ORIF - Radial column plate
1. Preliminary remarks
Fracture assessment
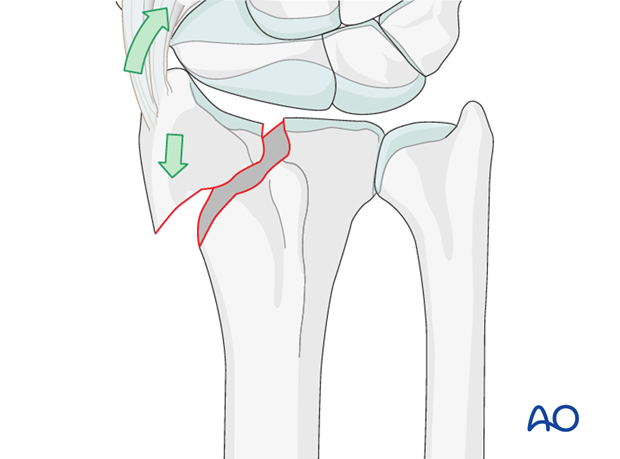
These are simple fractures of the radial styloid without comminution. They may be caused by shearing forces.
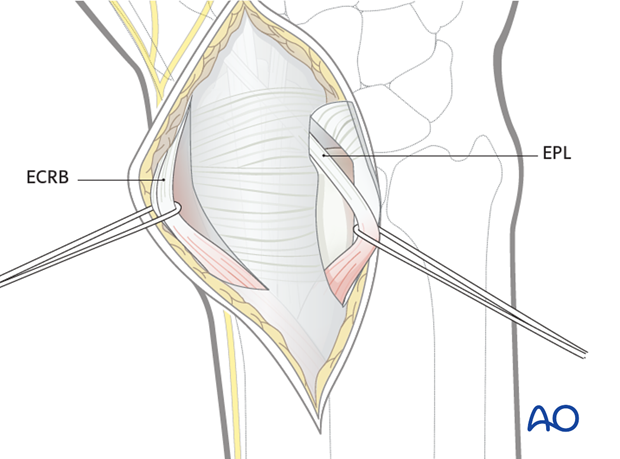
Access to the radial column may be gained through a dorsal approach using a retinacular incision between the first and second compartment (see dorsal approach for details).
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
Provisional reduction in displaced fractures
Reduction is achieved by applying longitudinal traction either manually or using Chinese finger traps.
The reduction is maintained by a temporary splint.
If definitive surgery is planned, but cannot be performed within a reasonable time scale, a temporary external fixator may be helpful.

2. Associated injuries
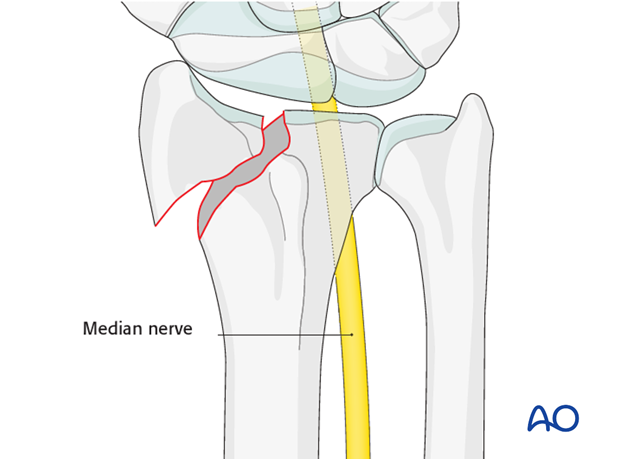
Median nerve compression
If there is dense sensory loss, or other signs of median nerve compression, the median nerve should be decompressed.
