Closed reduction - Lag screws
1. Introduction
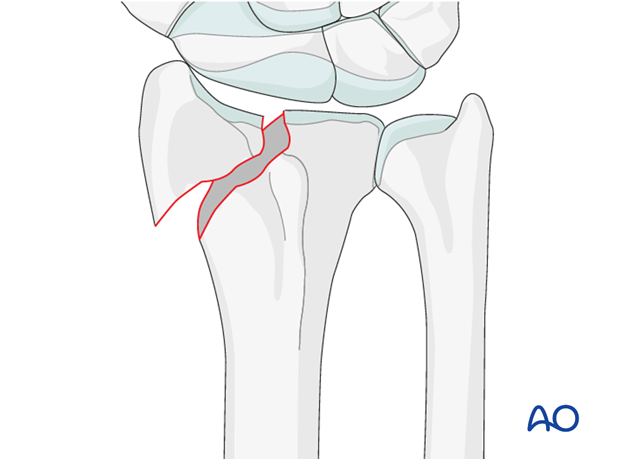
Fracture assessment
These are simple fractures of the radial styloid without comminution. They can occur because of shearing forces.
Access to the radial column may be gained through a dorsal approach using a retinacular incision between the first and second compartment (see dorsal approach for details).
Cannulated / conventional lag screws
If available, cannulated screws would be the preferred choice. If cannulated screws are not available, conventional lag screws may be used. Care should be taken that the K-wire placement does not interfere with screw insertion.
Provisional reduction in displaced fractures
Reduction is achieved by applying longitudinal traction either manually or using Chinese finger traps.
The reduction is maintained by a temporary splint.
If definitive surgery is planned, but cannot be performed within a reasonable time scale, a temporary external fixator may be helpful.

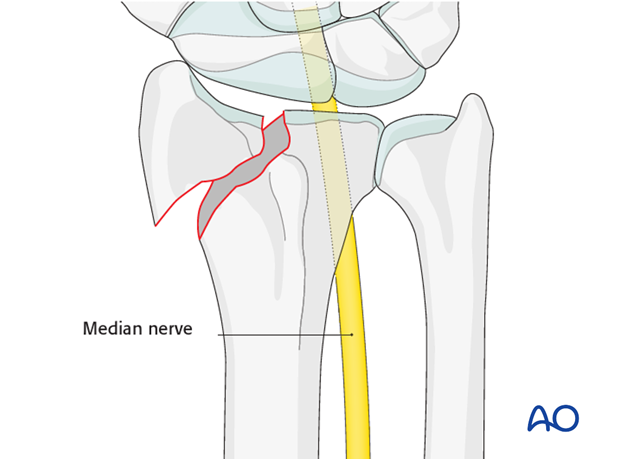
2. Associated injuries
Median nerve compression
If there is dense sensory loss, or other signs of median nerve compression, the median nerve should be decompressed.
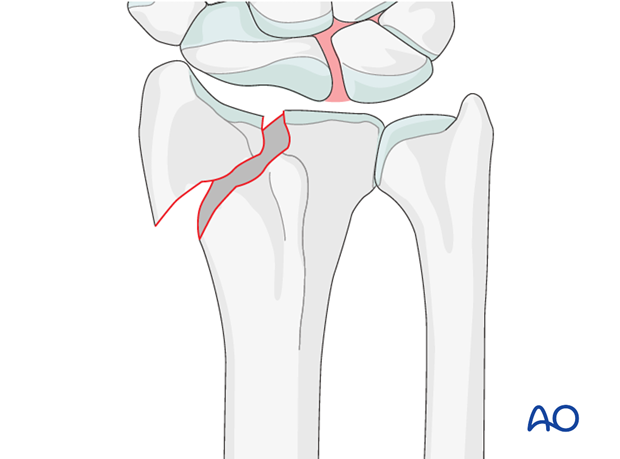
Associated carpal injuries
These injuries may be associated with shearing injuries of the articular cartilage, scaphoid fracture and rupture of the scapholunate ligament (SL). Every patient should be assessed for this injury. If present, see carpal bones of the Hand module.
