ORIF - Dorsoradial double plate
1. Preliminary Remarks
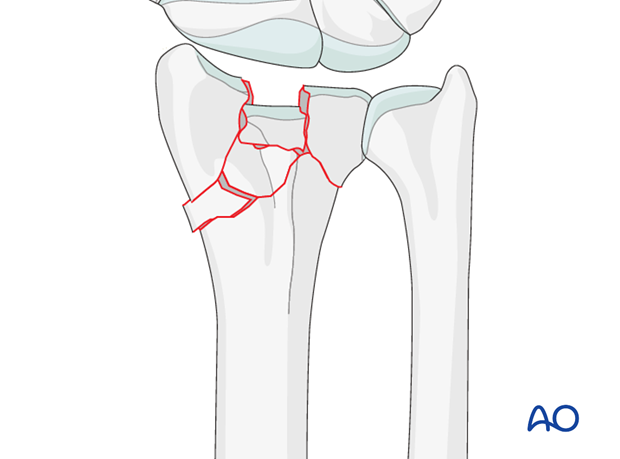
These are complete articular fractures of the distal radius.
As these are intraarticular fractures, where possible, they should be treated with anatomic reduction and absolute stability in order to minimize the risk of subsequent degenerative changes in the joint.
Anatomical reduction and stabilization of these articular fractures is also essential because of the functional implications of the involvement of the distal radioulnar joint.
These are among the most common fractures seen and treated in the older population, with underlying osteoporosis.
When these fractures occur in younger individuals, they are more likely to be the result of high energy trauma, with associated soft-tissue, or skeletal injuries.
It is not possible to make an accurate assessment of the details of these injuries without a CT scan.
Provisional reduction in displaced fractures
Reduction is achieved by applying longitudinal traction either manually or using Chinese finger traps.
The reduction is maintained by a temporary splint.
If definitive surgery is planned, but cannot be performed within a reasonable time scale, a temporary external fixator may be helpful.

2. Associated injuries
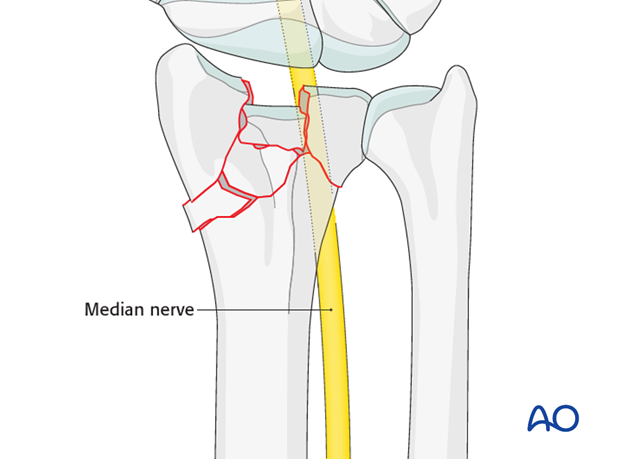
Median nerve compression
If there is dense sensory loss, or other signs of median nerve compression, the median nerve should be decompressed.
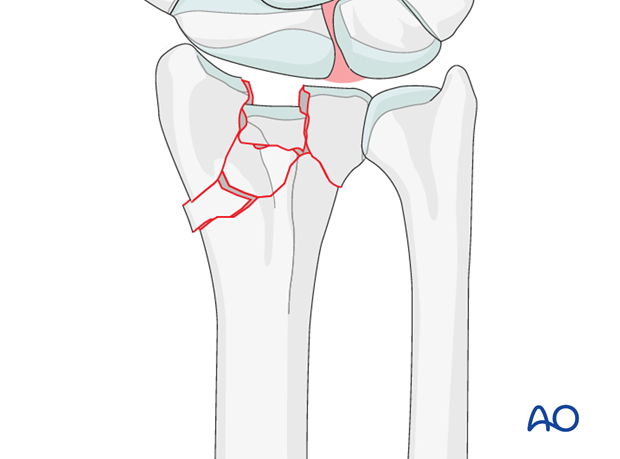
Associated carpal injuries
These injuries may be associated with shearing injuries of the articular cartilage, scaphoid fracture and rupture of the scapholunate ligament (SL). Every patient should be assessed for this injury. If present, see carpal bones of the Hand module.
