Joint-spanning external fixation (temporary or definitive)
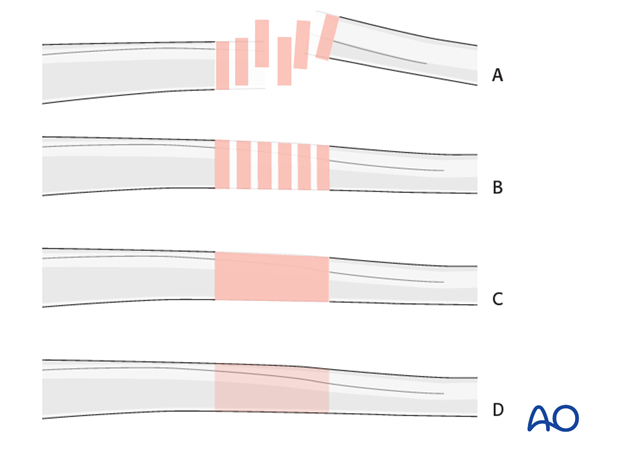
1. Note on illustrations
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fracture
B) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
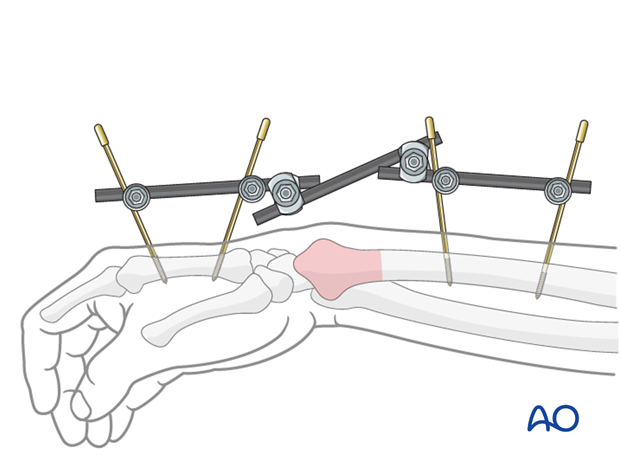
2. Principles of joint-spanning external fixation
Joint-spanning external fixation of the wrist may be used as a temporary or definitive treatment in simple or complex distal forearm fractures.
The external fixator may be used on its own or to supplement K-wire fixation. Specifics of K-wire fixation are given in separate treatment options for each appropriate fracture type.
Details of external fixation are described in the basic technique for application of modular external fixator.
Specific considerations for the wrist are given below.
In joint-spanning external fixation of the wrist, the 4 mm (small) external fixator system is commonly used and may be combined with the 8 mm (medium) system. They are applied as described in the basic technique for the 11 mm (large) system.
There are several other external fixation systems available.
Teaching video
AO teaching video: Distal Radius - Small External Fixator: Wrist-spanning Frame
3. Patient preparation
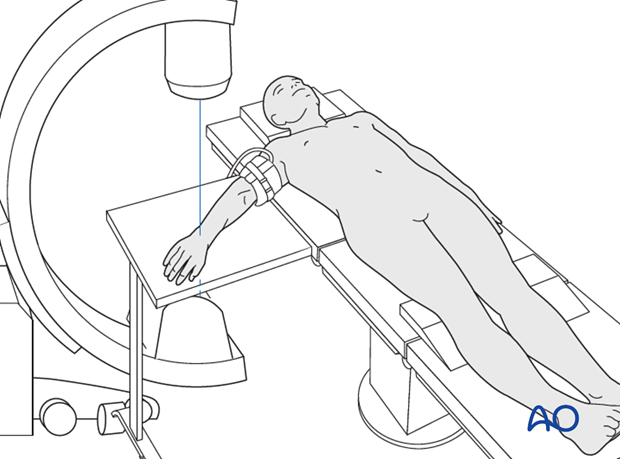
The patient is placed in a supine position for dorsal approaches.
4. Pin insertion (wrist)
Complications with pin insertion
The following three potential complications are of concern when inserting threaded pins for external fixation:
- Injury to extensor tendons
- Injury to the superficial branch of the radial nerve
- Metacarpal fracture
The following precautions minimize the risk of these complications:
- Knowledge of the anatomy and specific landmarks for pin insertion
- Larger surgical incisions (1 cm over the second metacarpal, longer incision over the radius), instead of stab incisions
- Blunt dissection to the bone
- Predrilling prior to insertion of the pins
Landmarks for pin insertion into the second metacarpal
The distal pin should be inserted proximal to the transition of the metacarpal head into the shaft.