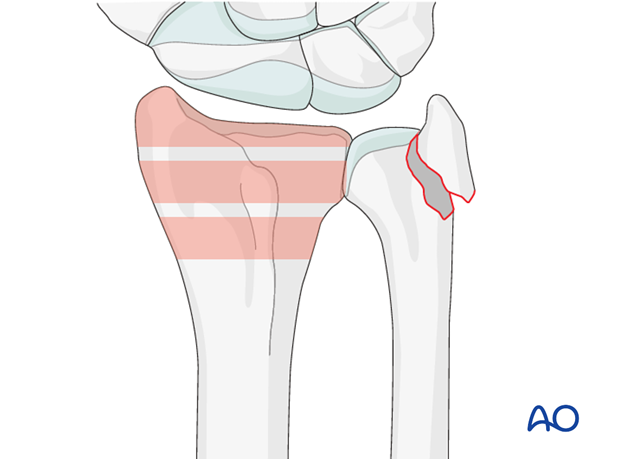
DRUJ/ulnar injuries
These injuries may be accompanied by avulsion of the ulnar styloid and/or disruption of the DRUJ. If there is gross instability after the fixation of the radial fracture, it is recommended that the styloid and/or the triangular fibrocartilaginous disc (TFC) is reattached. This is not common in simple fractures, but may occur with some high energy injuries.
The uninjured side should be tested as a reference for the injured side.
It may not be possible to assess DRUJ stability until the fracture has been stabilized (as described below).
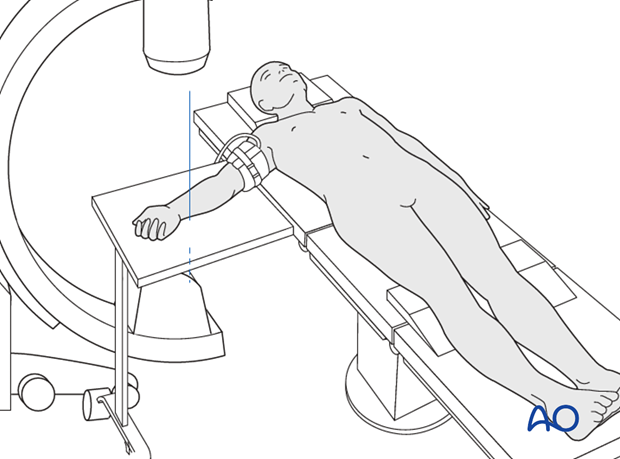
3. Patient preparation
The patient may be placed in a supine position for palmar approaches.
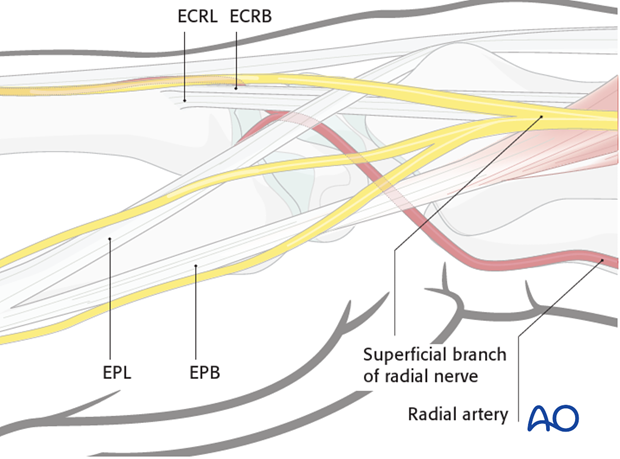
4. Percutaneous approach
It may be possible to reduce and fix the radial styloid through a small percutaneous approach over the tip of the styloid. Care must be taken to avoid damaging important structures in this region.