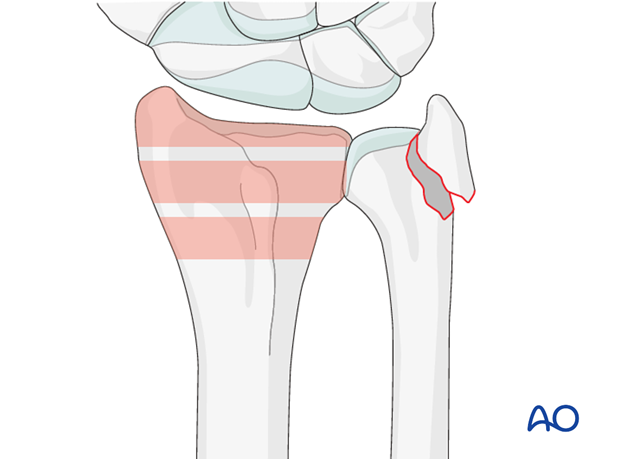
DRUJ/ulnar injuries
These injuries may be accompanied by avulsion of the ulnar styloid and/or disruption of the DRUJ. If there is gross instability after the fixation of the radial fracture, it is recommended that the styloid and/or the triangular fibrocartilaginous disc (TFC) is reattached. This is not common in simple fractures, but may occur with some high energy injuries.
The uninjured side should be tested as a reference for the injured side.
It may not be possible to assess DRUJ stability until the fracture has been stabilized (as described below).
3. Principles
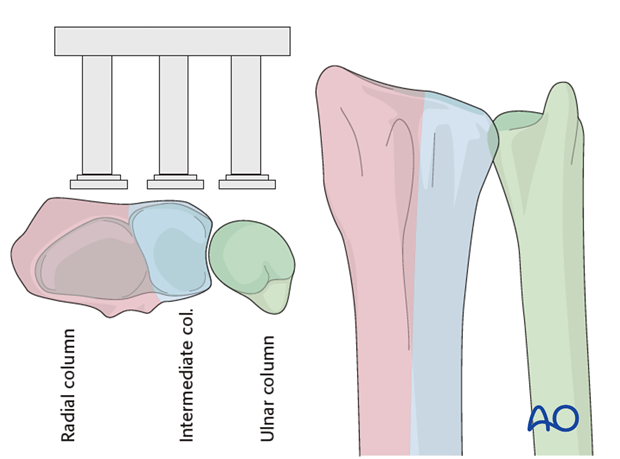
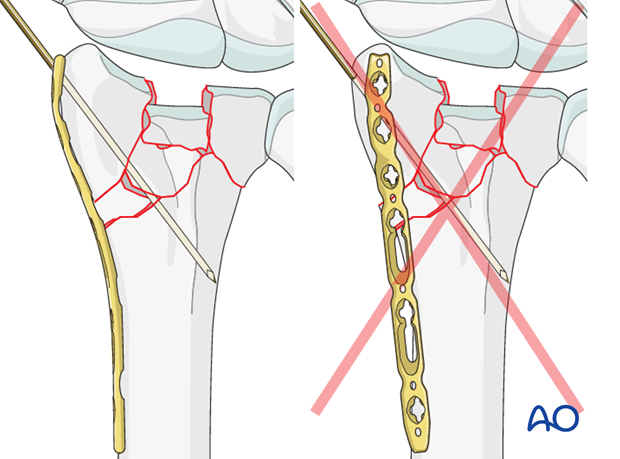
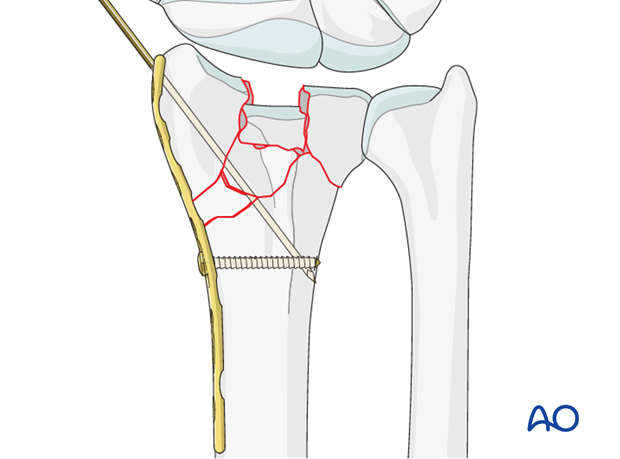
Buttressing the intermediate and radial columns
In dorsal double plating, the intermediate column and the radial column are buttressed, each with a separate plate. The radial column is buttressed by a plate placed radially, deep to the first extensor compartment. The intermediate column is buttressed with a separate, precontoured plate on the dorsal aspect of the intermediate column.
