Nonoperative treatment - Cast
1. General principles
Cast treatment is recommended and reliable for:
- undisplaced or minimally displaced intraarticular fractures
- unstable fractures in some low demand patients (when some degree of malunion may be tolerated)
How to make it work:
- exclude unstable fracture patterns
- recognize deformity and correlate to mechanism of injury
- use adequate analgesia
- obtain a good reduction before applying the cast
- meticulous casting technique
- do not immobilize in extreme positions
- careful early follow-up (x-rays and clinical)
Casting in low demand patients
It may not be possible to maintain reduction of a fracture in a cast, but a cast may be useful as a splint to help relieve pain.
Teaching videos
AO teaching video: Basic forearm circular cast
AO teaching video: Fractures and sprains - palmar slab splint
2. Reduction
Manual reduction
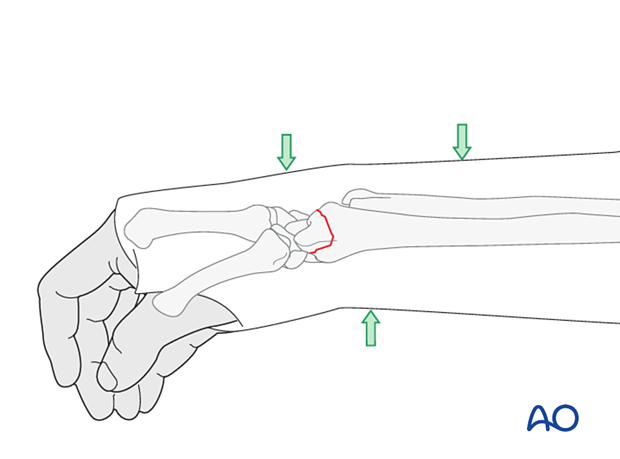
With traction applied, the distal fragment is pushed distally, and the wrist flexed to reduce the articular congruity.
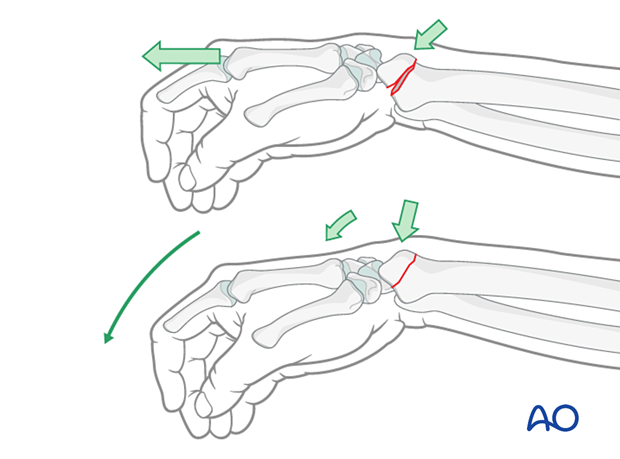
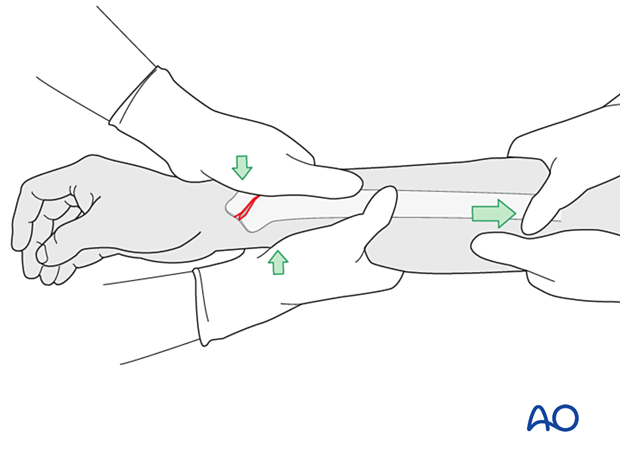
Correct remaining deformities
The heel of one hand is used as a fulcrum. Firm pressure, directed anteriorly corrects remaining posterior displacement and restores articular congruity. This is visible in lateral x-rays.
