Closed reduction - K-wires and cast/external fixator
1. Preliminary remarks
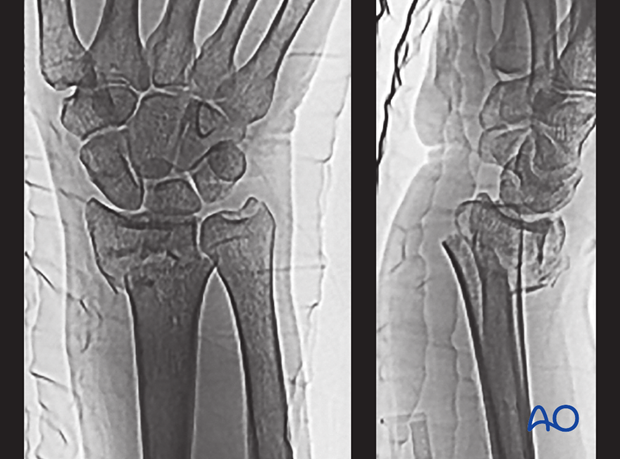
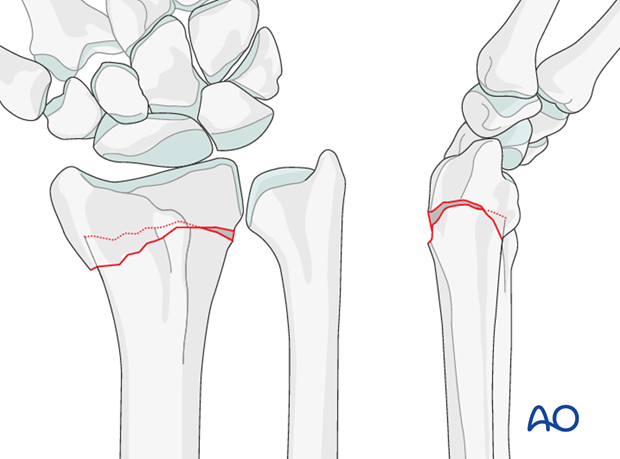
Fracture assessment
These are fractures of the distal metaphysis with dorsal displacement. These are often referred to as Pouteau or Colles fractures.
If shortening of the radial metaphysis results in relative ulnar overlength, painful ulnar impaction may occur.
Fractures angulated dorsally >25°, associated with osteoporosis, or with dorsal metaphyseal comminution, will prove unstable after closed manipulative reduction, and may require additional support.
Indications
Fractures, which seem stable enough to treat in a cast may not need additional K-wires. If there is concern about stability, or if initial reduction in a cast has failed, sufficient additional stability may be obtained with the addition of K-wires.
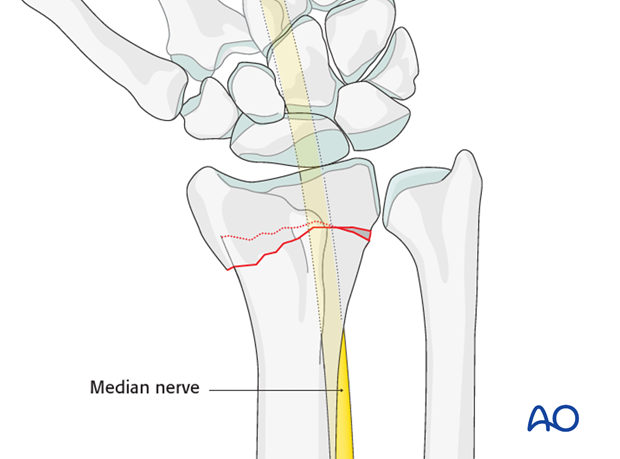
Anatomy of the wrist
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
2. Associated injuries
Median nerve decompression
If there is dense sensory loss, or other signs of median nerve compression, the median nerve should be decompressed.
