Closed reduction - K-wires and cast/external fixator
1. Preliminary remarks
Fracture assessment
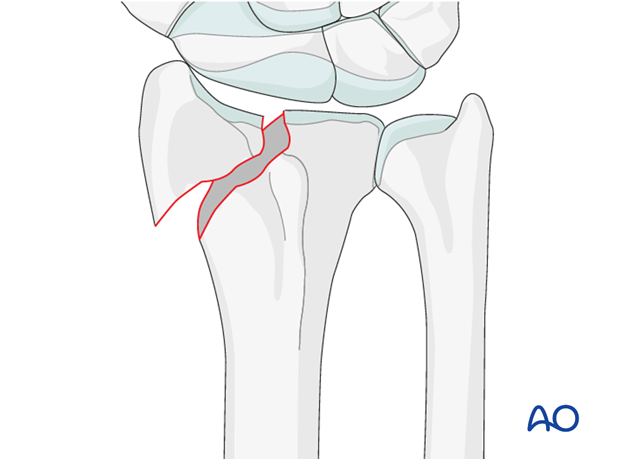
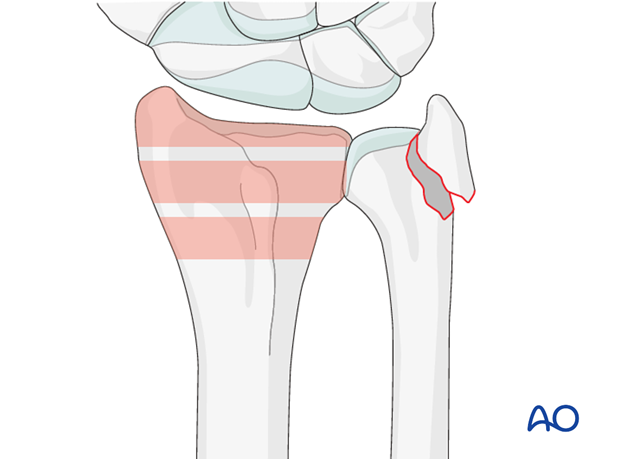
Partial articular fractures demand accurate reduction since they involve the articular surface.
Fractures involving the radial styloid occur because of compression injuries of the scaphoid facet of the distal radius.
Fractures with a simple articular split of the radial styloid may also involve rotation of the radial styloid and/or compression of the articular surface.
CT scans are advisable for preoperative assessment to be sure that it is a simple fracture.
Indications
As these are intraarticular fractures, even if a reasonable reduction is achieved initially, it is very difficult to maintain this with a cast alone. K-wires are usually required to maintain articular congruity.
Anatomy of the wrist
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
2. Associated injuries
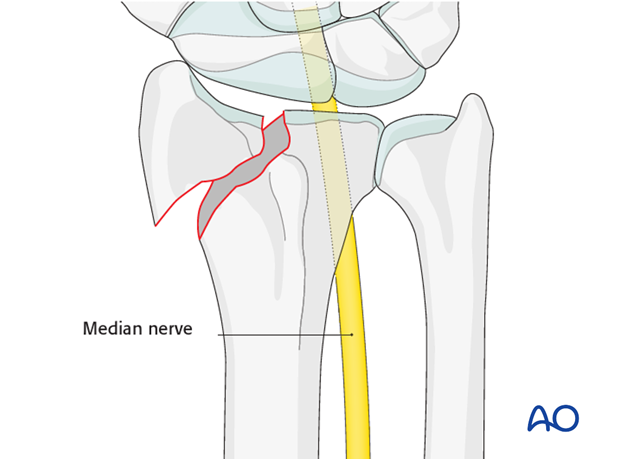
Median nerve decompression
If there is dense sensory loss, or other signs of median nerve compression, the median nerve should be decompressed.
Associated carpal injuries
These injuries may be associated with shearing injuries of the articular cartilage, scaphoid fracture and rupture of the scapholunate ligament (SL). Every patient should be assessed for this injury. If present, see carpal bones of the Hand module.
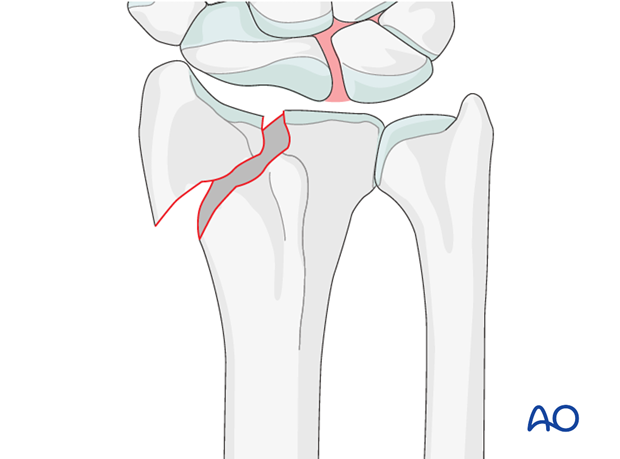
DRUJ/ ulnar injuries
These injuries may be accompanied by avulsion of the ulnar styloid and/or disruption of the DRUJ. If there is gross instability after the fixation of the radial fracture, it is recommended that the styloid and/or the triangular fibrocartilaginous disc (TFC) is reattached. This is not common in simple fractures, but may occur with some high energy injuries.