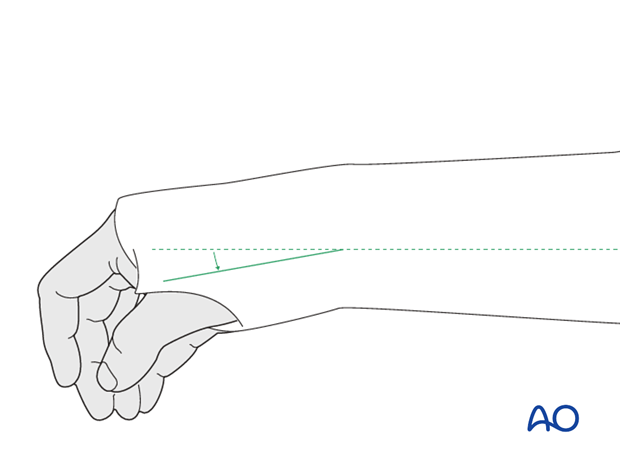
The wrist should be maintained in the cast at 15° of flexion, so that the dorsal capsule of the wrist joint keeps the dorsal fragments reduced.
3. Below elbow cast
Imaging
It is advisable to confirm that the fracture is in an acceptable position before applying the cast. This may require image intensifier.
Purpose
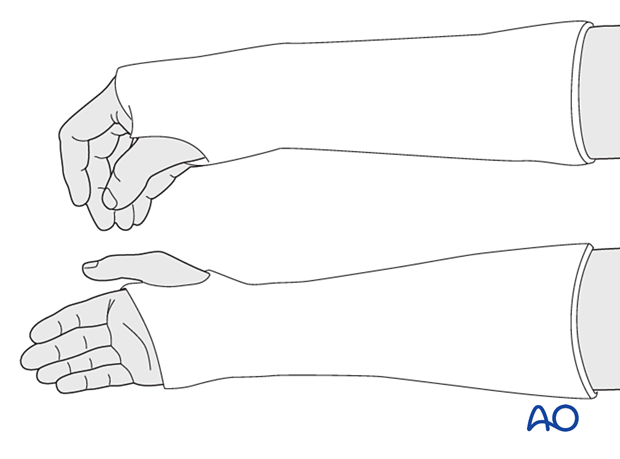
The cast used in the nonoperative treatment of most of distal radial fractures is a below elbow cast. If the ulna is involved, a sugar tong or an above elbow cast may be considered to control forearm rotation.
The purpose of a cast is to maintain the fracture reduction or prevent displacement, but ideally while minimizing the functional effect on the limb.
This is normally achieved by applying three-point fixation in the directions specific for that fracture pattern.
Care must be taken not to immobilize joints in a position which interferes with long term function, wherever possible.
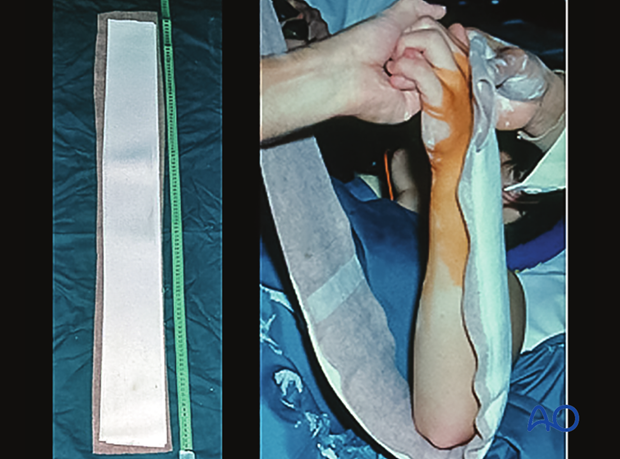
Applying a cast
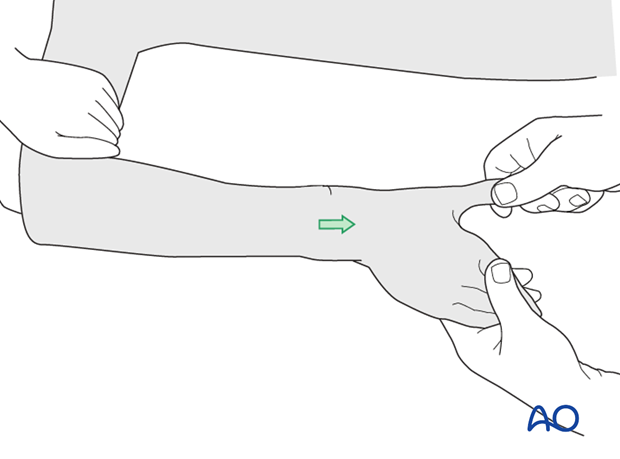
The assistant holds the thumb fully extended with one hand. The other hand holds the radial two/three fingers (avoiding cupping of the hand) maintaining slight traction, with ulnar deviation at the wrist.