A buttress plate resists axial load by applying a force at 90° to the axis of potential displacement.
4. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position for dorsal approaches.
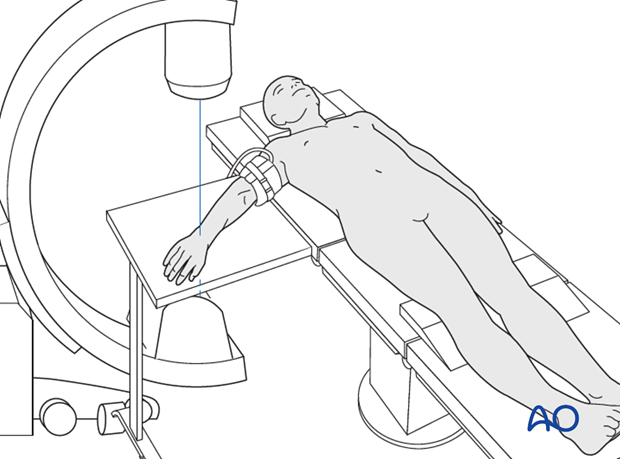
Approach
For this procedure a dorsal approach is normally used.
A thorough knowledge of the anatomy around the wrist is essential. Read more about the anatomy of the distal forearm.
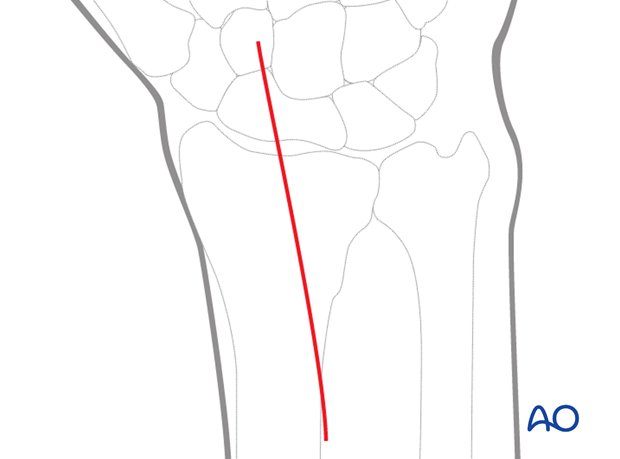
5. Radial column
Applying traction with an external fixator
A temporary joint-bridging external fixator may be used to help hold the preliminary manual reduction and to distract the joint for better inspection.
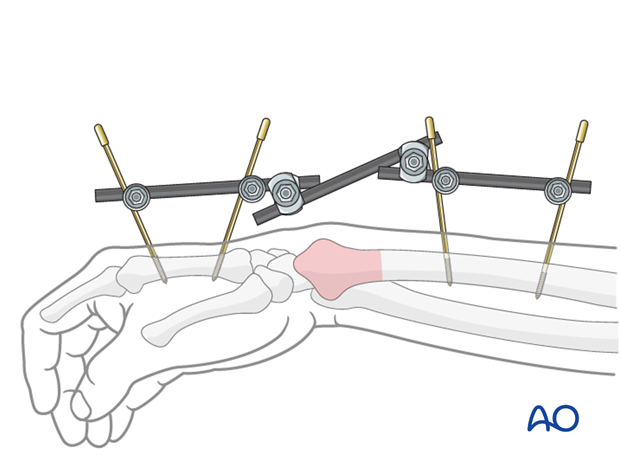
Plate selection
Radial column plates come precontoured. However, some further contouring may be necessary to accommodate the individual anatomy of some patients.
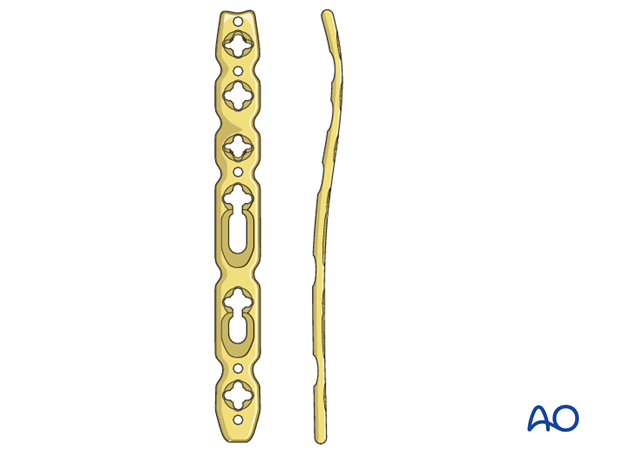
Pitfall: Screw hole distortion
Avoid contouring the plate through the locking holes, otherwise the locking head screw might not fit any more.

