Nonoperative treatment - Definitive cast
1. General considerations
Definitive nonoperative treatment with a cast is only exceptionally indicated for distal tibia fractures. The nonoperative treatment may, however, be adequate in non- or minimally displaced fractures that are stable. Exceptionally, high surgical risk may be an indication for nonoperative treatment despite incomplete reduction.
Cast immobilization may occasionally be used for initial management until soft tissues recover for ORIF. In highly unstable fractures, a cast may not provide adequate reduction and stability. These fractures should be stabilized with an external fixator.
Teaching video
AO teaching video: Application of a Lower Leg Circular Cast
2. Reduction
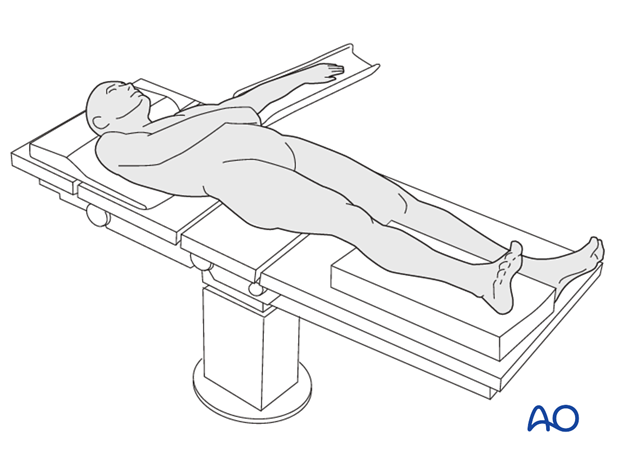
Positioning
In undisplaced fractures reduction is not necessary. Displaced fractures should be reduced as soon as possible with anesthesia as necessary. The lower leg should be positioned on a pillow so that the heel is slightly elevated from the table.
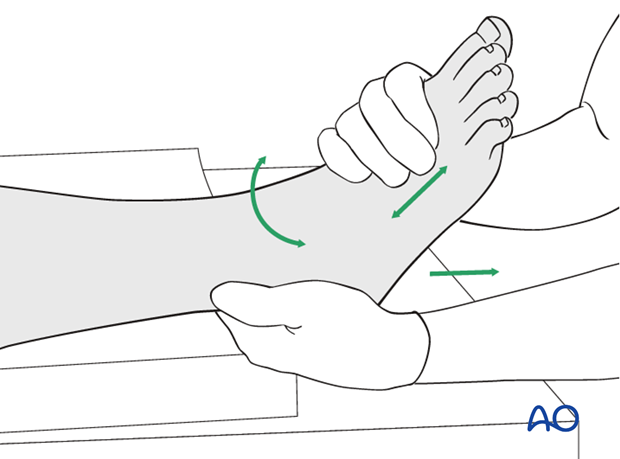
Manual reduction
The foot is held around its middle from plantar and medial with one hand by the surgeon. The heel is grasped with the other hand. Reduction is achieved by gentle traction and by alignment of the foot to match the axis of the lower leg, also correcting rotation.
For temporary casting, the deformity may in some cases be overcorrected to protect the soft tissues.
Note: After reduction, presence of palpable pedal pulses should be reconfirmed.
3. Cast application
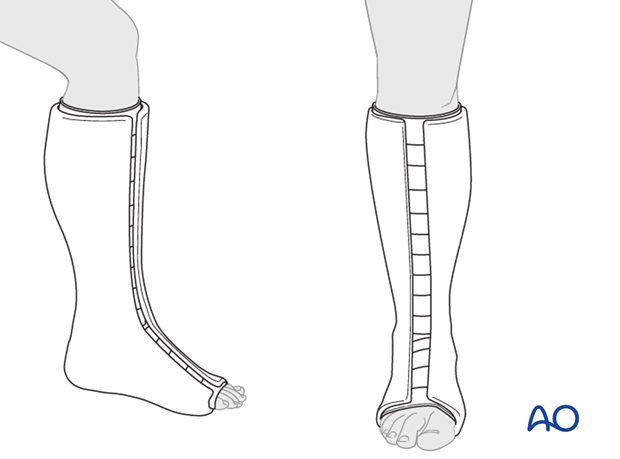
Principles
Reduction must be maintained during cast application by gentle manual and/or gravity traction.