If Chinese finger traps have been used instead of an assistant, the cast may be applied before the finger traps are released.
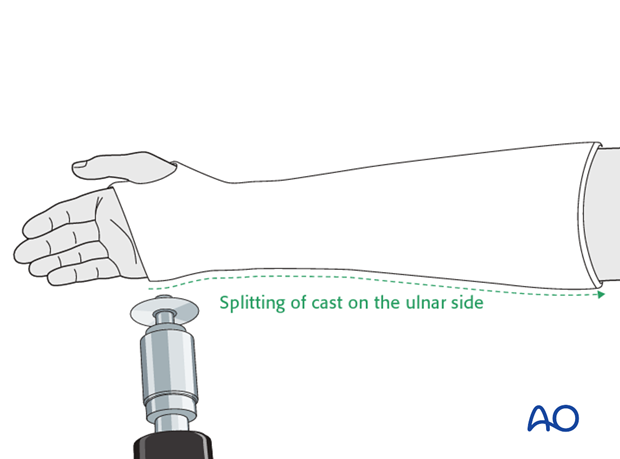
The initial cast should either be a backslab or a split cast to allow for swelling.
Distal perfusion should be checked at all stages of this procedure and continually monitored after cast completion.
In most fractures, the cast is maintained for 4-6 weeks. Once the initial swelling has subsided, the cast is changed with careful maintenance of position. It may be prudent to obtain a check radiograph in the new cast to make sure that no displacement occurred as the cast was changed.
In fractures which had significant displacement, even if well reduced in the initial cast, there is a significant risk of subsequent displacement and they should be monitored carefully with radiographs at one and two weeks.
Although a fracture may be remanipulated within two weeks of the injury, if a fracture displaces in a cast, the deformity should either be accepted, or the fracture might be better managed with ORIF.
Pearl
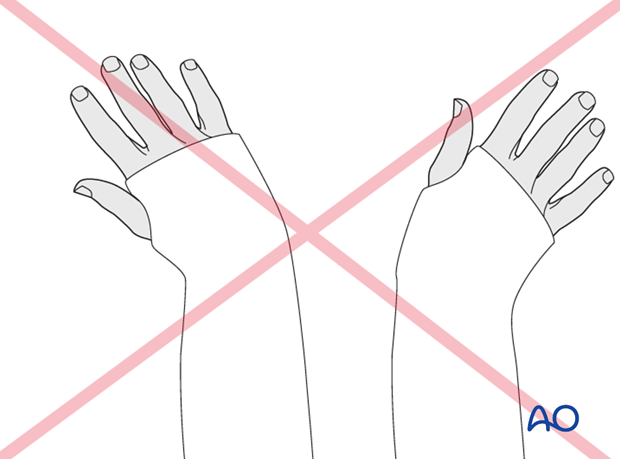
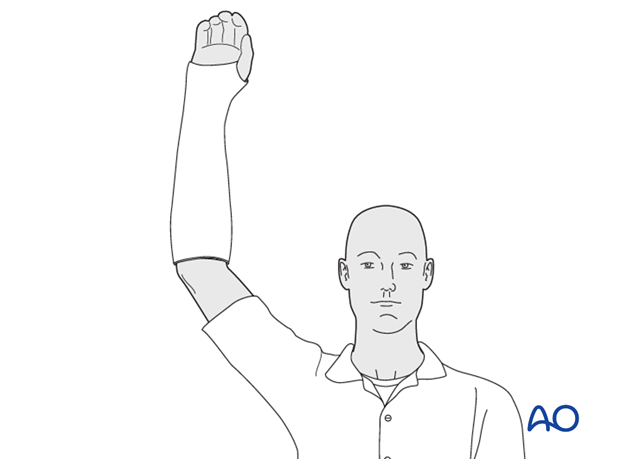
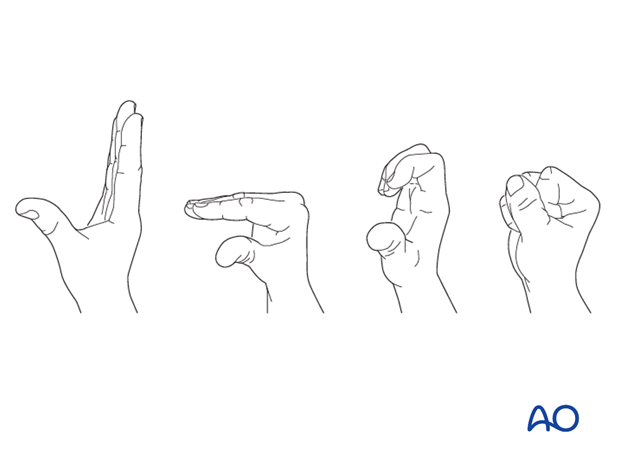
The joints at each end of the cast must be left free to move during the period of casting. Avoid extending the cast too close to the elbow anteriorly (which prevents elbow flexion). Pay particular attention to leaving the metacarpophalangeal joints (MCPJs) free. Failure to do this will result in capsular contracture and loss of MCPJ flexion.