Variable angle locking plates enable precise positioning of the distal screws in desired directions, because there is 30° of freedom for each screw inside the plate hole to
address the individual fracture patterns.
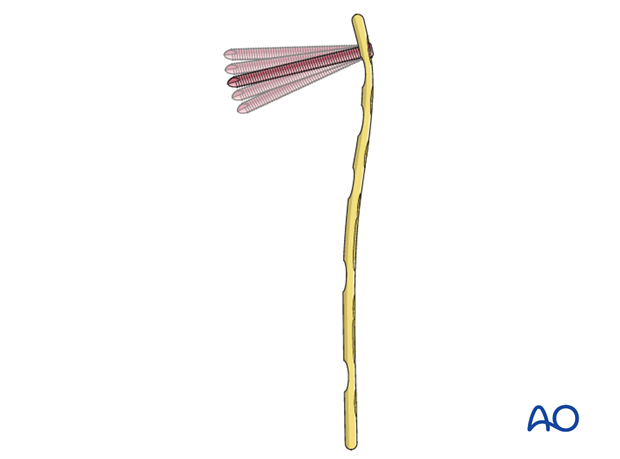
Application of the plate
Slide the plate underneath the first compartment and apply it onto the radial column.
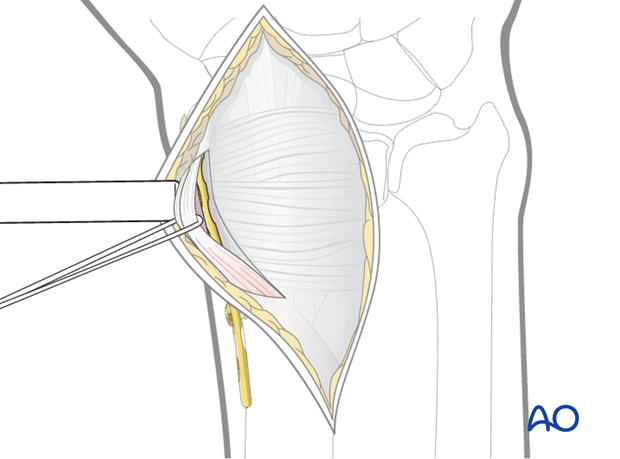
Pitfall: Inadequate buttressing
To create a buttress for the radial styloid, the plate must be positioned correctly on the radial styloid, on its true lateral aspect.
Note
Placement of the plate on the dorsal aspect of the radial column is to be avoided as it will not buttress the reduction adequately against axial shear forces
Insert a standard cortical screw into the oblong hole proximal to the fracture (in the buttress position of the plate). The position of the plate may be adjusted before the screw is tightened.
6. Intermediate column
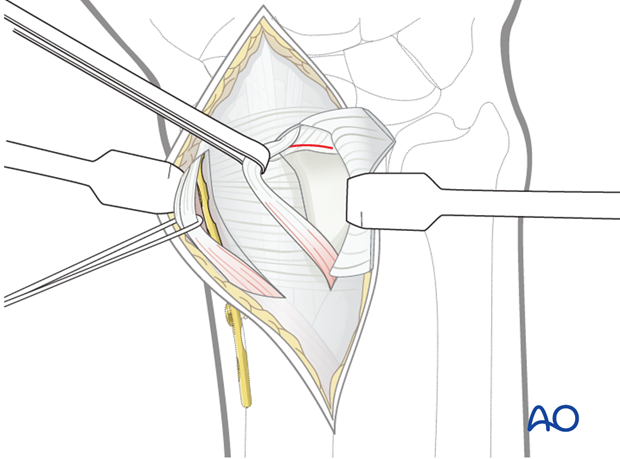
Arthrotomy
If direct vision of the articular surface is needed, a limited, transverse, radiocarpal arthrotomy is performed.
The joint surface is now visible. Check the proximal carpal row for additional ligament injury.
The radial insertion of the triangular fibrocartilage complex can also be checked.