The more proximal pin is inserted distal to transition of the shaft into the metacarpal base.
The pins should obtain a good hold in both cortices.

Pitfall: Eccentric pin positioning
An eccentric position of a pin may weaken the metacarpal, leading to fracture.
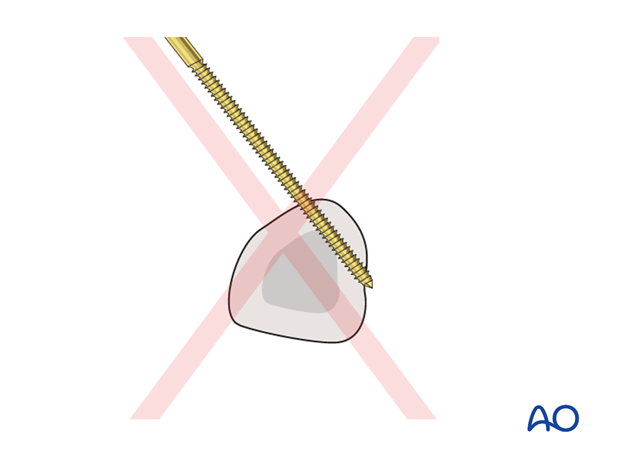
The extensor tendon hood must not be transfixed with the distal metacarpal screw.
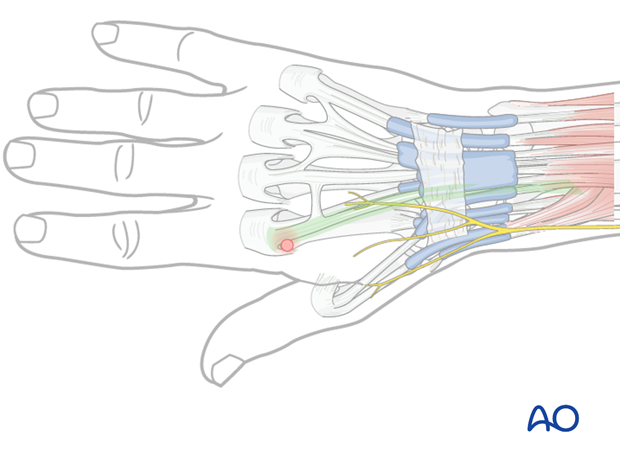
To avoid this complication, the index metacarpophalangeal (MCP) joint should be passively flexed 90° so that the extensor hood moves slightly distally, and the tendons are pulled in an ulnar direction.
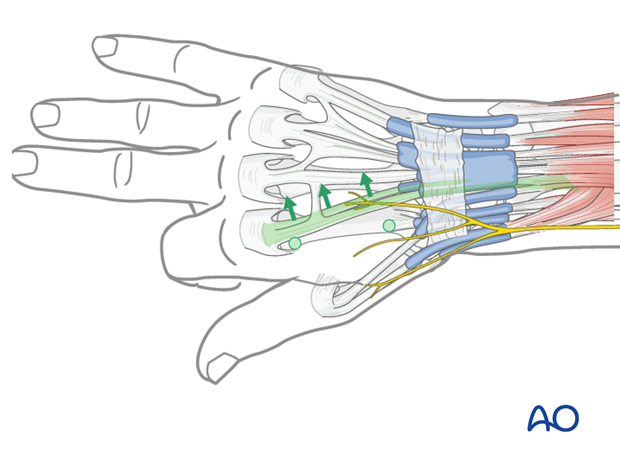
In the frontal plane, the pins should be inserted at an angle of 30°-40° in relation to the sagittal plane to avoid transfixing the extensor tendon/hood.

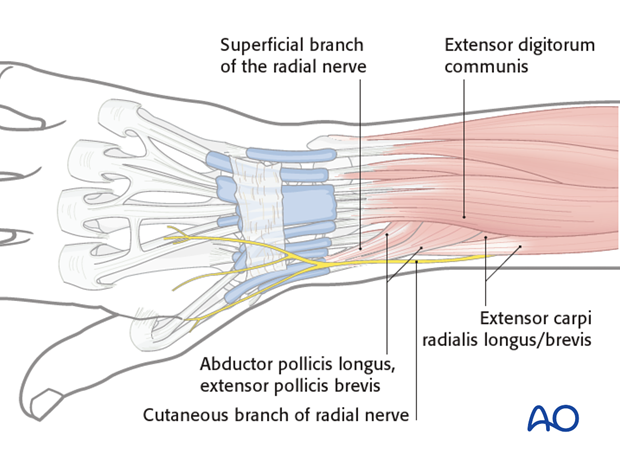
Landmarks for pin insertion in the radial shaft
The proximal two pins should be inserted proximal to the muscle bellies of abductor pollicis longus (APL) and extensor pollicis brevis (EPB), and should not penetrate them.