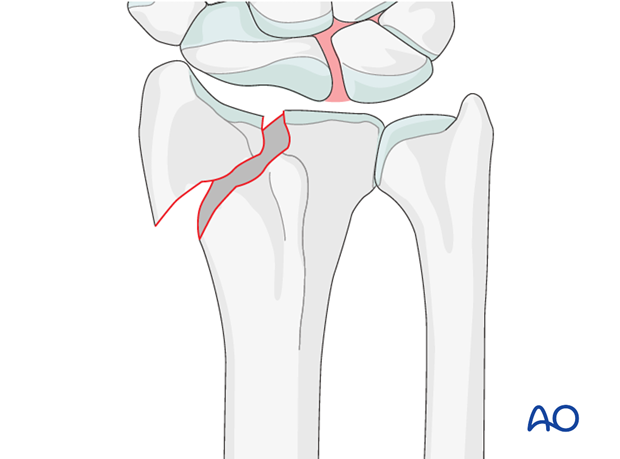
Associated carpal injuries
These injuries may be associated with shearing injuries of the articular cartilage, scaphoid fracture and rupture of the scapholunate ligament (SL). Every patient should be assessed for this injury. If present, see carpal bones of the Hand module.
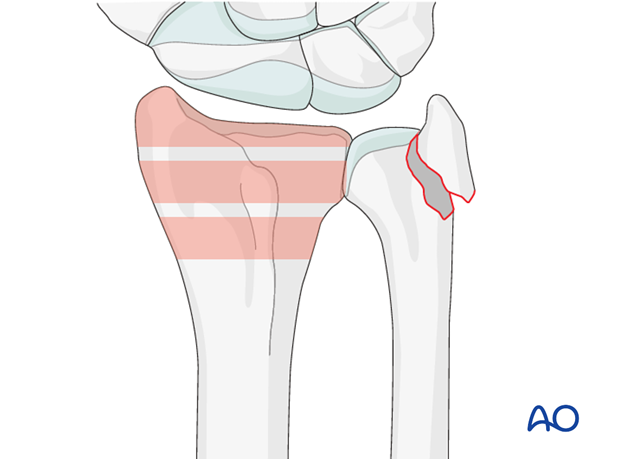
DRUJ/ulnar injuries
These injuries may be accompanied by avulsion of the ulnar styloid and/or disruption of the DRUJ. If there is gross instability after the fixation of the radial fracture, it is recommended that the styloid and/or the triangular fibrocartilaginous disc (TFC) is reattached. This is not common in simple fractures, but may occur with some high energy injuries.
The uninjured side should be tested as a reference for the injured side.
It may not be possible to assess DRUJ stability until the fracture has been stabilized (as described below).
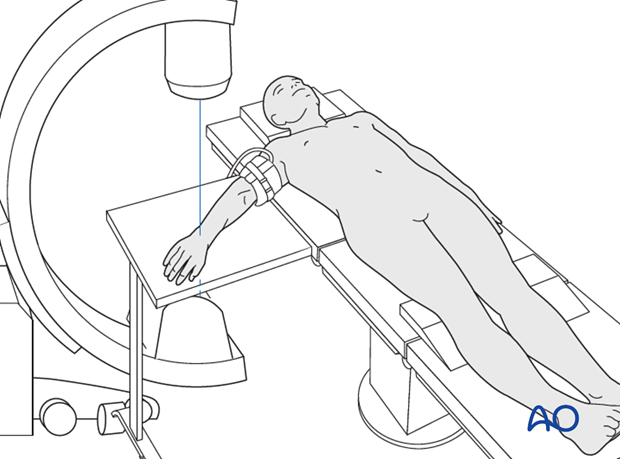
3. Patient preparation
The patient may be placed either in a supine position for palmar approaches or for dorsal approaches.
4. Provisional fixation of the radial styloid
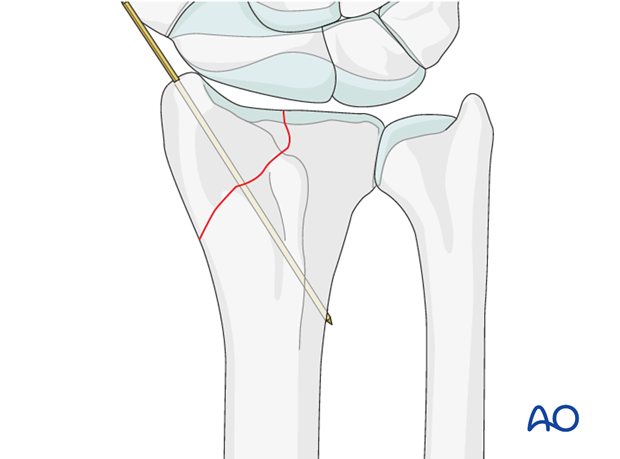
Provisional K-wire fixation
Insert a K-wire through the tip of the radial styloid to hold the fragment provisionally.