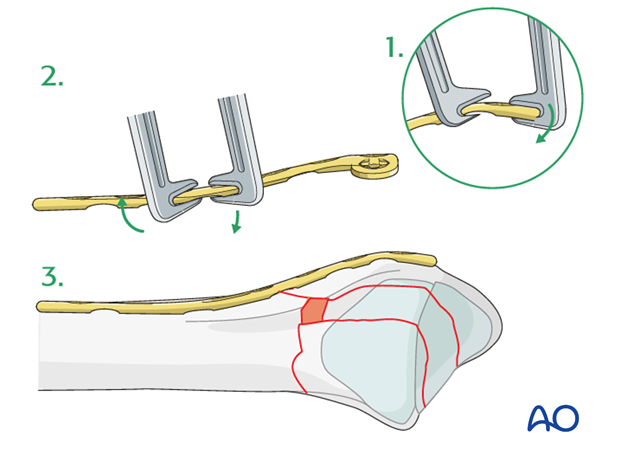
Reduction of articular fragment
The centrally impacted articular fragment is reduced to the level of the radiocarpal joint surface by direct manipulation, using a dissector, or dental pick.
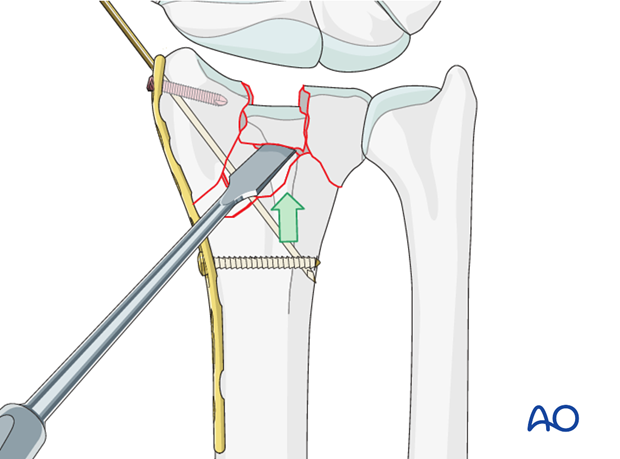
Reduction of dorsoulnar fragment
The dorsoulnar fragment is reduced. The fragment reductions are held with a pointed reduction forceps.
The resulting bony defect, created by the disimpaction, may be filled with bone graft or bone graft substitute.
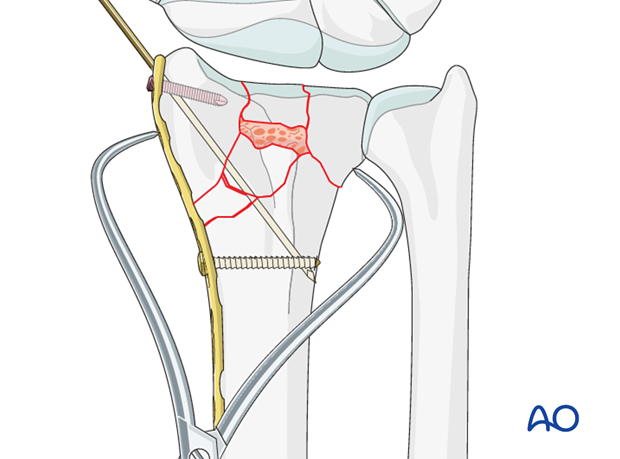
Plate selection and preparation
An appropriate plate is selected according to the fracture configuration. The choice of the plate (T-, or L-shaped) is determined by the fracture pattern. If necessary, the plate can be contoured.
A plate which allows variable angle locking screws may be very useful in this situation.
Pitfall: Screw hole distortion
Avoid contouring the plate through the locking holes, otherwise the locking head screw might not fit any more.

Plate application
The plate is precontoured and positioned so that it buttresses the intermediate column and supports the reconstructed radiocarpal joint surface.
Fix the plate provisionally with a standard cortical screw through the oblong hole.
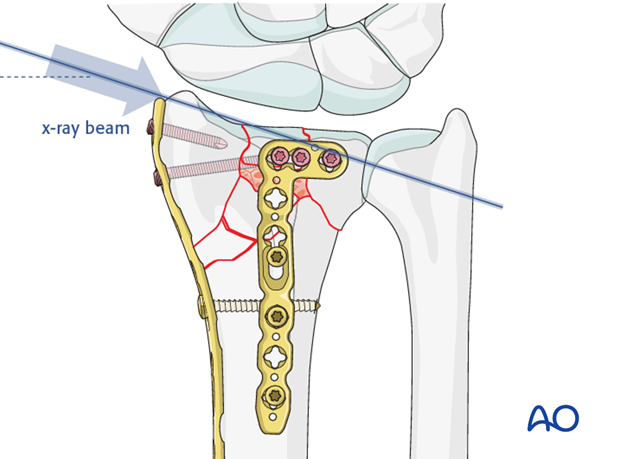
Check the reduction and position of the implants using image intensification.