3. Patient preparation
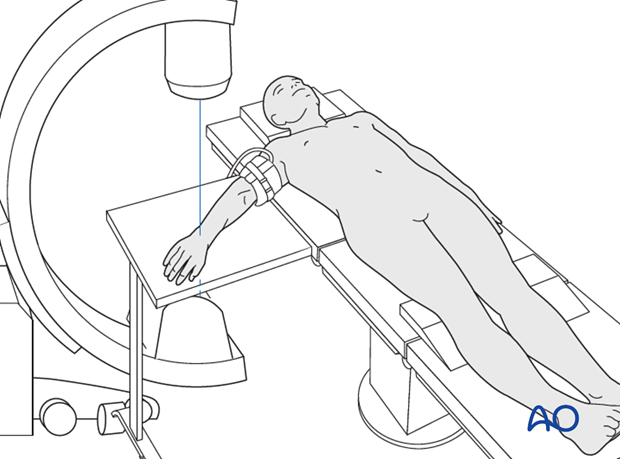
The patient may be placed either in a supine position for palmar approaches or for dorsal approaches.
4. Closed reduction
Traction
Closed reduction can be performed with or without continuous finger traction, e.g., using Chinese finger traps.
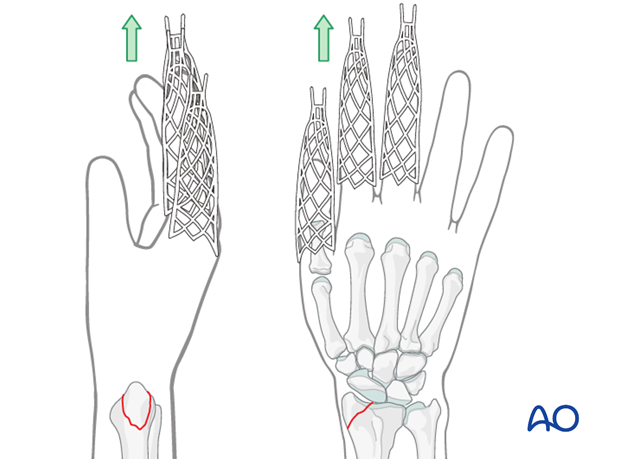
Manual reduction
For radial styloid fractures, closed reduction is achieved by longitudinal manual traction combined with ulnar deviation at the wrist.

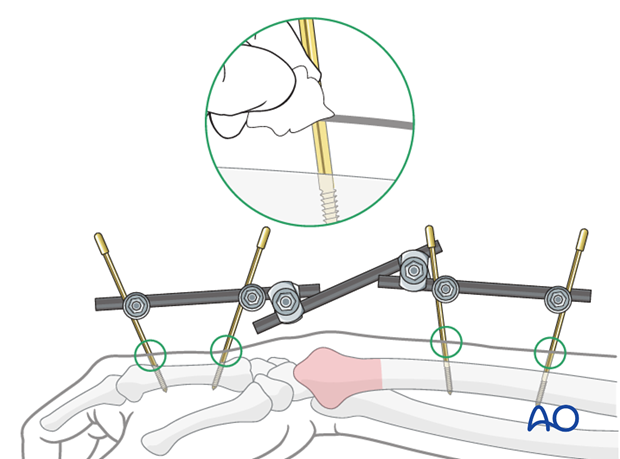
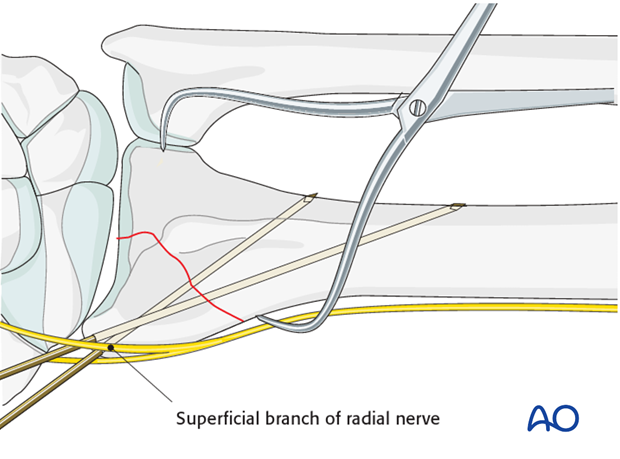
5. Insertion of the first K-wire
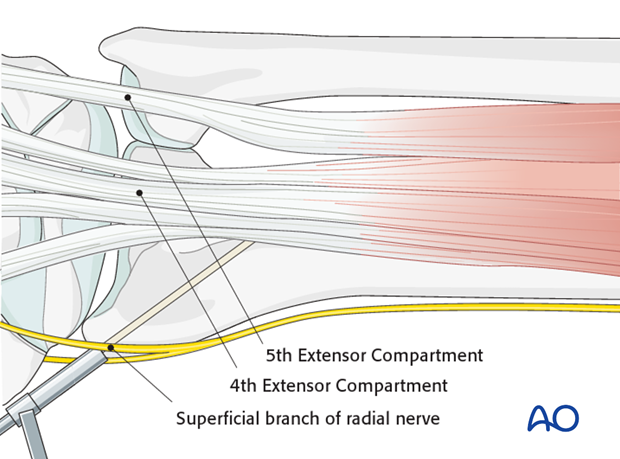
Whilst maintaining the closed reduction, a 1 cm incision is made over the tip of the radial styloid. The radial styloid is exposed by blunt dissection and taking great care is taken not to injure the superficial branch of the radial nerve, or the tendons of the first and third extensor compartments.