Abundant cast padding is applied. This should not be too tight but may include very gentle compression.
Progressive local soft-tissue swelling is expected during the first days after injury. Therefore, a closed circular cast is usually contraindicated. The cast may be split and spread anteriorly, or “bivalved” with medial and lateral cuts. The splitting should provide room for swelling, the padding should not be too tight, and all bony prominences should be decompressed.
Plaster of Paris or fiberglass cast tape can be used. With plaster, the cast must be allowed to harden before splitting is possible.
A compartment syndrome can occur even after a cast is split. The split cast has to be sufficiently stable to support the fracture.
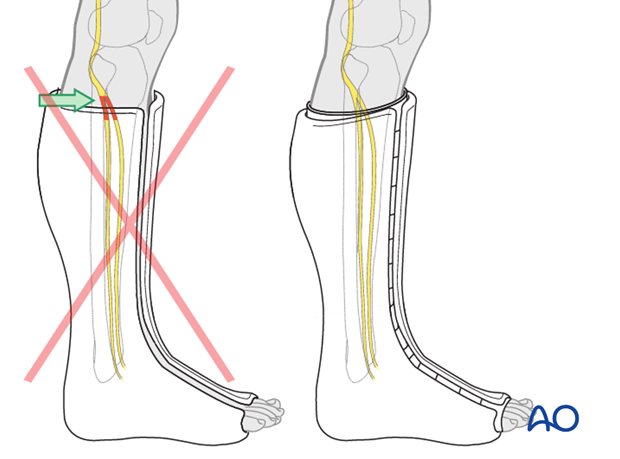
Landmarks for cast application and the importance of adequate padding
Proximally, the posterior edge of the cast lies distal to the popliteal fossa, laterally it remains distal to the neck of the fibula and the at risk common peroneal nerve. Anteriorly, it can approach the tibial tubercle. An easy landmark is 3-4 fingerbreadths below the popliteal crease. All toes should be visible dorsally. The common peroneal nerve, superficial to the proximal fibula, may be compressed by the top of a below-knee cast. Adequate padding and cast molding (posterior flattening and apex anterior angle) help to minimize this risk.
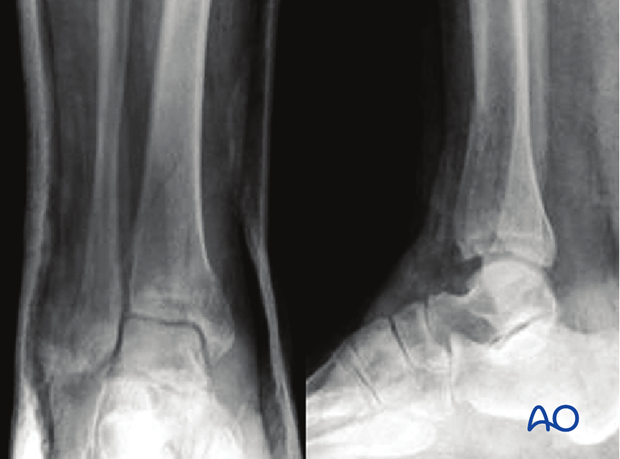
Note: After application of the cast, the fracture alignment should be documented radiologically.
4. Aftercare following nonoperative treatment with a cast
Follow-up x-rays at three or seven, and fourteen days will detect early loss of reduction in cases where definitive nonoperative treatment is planned. In case of secondary displacement, remanipulation is possible but the fracture situation usually requires additional stability by internal or external fixation.
With definitive nonoperative treatment, the split cast is changed for a circular cast after 1 - 2 weeks dependent upon the local soft-tissue situation. The circular cast is worn for another 4 - 5 weeks.
Weight bearing is typically not allowed during the period of cast immobilization.
After 6 weeks, progressive weight bearing is initiated over a period of 4 – 6 weeks. Thrombosis prophylaxis is often indicated until full weight bearing is achieved.