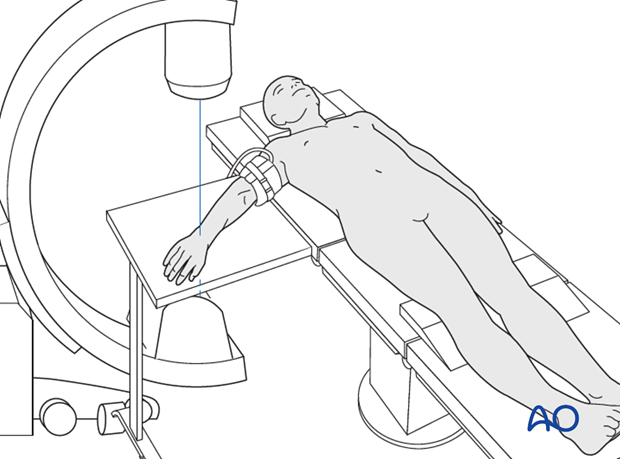
3. Patient preparation
The patient may be placed either in a supine position for palmar approaches or for dorsal approaches.
4. Closed reduction
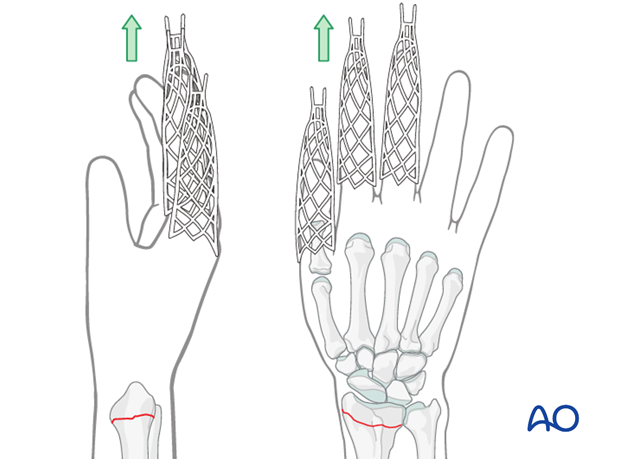
Traction
Closed reduction can be performed with or without continuous finger traction, e.g., using Chinese finger traps.
Manual reduction
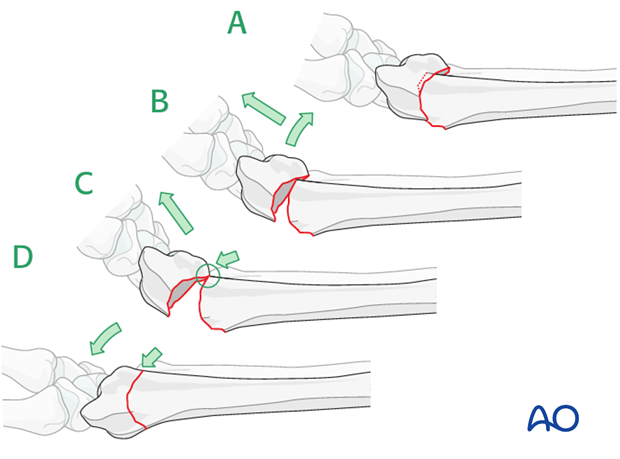
If there are impacted fragments, the first step in reduction is to disimpact these fragments. It may be necessary to release the traction and exaggerate the deformity to achieve this.
As a principle, the first step in reduction is to disimpact the fragment by increasing the dorsal angulation (B). Then, with traction applied, the distal fragment is pushed distally, and flexed (C + D), to reduce the palmar cortex and restore palmar inclination.
5. K-wire insertion
Preliminary remarks
There are numerous techniques of K-wire fixation (e.g., two wires, three wires, Kapandji-technique) for fractures of the distal radius.
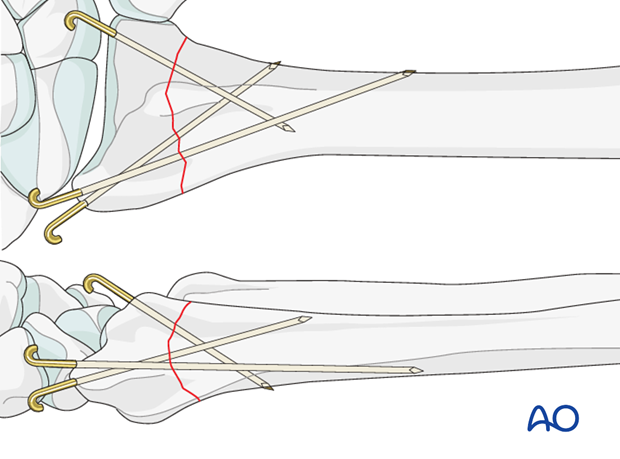
We describe a technique using three K-wires. Two are introduced from the tip of the radial styloid, one from the dorsoulnar aspect.