If necessary, adjust the reduction and plate position, then tighten the screw.
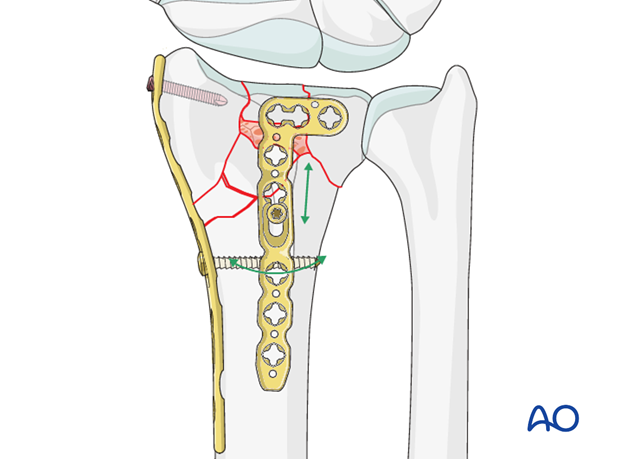
7. Complete the fixation
After confirming the correct position of the plate, it is secured to the diaphysis with a second screw through its most proximal hole. The distal locking head screws are inserted to stabilize the articular fragments.
If a variable angle plate is available, the direction of each screw can be chosen to avoid penetration into the joint.
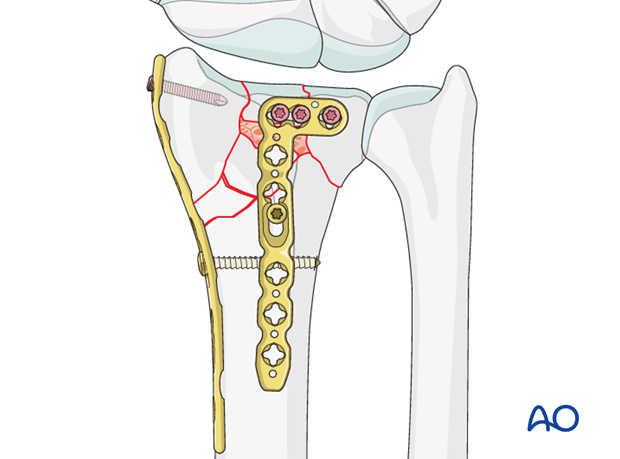
After reconfirming the correct position of the radial column plate, insert distal locking head screw(s) through the most distal hole(s) and remove the K-wire.
Additional screws may be inserted proximal to the fracture, if its configuration permits.
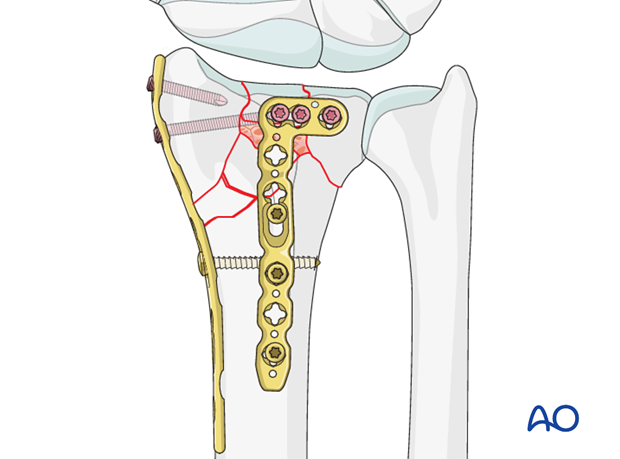
The position of the distal screws is verified by imaging. If the screws appear to enter the radial carpal joint, they can be repositioned if a variable angle locking plate has been used.
