Medial approach to the distal humerus
1. Indications
The main indications for a medial approach to the distal humerus are:
- Isolated medial epicondyle avulsion fractures
- Isolated medial trochlear fractures (very rare)
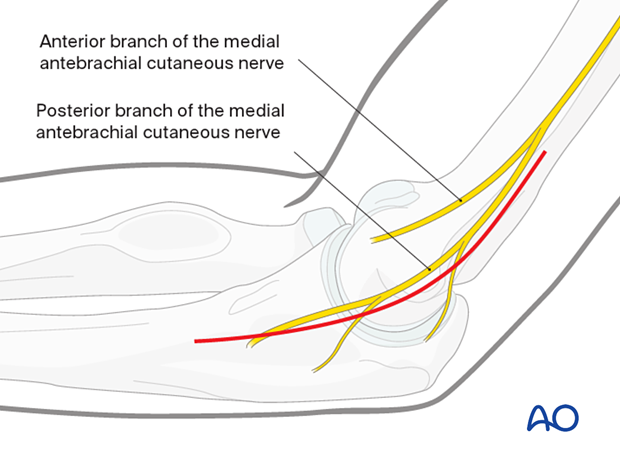
2. Skin incision
Center the incision over the medial epicondyle and extend it proximally over the medial supracondylar ridge and distally in the line of the flexor/pronator mass as required.
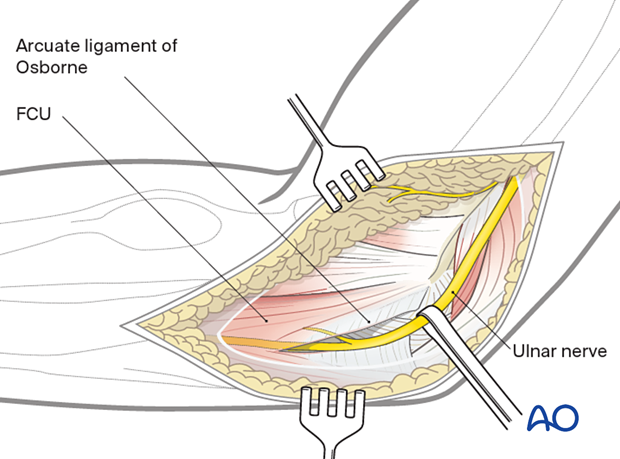
3. Identification of the ulnar nerve
Identify the ulnar nerve proximally between the triceps muscle and the medial intermuscular septum, in the groove posterior to the medial epicondyle, and distally between two heads of the flexor carpi ulnaris.
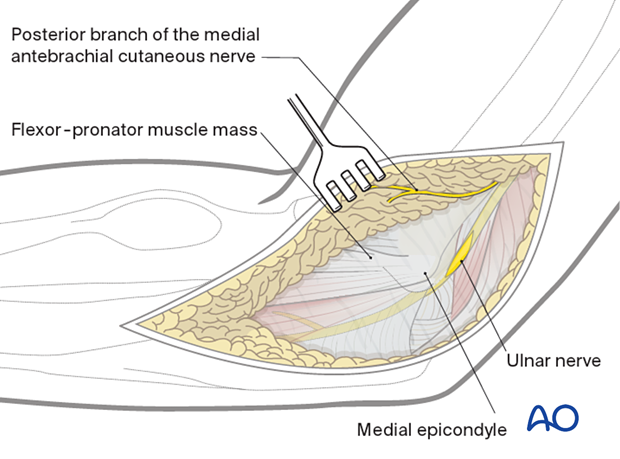
Gently free the ulnar nerve and protect it. If anterior transposition of the nerve becomes necessary, take care to preserve the motor branch to the flexor carpi ulnaris.
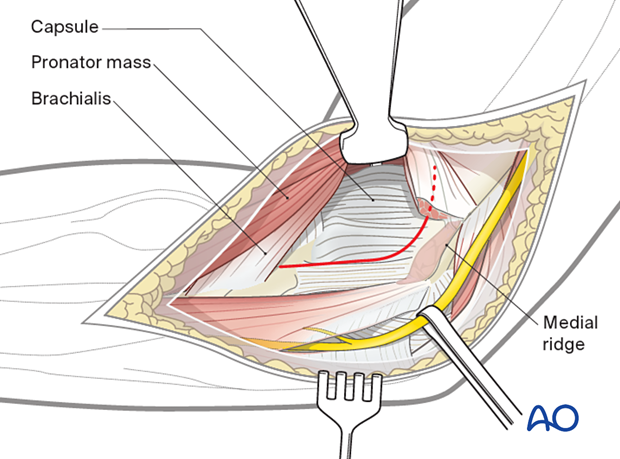
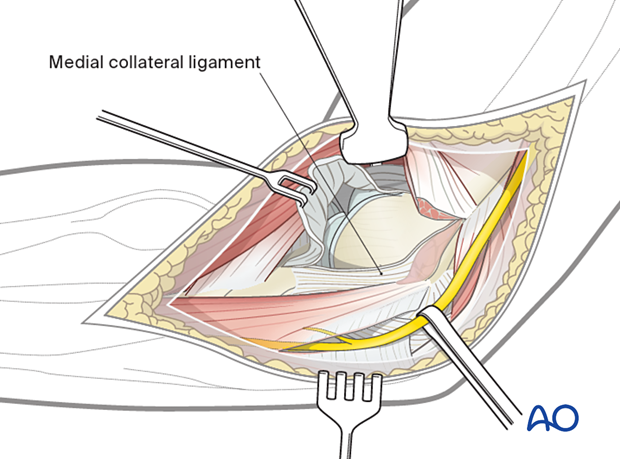
4. Deep dissection
The medial epicondyle fracture should now be identified, mobilized, and prepared for fixation.
If access to the trochlea is required, a split in the flexor/pronator muscle mass anterior to the origin of the medial collateral ligament should be made.
The planned capsulotomy is marked in red.
5. Opening the joint
Proximally elevate the muscles and joint capsule from the medial supracondylar ridge to access the trochlea.
Distally open the joint capsule and reflected anteriorly to the medial collateral ligament.
6. Wound closure
Close the wound in layers.