Insertion of the first smooth K-wire
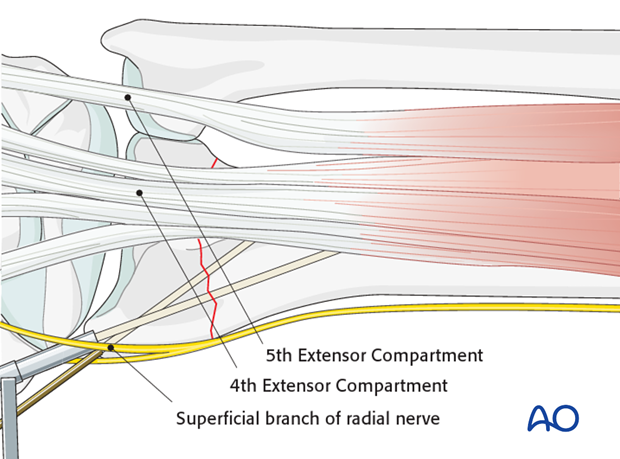
First, a 1 cm incision is made over the tip of the radial styloid. The radial styloid is exposed by blunt dissection and great care is taken not to injure the superficial branch of the radial nerve or the tendons of the first and third extensor compartments. The drill guide is introduced between the tips of the soft-tissue spreader.
After checking reduction and anticipated direction of the K-wire using image intensification, the K-wire is introduced carefully with a power drill.
The K-wire should just penetrate the opposite cortex of the radial shaft.
When inserting the first K-wire, additional control of the distal fragment may be necessary. This may be achieved with a small pointed awl, inserted percutaneously.
Second K-wire
A second K-wire is introduced through the radial styloid in the same manner, but in a divergent direction.
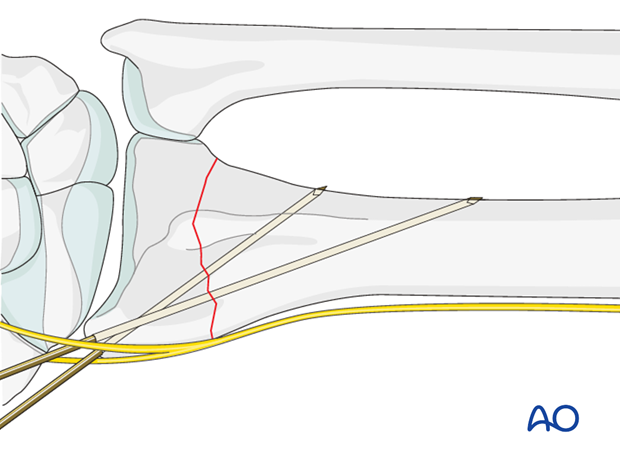
Third K-wire: Insertion from the dorsoulnar aspect
A second incision is made between the fourth and fifth extensor compartments. Blunt dissection to the bone is carried out.
Under image intensifier control, the third K-wire is introduced from the dorsoulnar rim of the radius into the anterior cortex of the radial shaft.
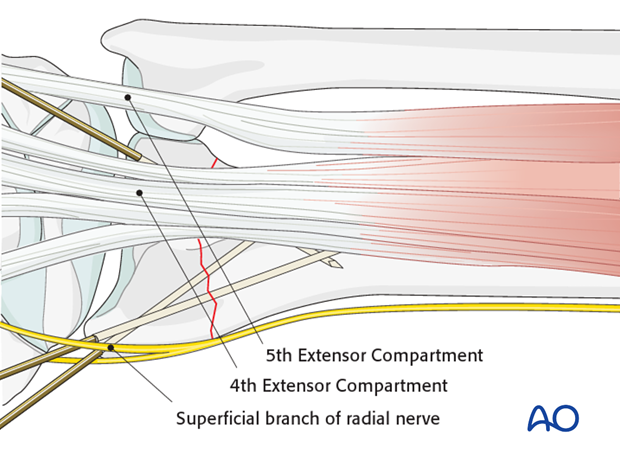
The fourth compartment is displaced radially by the pressure of the thumb, which enables precise K-wire positioning into the dorsoulnar corner of the lunate facet.