Confirm using image intensification.
5. Plate contouring
Dedicated radial column plates are available precontoured. However, some additional contouring may be necessary to accommodate the individual anatomy of some patients.
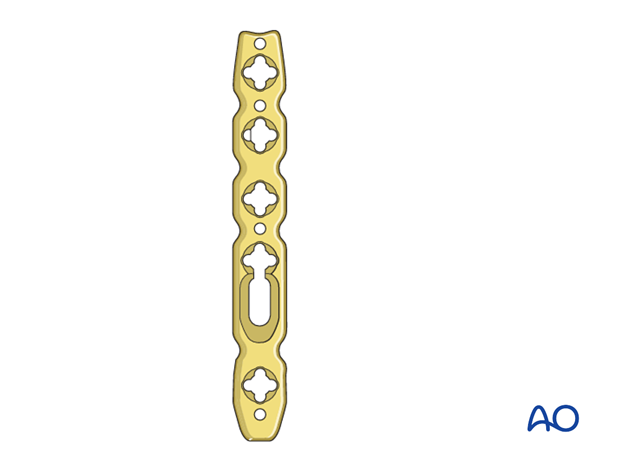
Pitfall: Screw hole distortion
Avoid contouring the plate through the locking holes, otherwise the locking head screw might not fit any more.

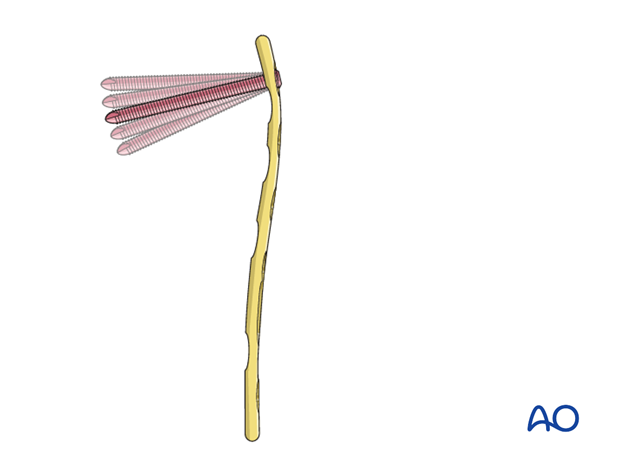
Variable angle locking plates enable precise positioning of the distal screws in desired directions, because there is 30° of freedom for each screw inside the plate hole to address the individual fracture patterns.
6. Plate application
Slide the plate underneath the first compartment and apply it onto the radial column.
Apply the plate onto the radial column.
Ideally, the notch in the distal tip of the implant should be placed against the temporary K-wire.

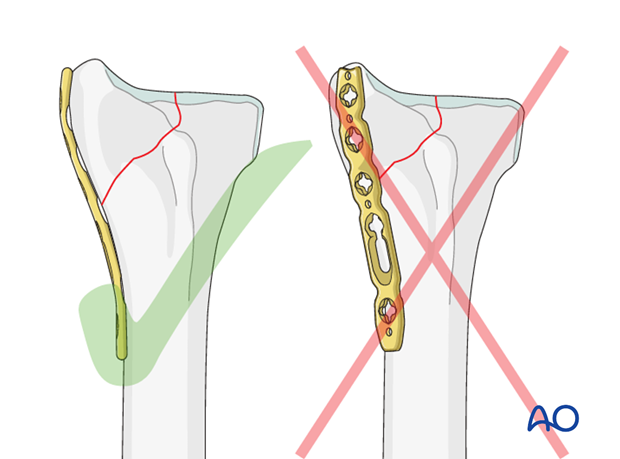
Pitfall: Inadequate buttressing
Placement of the plate on the dorsal aspect of the radial column is to be avoided as it will not buttress the reduction against shear forces.