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
5. Reduction
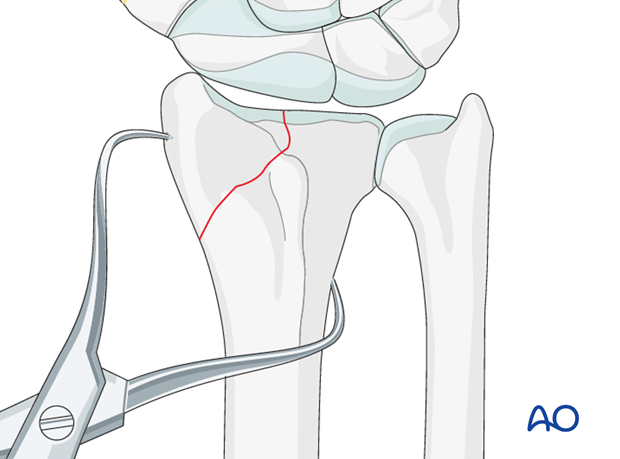
Closed reduction
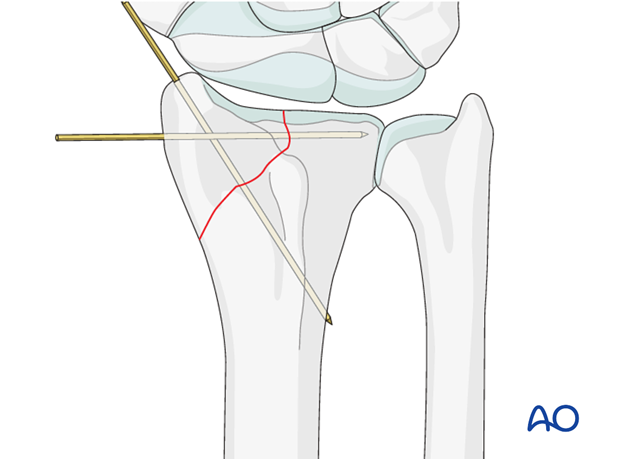
Reduce the fracture using percutaneous pointed reduction forceps, inserted through small stab incisions, or the main small incision over the styloid process.
Confirm the reduction, using image intensification.
Insert a guide wire into the styloid fragment as perpendicular as possible to the fracture site.
Pass the wire across the fracture site, gaining purchase in the ulnar cortex of the radius.
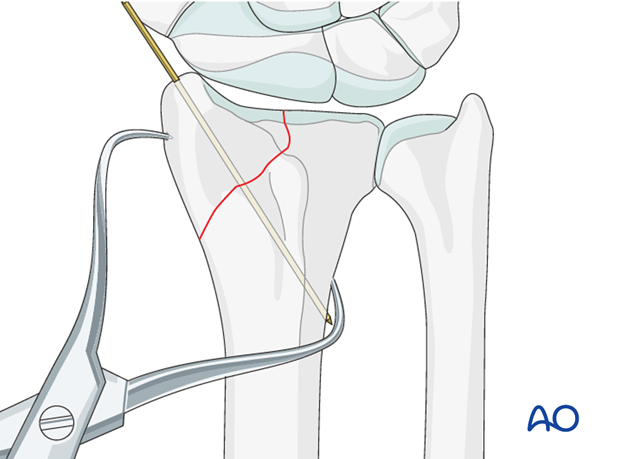
If the fragment is large enough, place a second guide wire as parallel to the joint surface as possible.
Open reduction (if necessary)
If the styloid fragment cannot be reduced closed, the fracture needs to be opened through a standard dorsal incision.