Cut and bend K-wires
The ends of the wires should be cut and bent.
The ends may be left underneath the skin, to reduce the possibility of pin-track infection.
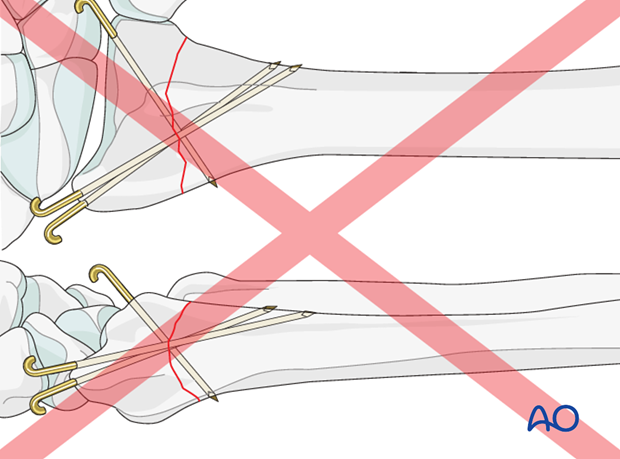
Pitfall: K-wire crossing
The K-Wires should not cross at one point at the fracture level.
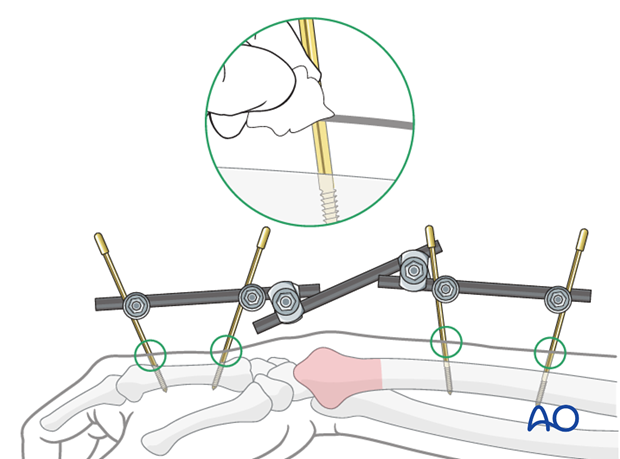
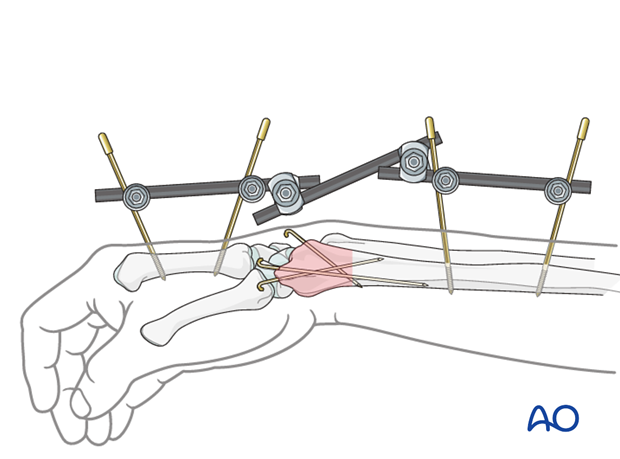
Pearl: Alternative method
If there are concerns about the security of reduction in a cast, particularly a risk of shortening, an external fixator as neutralizing device (without traction) may be preferred after K-wire fixation.
This is particularly useful in extensive metaphyseal comminution or osteoporosis.
