Anteromedial or anterolateral approach to the distal tibia?
1. Principles
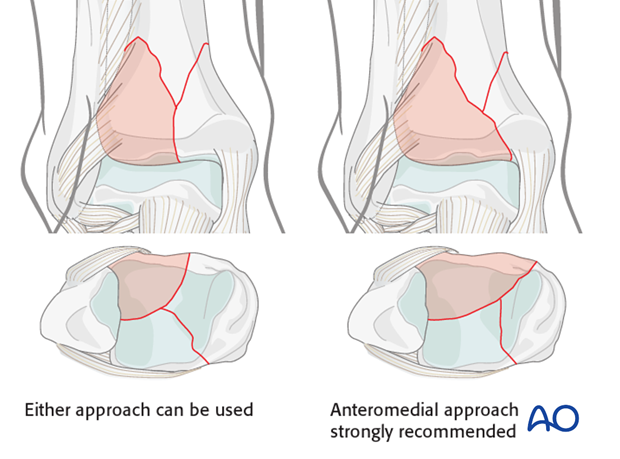
Most tibial pilon fractures are best approached anteriorly, either anteromedially or anterolaterally. The size of the anterolateral fragment helps determine the optimal approach. When it is large, and its medial fracture plane is at or near the medial malleolus, an anteromedial approach is recommended. When the anterolateral fragment is smaller, and the fracture crosses the articular margin more laterally, its reduction can be achieved with an anterolateral approach.
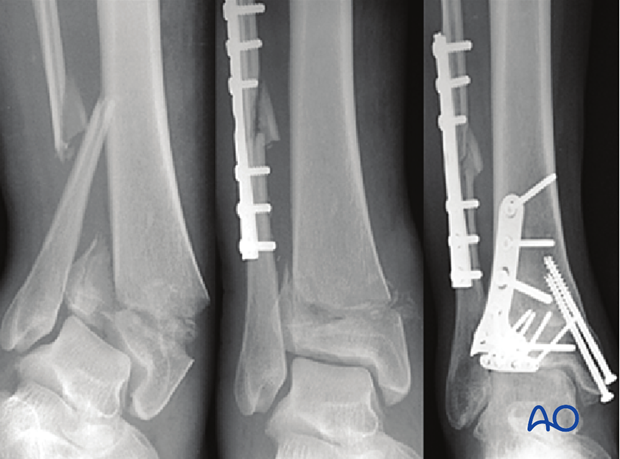
For open fractures with the commonly observed associated transverse medial traumatic wound at the distal tibia (see illustration), an anterolateral surgical approach may be preferable to minimize additional dissection beneath the medial traumatized skin. Similarly, a distal tibial fracture with an associated lateral traumatic open wound may be best approached anteromedially. The anticipated incision(s) for ORIF should be considered during initial debridement and external fixation, even though definitive fixation is delayed until soft tissues recover.

2. Injury radiographic evaluation and its influence on approach and implants
The choice of implants in a 3-part articular fracture is dependent on the associated metaphyseal comminution, the surgical approach, and the soft tissue envelope as previously described. The associated metaphyseal comminution should be considered and assessed on the injury radiographs. With bending fractures, comminution occurs on the side that fails in compression. Tension failure typically produces a simple transverse fracture plain.
For pilon fractures with a varus deformity, medial metaphyseal comminution is commonly observed and medial buttress plating with a stronger medial implant is necessary. An anteromedial approach is preferable for its application.
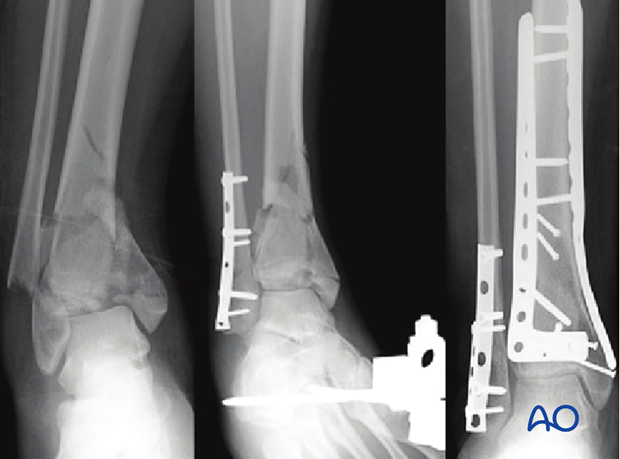
For pilon fractures with a valgus deformity, lateral metaphyseal comminution is commonly observed, and the medial distal tibia typically fails in tension. In these patterns, lateral or anterolateral buttressing is optimal and medial fixation can be less strong.