The patient should be encouraged to extend the fingers and make a fist many times daily.

Pitfall: positional errors
Avoid extremes of any position. Difficulties will be encountered if the wrist is immobilized in extreme radial/ulnar deviation and/or flexion.
Monitoring
All patients in a cast should be monitored for pain, swelling, altered sensation or perfusion.
4. Other casting options
A simple forearm cast cannot control pronation and supination. If it is felt important to limit supination and pronation movement in the forearm, for example in ulnar fractures, it is necessary to extend a forearm cast proximally, either by the use of a sugar tong cast or an above elbow cast.
Sugar tong cast
A sugar tong cast is indicated in injuries affecting the DRUJ, if there is concern about any possible displacement.
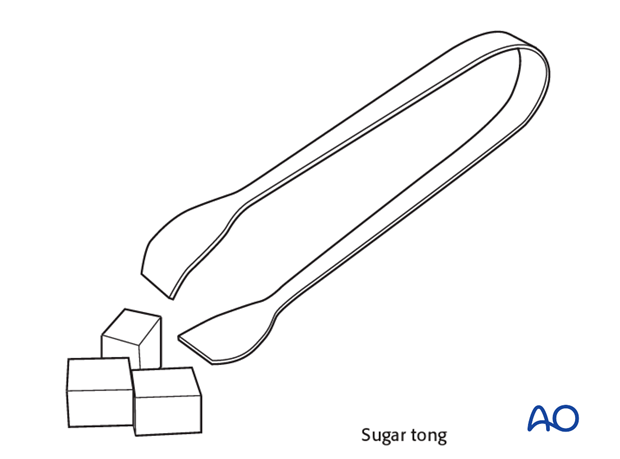
A sugar tong splint may be used for the first 2-3 weeks only. It prevents forearm rotation by immobilizing the distal radioulnar joint (DRUJ), yet allows some elbow flexion/extension, thereby preventing elbow stiffness.
It should be applied with elastic wrapping to allow for soft-tissue swelling.

5. Aftercare
Functional exercises
As soon as possible, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
X-rays are taken to check the reduction. Refer to your local protocol for timing of X-ray follow-up.
Cast removal
The cast (and K-wires if used) is left in place for 4-6 weeks. An x-ray will document fracture position at this time.