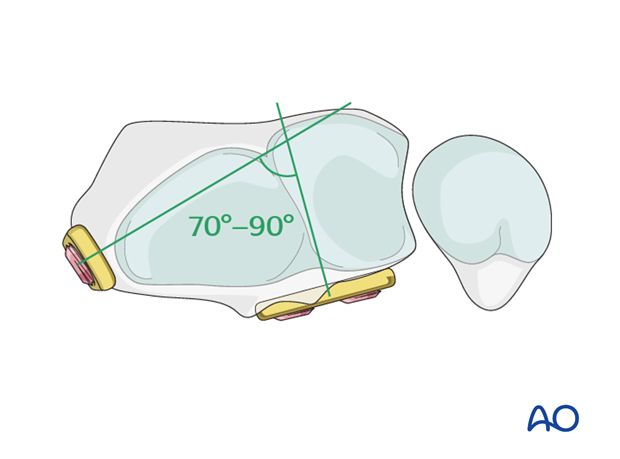
The plates should now form an angle of 70º-90º to each other.
Check osteosynthesis using image intensification.
Finally, unlock the external fixator, if used, and check stability.
8. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation, the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
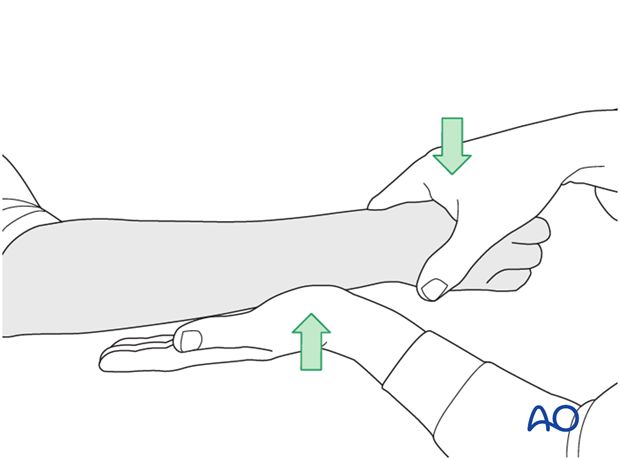
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
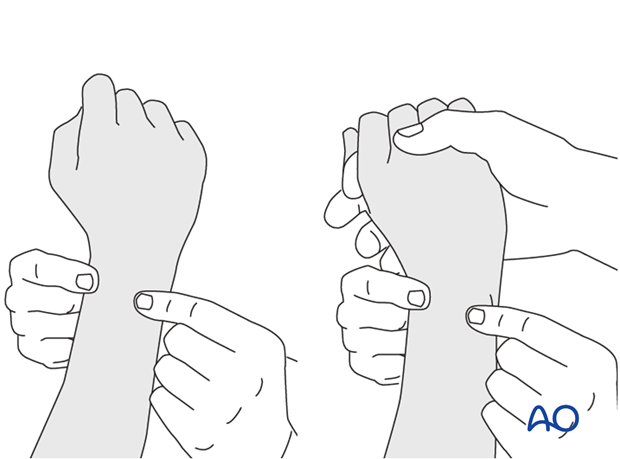
This is repeated with the wrist in full supination and full pronation.
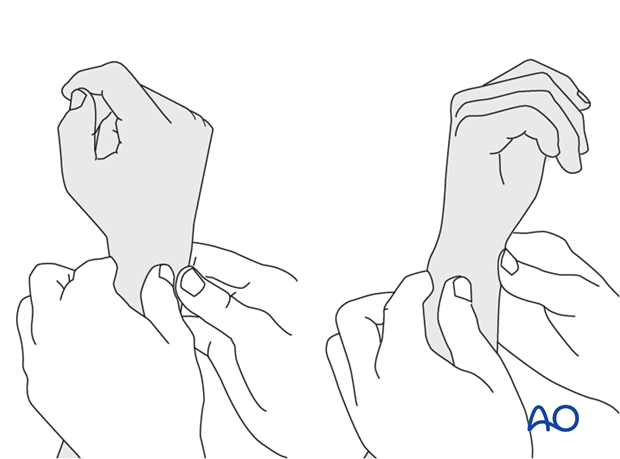
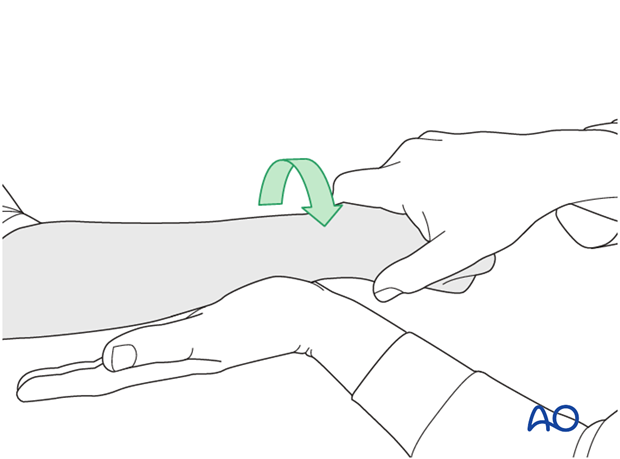
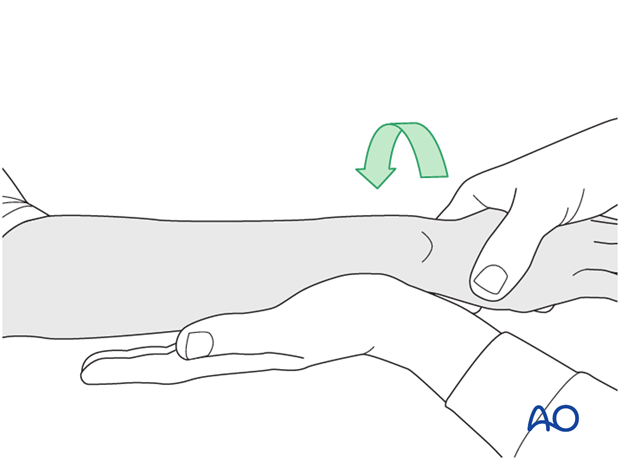
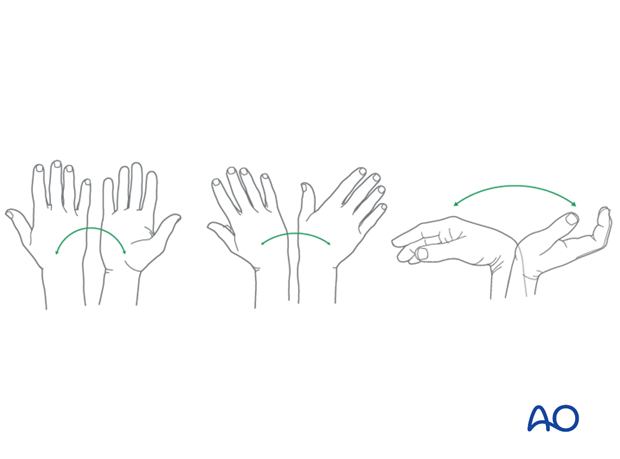
Method 2
To test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
...while the forearm is passively put through full supination...
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
9. Aftercare
Functional exercises
Immediately postoperatively, the patient should be encouraged to elevate the limb and mobilize the digits, elbow and shoulder.