7. Plate fixation
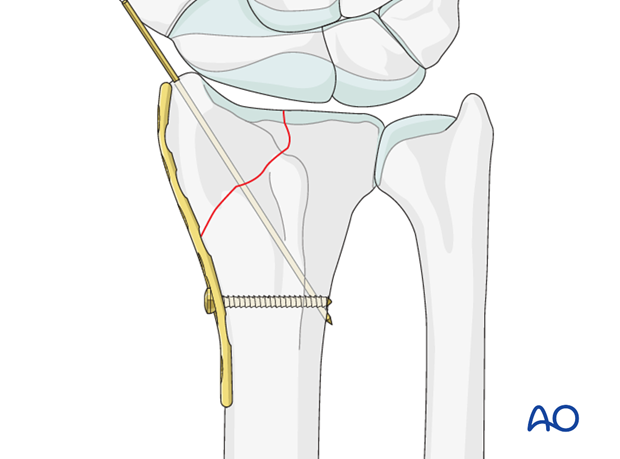
Insert first screw
Insert a conventional screw through the oblong plate hole. The screw should engage the far cortex.
Confirm plate position using image intensification. Fine tuning of the plate position is still possible before the conventional screw is tightened.
Insert first locking head screw
To prevent rotation of the plate during distal subchondral locking screw fixation, the plate should be secured to the bone, by inserting the most proximal screw.
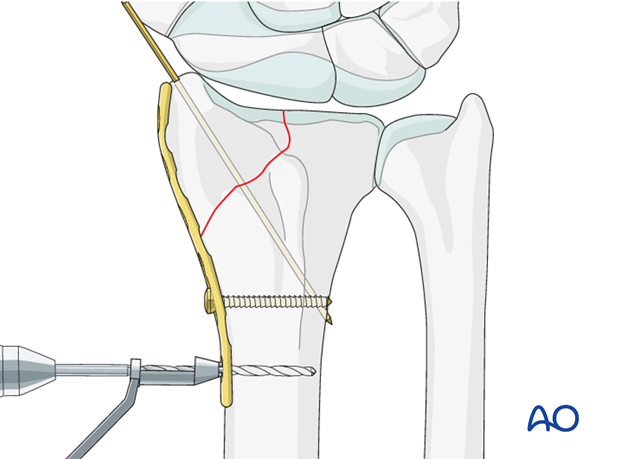
To avoid overtightening the locking screws in the locking screw plate hole, it is mandatory to use the torque limiting device.
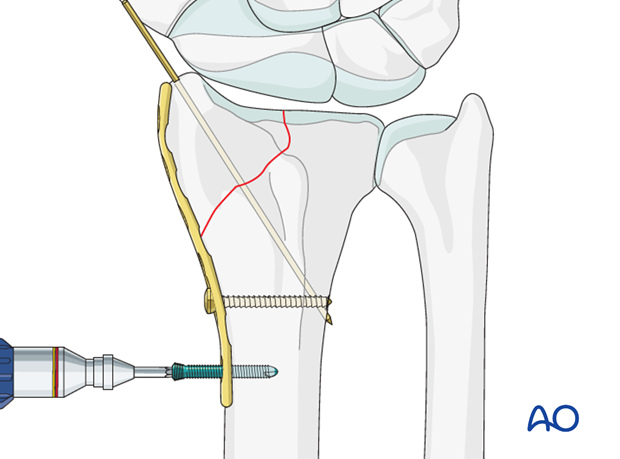
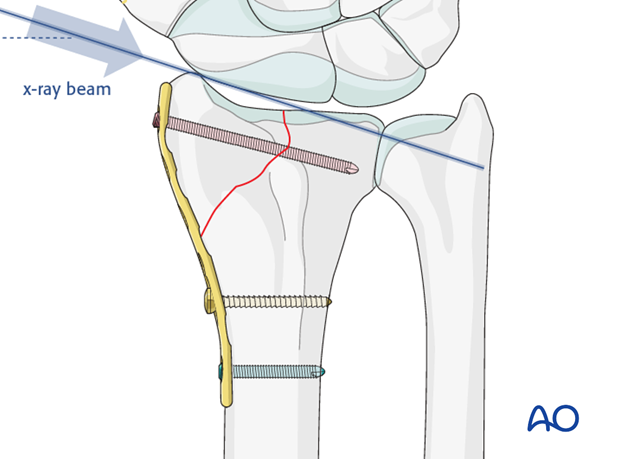
Insert subchondral distal locking head screw
Insert a locking head screw into the distal locking hole of the plate.