6. Fixation
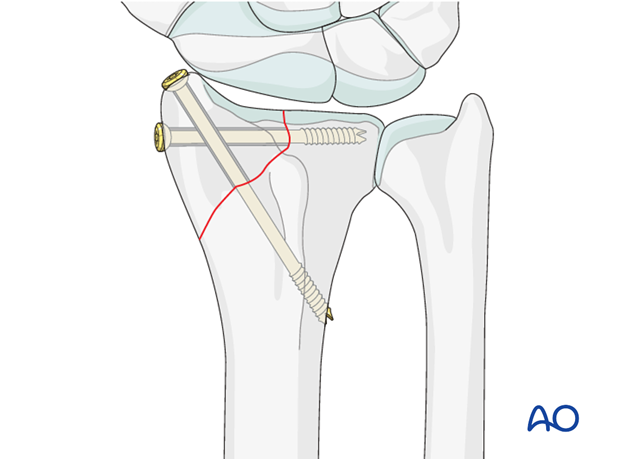
Screw placement
Drill over the guide wires and insert the appropriate screws; the drill should just penetrate the medial cortex of the radius except near the sigmoid notch, where the screw should stop a few mm short.
To obtain the lag effect, either use partially threaded screws or overdrill the hole in the radial styloid.
Use a drill sleeve to ensure that the soft tissues are protected during drilling.
7. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation, the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
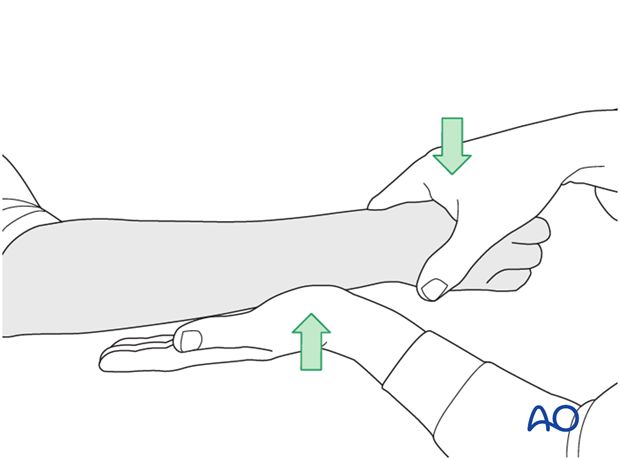
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
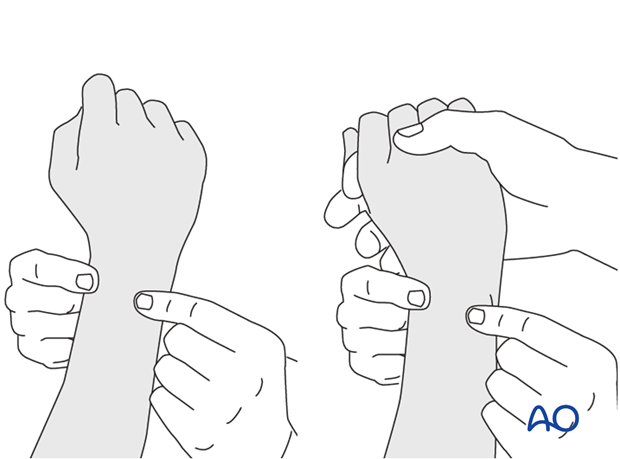
This is repeated with the wrist in full supination and full pronation.