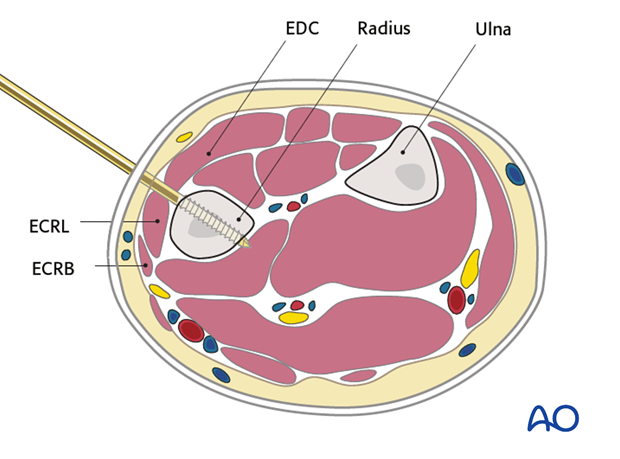
These muscles are usually easy to identify. Proximal to these muscles, the radial shaft can be palpated through the skin between the bellies of the extensor digitorum communis (EDC) and extensor carpi radialis longus/brevis (ECRL/ ECRB) over 3-4 cm. This is the preferred area for proximal pin insertion in the radial shaft.
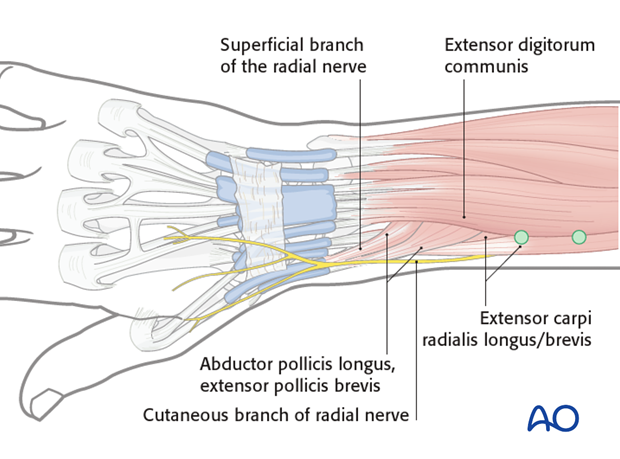
The pins are inserted perpendicular to the transverse section of the radius.
5. Frame construction / reduction and fixation (wrist)
Reduction and fixation
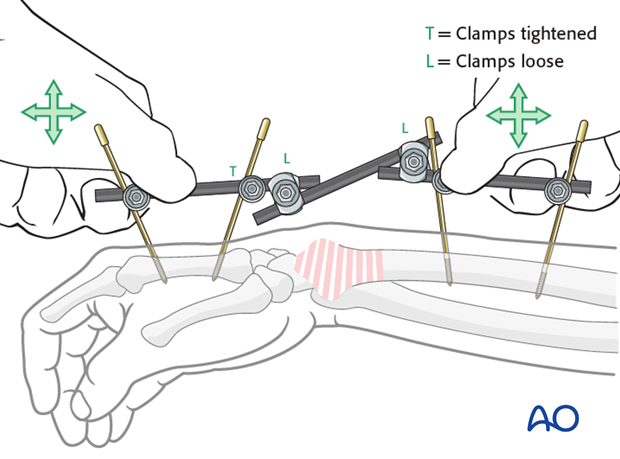
Longitudinal traction is applied on the thumb and index finger or the distal partial frame to reduce the fracture. Additional maneuvers may be necessary depending on the specific fracture pattern. Pressure from the dorsal side of the carpus may be helpful to restore volar tilt of the distal radius joint surface.
