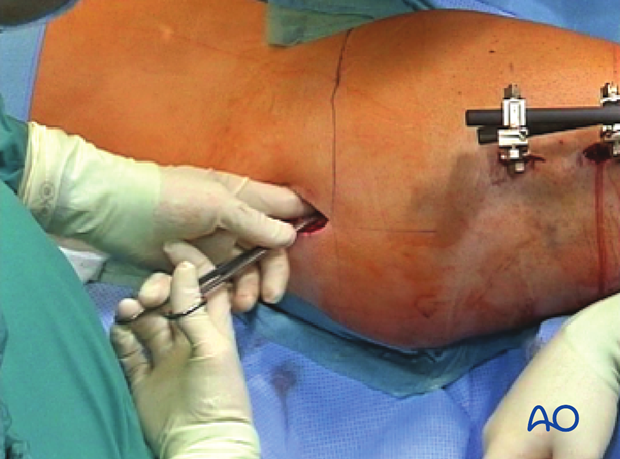
A finger is inserted to palpate the greater trochanter. The 2.8 mm guide wire, inserted under image intensifier control, enters the medullary canal at a slightly oblique angle. Introduction is manual, using the universal chuck with T-handle.
Verify the entry point by both AP and lateral views with image intensifier.
(Image shows external fixator used as temporary fixation device.)
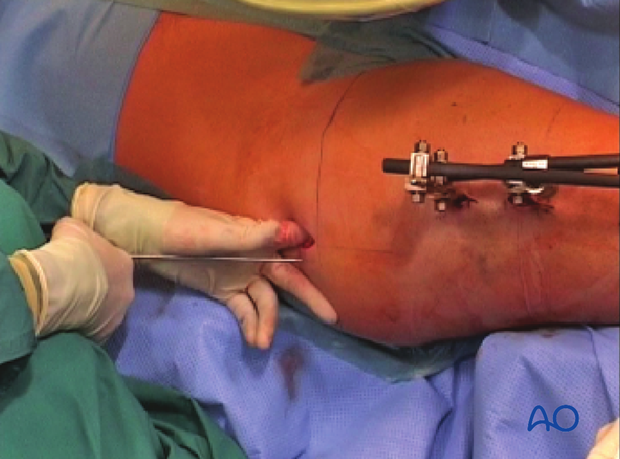
If there is difficulty pushing the guide wire through the cortex of the piriformis fossa, the awl can be used to start the track.
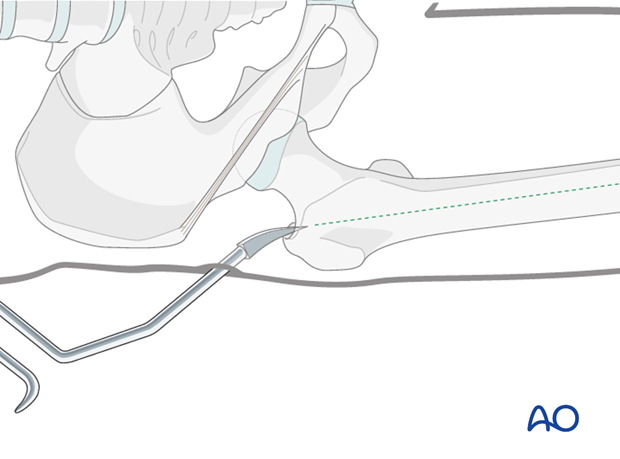
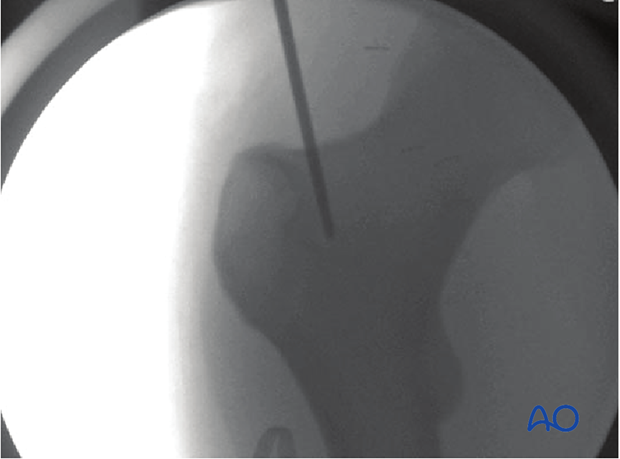
Fluoroscopy image of awl in piriformis with unidentified femoral neck fracture.

The soft-tissue track for determination of the entry point should deviate less than 15° from the axis of the femoral shaft to avoid any stress on the femoral neck upon insertion of the nail.
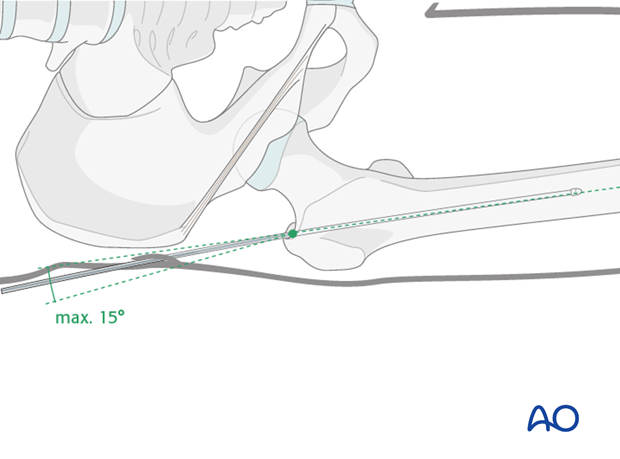
X-ray showing the correct position of the guide wire.
5. Opening the canal
The cannulated drill bit is passed over the guide wire and through the protection sleeve to open the medullary canal.
(Enlarged image shows external fixator used as temporary fixation device.)
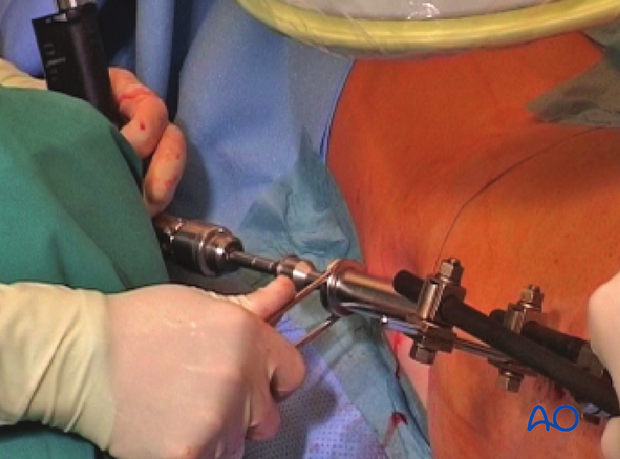
Image shows opening the canal using a drill bit.