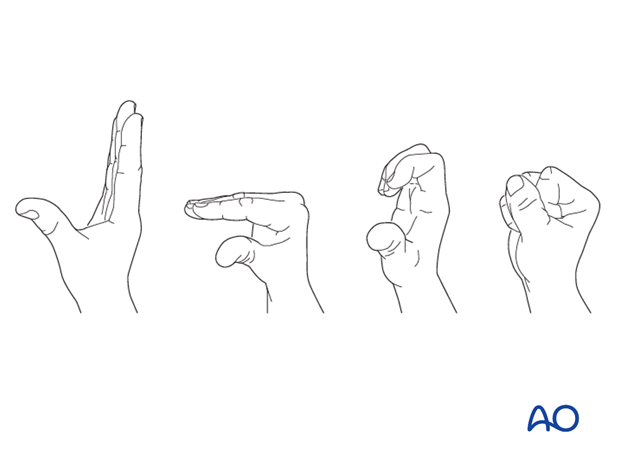
Some surgeons may prefer to immobilize the wrist for 7-10 days before starting active wrist and forearm motion. In those patients, the wrist will remain in the dressing applied at the time of surgery.

Wrist and forearm motion can be initiated when the patient is comfortable and there is no need for immobilization of the wrist after suture removal.
Resisted exercises can be started about 6 weeks after surgery depending on the radiographic appearance.
If necessary, functional exercises can be under the supervision of a hand therapist.
Follow up
See patient 7-10 days after surgery for a wound check and suture removal. X-rays are taken to check the reduction.
Implant removal
Implant removal is purely elective but may be needed in cases of soft-tissue irritation, especially tendon irritation to prevent late rupture. This is particularly a problem with dorsal or radial plates. These plates should be removed between nine and twelve months.