The drill guide is introduced between the tips of the soft-tissue spreader.
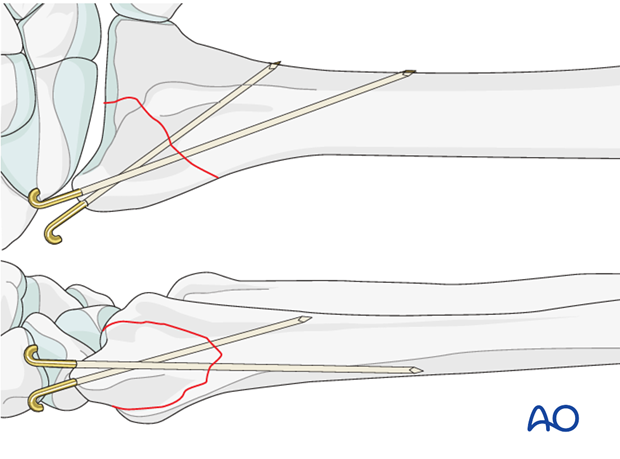
After checking reduction and anticipated direction of the K-wire using image intensification, the K-wire is introduced carefully with a power drill.
The K-wire should just penetrate the opposite cortex of the radial shaft.
Second K-wire
A second K-wire is introduced through the radial styloid in a similar manner, in a divergent direction.
Cut and bend K-wires
The ends of the wires should be cut and bent.
The ends may be left underneath the skin, to reduce the possibility of pin-track infection.
6. Cast application
For more details on casting techniques, see nonoperative treatment options.
A well-padded cast is applied.
One option to consider is creating a window in the cast directly over the pin site.
Because the reduction is stabilized with K-wires, a below elbow cast is preferred, and molding is less important.

7. Aftercare
Functional exercises
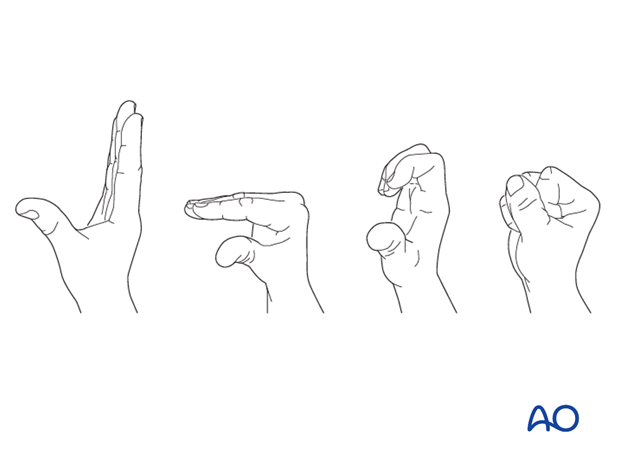
As soon as possible, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.

If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and/or suture removal. X-rays are taken to check the reduction. Refer to your local protocol for timing of X-ray follow-up.
K wire removal
The K-wires are usually removed at about 6-8 weeks. If the wires were buried, it may be necessary to take the patient to the OR to reopen the incisions and retrieve the wires.
Cast removal
The cast is left in place for 4-6 weeks. An x-ray will document fracture position at this time.
Exfix management
The patient needs to be instructed in pin care and should clean the insertion sites daily.
The external fixator is usually left in place for six weeks, but in very unstable fractures or where there are delays in fracture healing it may be left for longer. Excessively long application of an external fixator risks joint stiffness.
The timing of external fixator removal is influenced by various factors. These include the specific details of the fracture and patient, and the radiological appearance of the healing fracture.