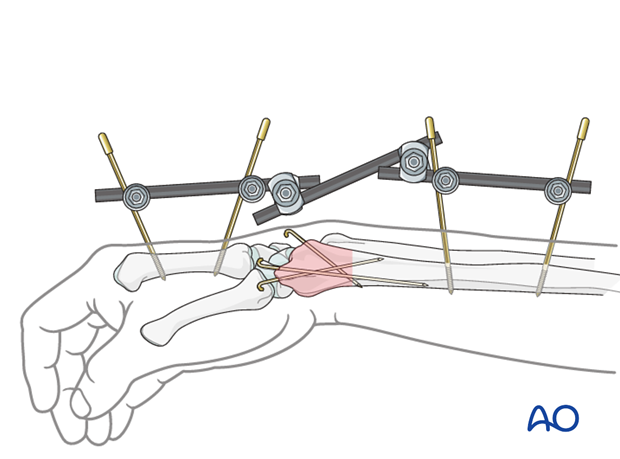
Additional K-wires
In multifragmentary fractures, additional K-wires may be inserted percutaneously, if the external fixator is used as a definitive treatment.
For details of K-wire insertion see the corresponding treatment option for the specific fracture type.
6. Aftercare following external fixation
Pin-site care
Proper pin insertion
To prevent postoperative complications, pin-insertion technique is more important than any pin-care protocol:
- Correct placement of pins (see safe zones) avoiding ligaments and tendons, eg tibia anterior
- Correct insertion of pins (eg trajectory, depth) avoiding heat necrosis
- Extending skin incisions to release soft-tissue tension around the pin insertion (see inspection and treatment of skin incisions)
Pin-site care
Various aftercare protocols to prevent pin tract infection have been established by experts worldwide. Therefore no standard protocol for pin-site care can be stated here. Nevertheless, the following points are recommended:
- The aftercare should follow the same protocol until removal of the external fixator.
- The pin-insertion sites should be kept clean. Any crusts or exudates should be removed. The pins may be cleaned with saline and/or disinfectant solution/alcohol. The frequency of cleaning depends on the circumstances and varies from daily to weekly but should be done in moderation.
- No ointments or antibiotic solutions are recommended for routine pin-site care.
- Dressings are not usually necessary once wound drainage has ceased.
- Pin-insertion sites need not be protected for showering or bathing with clean water.
- The patient or the carer should learn and apply the cleaning routine.
Pin loosening or pin tract infection
In case of pin loosening or pin tract infection, the following steps need to be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for a microbiological study to guide appropriate antibiotic treatment if necessary.
Before changing to a definitive internal fixation an infected pin tract needs to heal. Otherwise infection will result.
Functional exercises
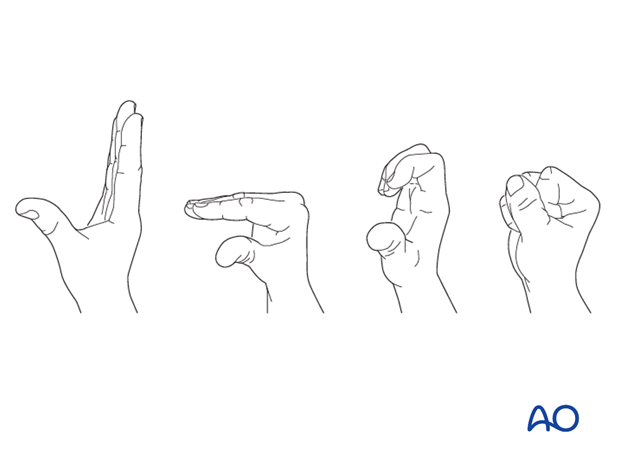
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
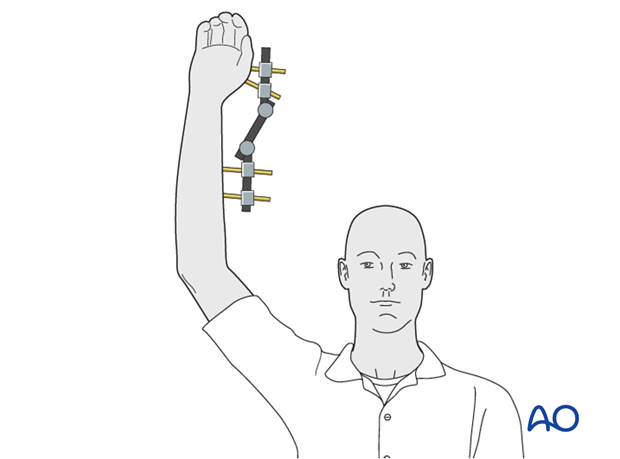
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check. X-rays are taken to check the reduction.
Implant removal
If external fixation is used for definitive treatment, the fixator (and K-wires if used) is usually left in place for six weeks.
The timing of removal may be influenced by various factors. These include the specific details of the fracture and patient, and the radiological appearance of the healing fracture.