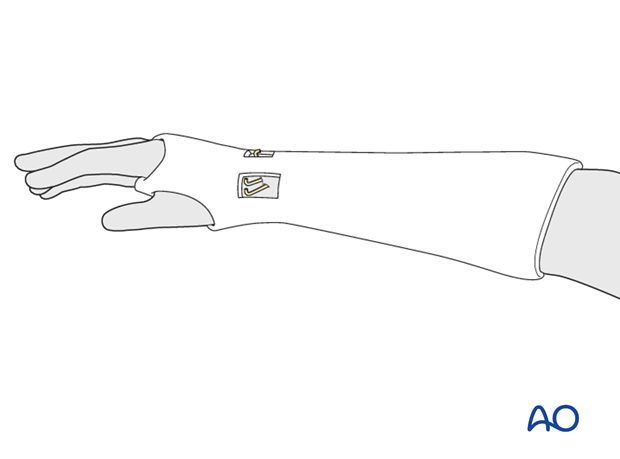
6. Cast application
For more details on casting techniques, see nonoperative treatment options.
A well-padded cast is applied.
One option to consider is creating windows in the cast directly over the pin sites.
Because the reduction is stabilized with K-wires, a below elbow cast is preferred, and molding is less important.
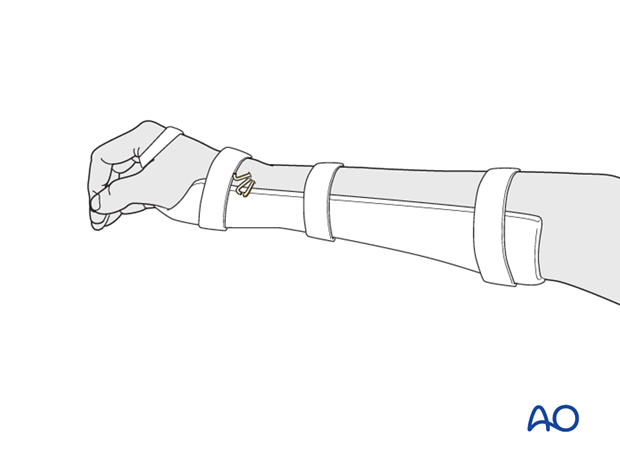
Alternative: Splint
As an alternative to a cast, a removable splint may be used. This gives access for skin care, but requires greater patient compliance.
A well-padded splint is applied on the palmar side, to avoid pressure over the K-wires.
It is imperative that the splint permit full digital motion, especially metacarpophalangeal flexion.
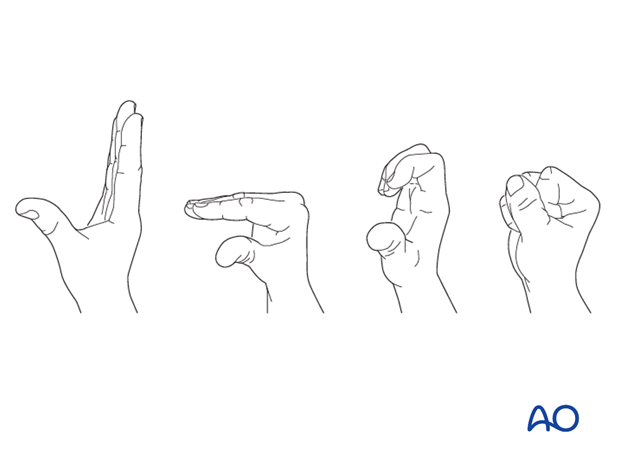
7. Aftercare
Functional exercises
As soon as possible, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.

If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and/or suture removal. X-rays are taken to check the reduction. Refer to your local protocol for timing of X-ray follow-up.
K wire removal
The K-wires are usually removed at about 6-8 weeks. If the wires were buried, it may be necessary to take the patient to the OR to reopen the incisions and retrieve the wires.
Cast removal
The cast is left in place for 4-6 weeks. An x-ray will document fracture position at this time.
Exfix management
The patient needs to be instructed in pin care and should clean the insertion sites daily.
The external fixator is usually left in place for six weeks, but in very unstable fractures or where there are delays in fracture healing it may be left for longer. Excessively long application of an external fixator risks joint stiffness.
The timing of external fixator removal is influenced by various factors. These include the specific details of the fracture and patient, and the radiological appearance of the healing fracture.