The screw should be placed in a subchondral position.

Confirm that the screw does not protrude into the joint using an image intensifier, with the beam angled 20º from the true lateral. This projection will profile the radial articular surface and visualize any encroachment of the screw into the joint.
8. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation, the uninjured side should be tested as a reference for the injured side.
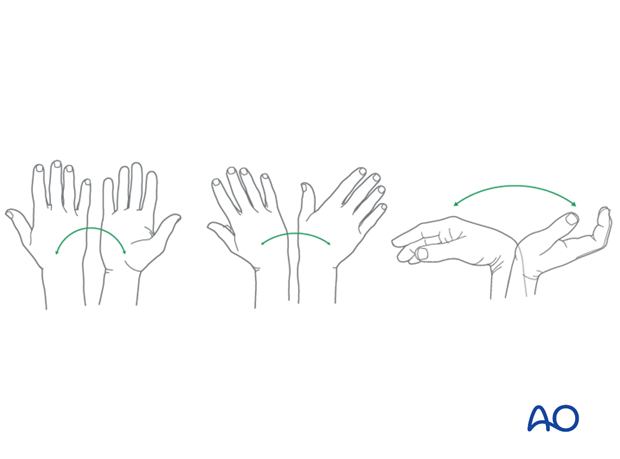
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
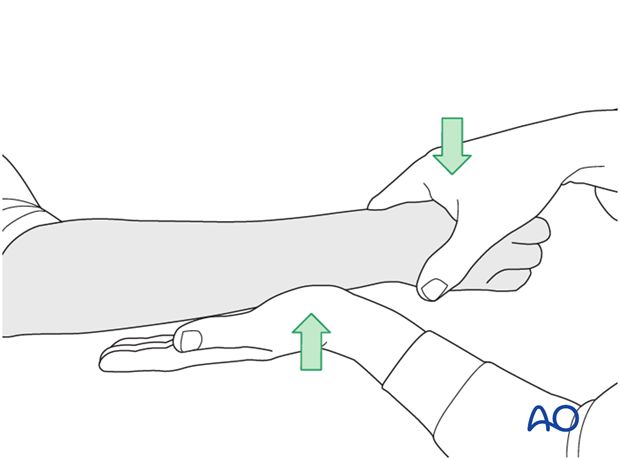
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
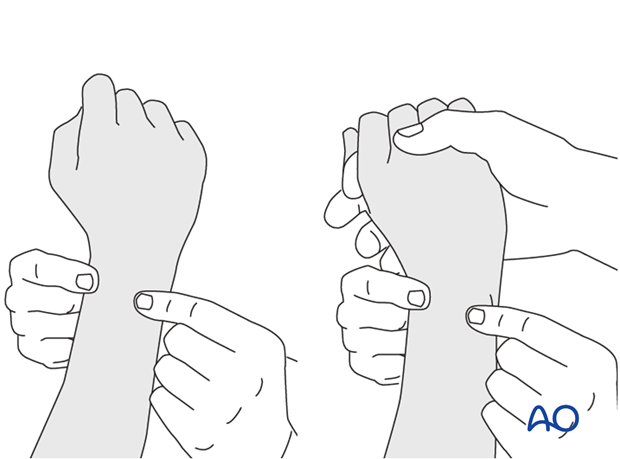
This is repeated with the wrist in full supination and full pronation.