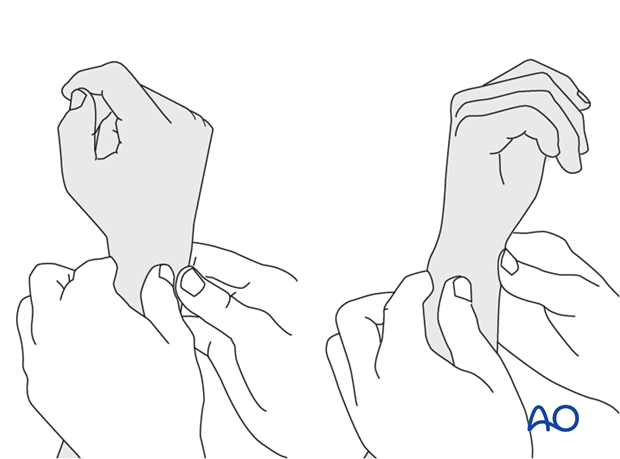
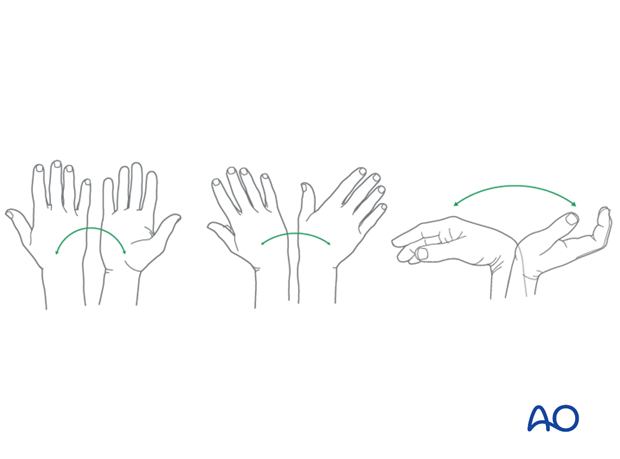
Method 2
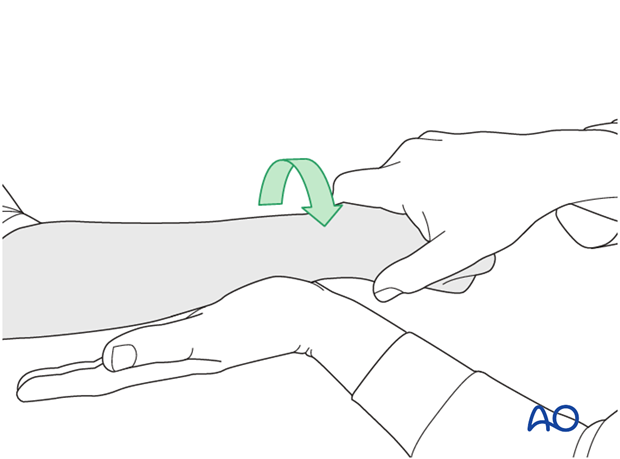
To test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
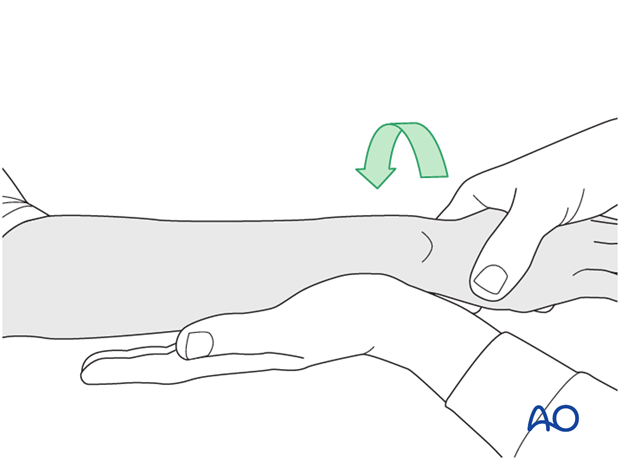
...while the forearm is passively put through full supination...
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
8. Aftercare
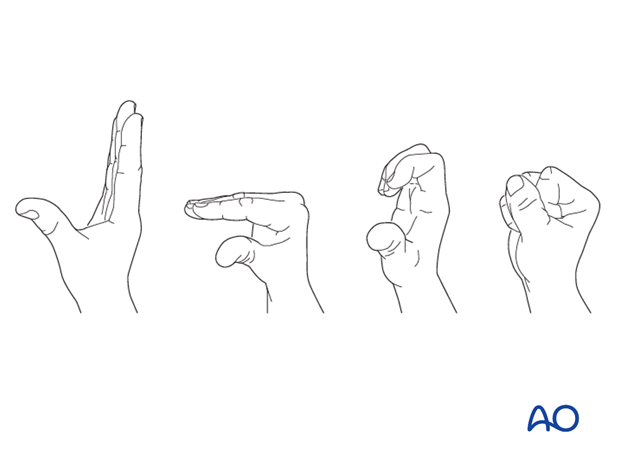
Functional exercises
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