Thus, for a pilon with significant initial valgus and lateral and/or anterolateral metaphyseal comminution, an anterolateral approach permits optimal placement of a buttress plate.
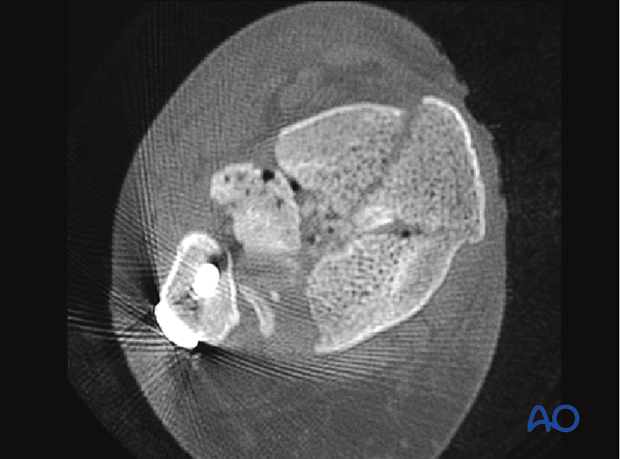
3. Articular comminution and impaction
There are multiple commonly observed articular injuries that increase the complexity of complete articular fractures from the 3-part injury described above. These include the presence of articular comminution and impaction. Impaction is frequently seen centrally and medially.
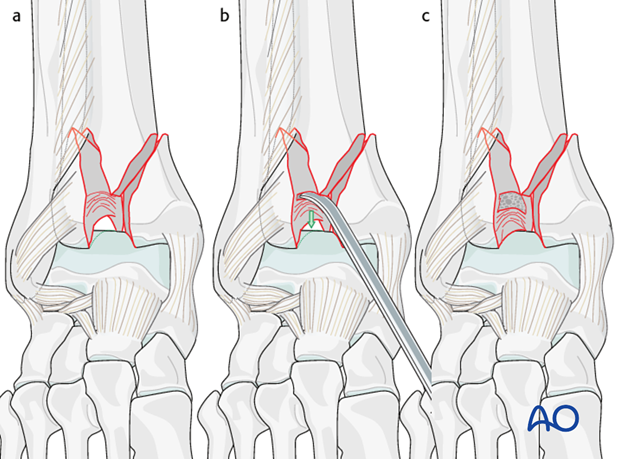
Articular surface impaction is important to identify and correct. Direct access to the impacted area must be provided through the chosen surgical approach.
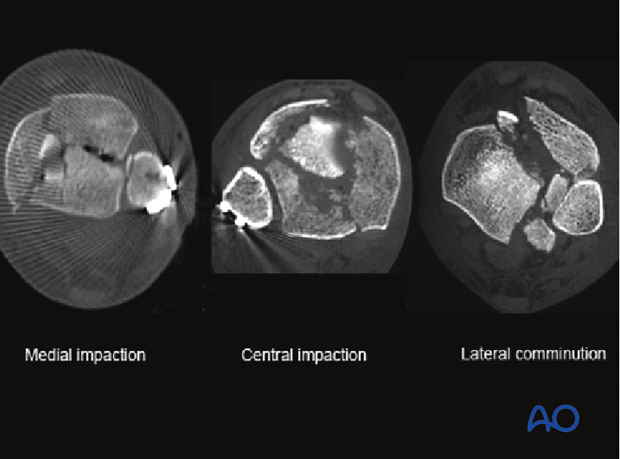
4. Medial comminution and impaction
Medial comminution and impaction is frequently seen in pilon fractures with a predominant varus deformity. The two typical locations are at the lateral aspect of the medial malleolus and at the medial aspect of the anterolateral fragment.
Medial articular comminution is optimally visualized through an anteromedial approach. In addition to reduction of the associated comminution of the medial malleolus, this approach allows for reduction of the impaction seen at the medial aspect of the anterolateral fragment.
5. Lateral comminution and impaction
Lateral comminution and impaction is frequently seen in pilon fractures with a predominant valgus deformity. Lateral articular comminution can be approached through either an anteromedial or anterolateral approach. Visualization may be optimal with an anterolateral approach that allows for external rotation of the anterolateral fragment and direct reduction of the associated comminution.