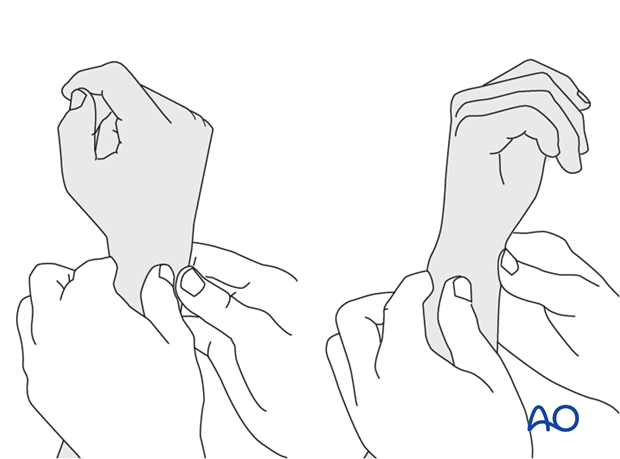
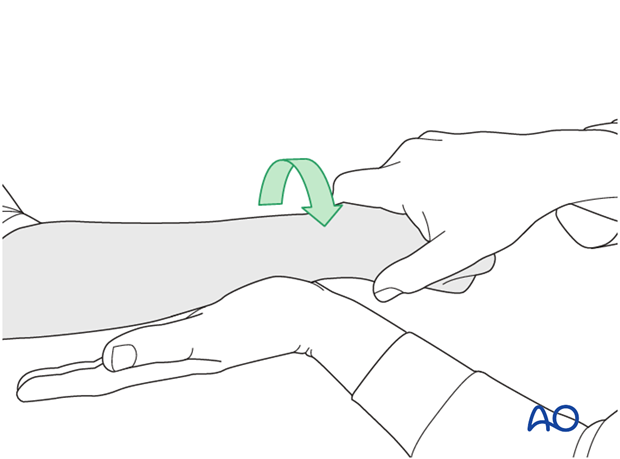
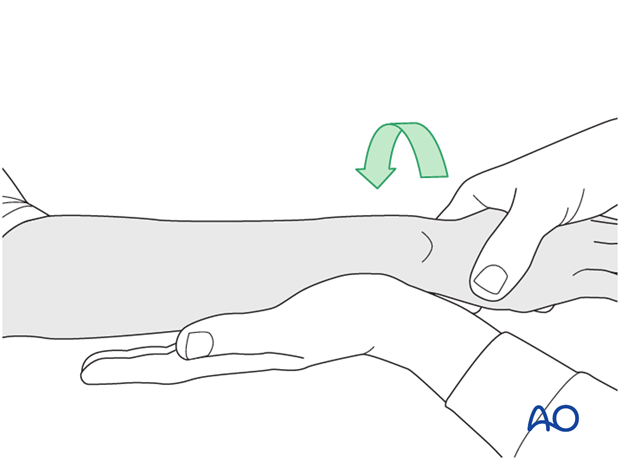
Method 2
To test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
...while the forearm is passively put through full supination...
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
9. Aftercare
Functional exercises
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
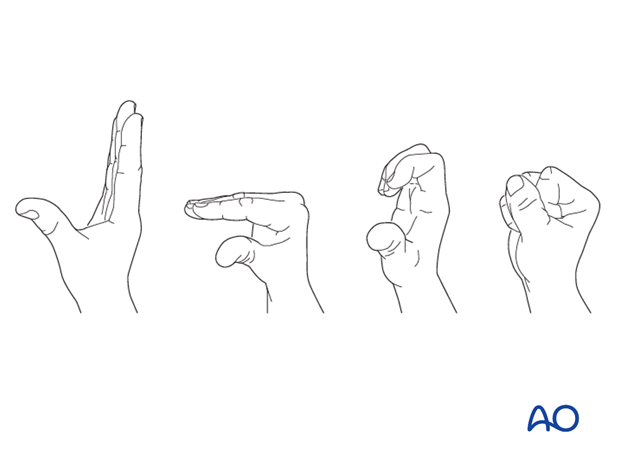
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













