Flexible intramedullary nail
1. Introduction
Intramedullary nailing of the clavicle is reserved for young and highly active patients who are expected to resume full active function soon after surgery.
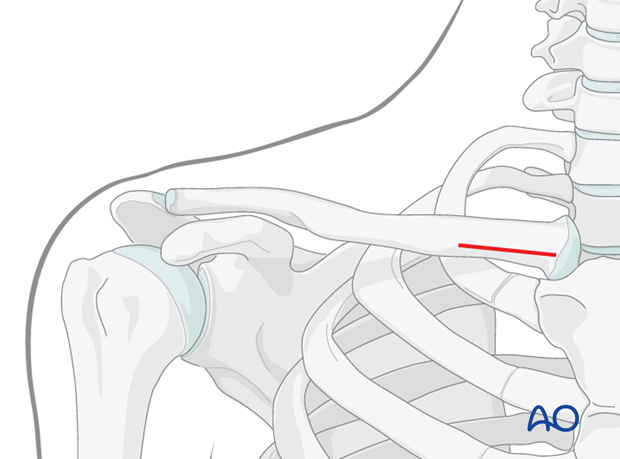
It is also a procedure best reserved for bending- and fragmented-wedge fractures in the middle zone of the clavicle
For technical reasons, other fracture patterns are not suitable for nailing.
This procedure is performed only under image intensifier guidance.
Intramedullary nailing
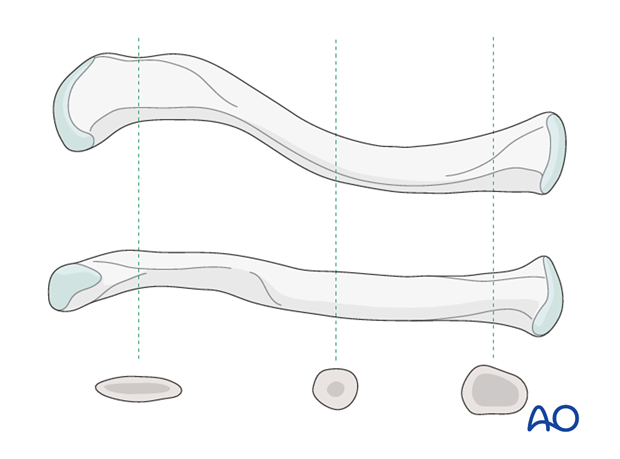
The goal of treatment for these types of fractures of the shaft of the clavicle is to achieve as anatomical reduction as possible and then splint them with intramedullary fixation. The shape of the nail and the shape of the bone maintain alignment and rotation. Shortening is prevented by bone contact.
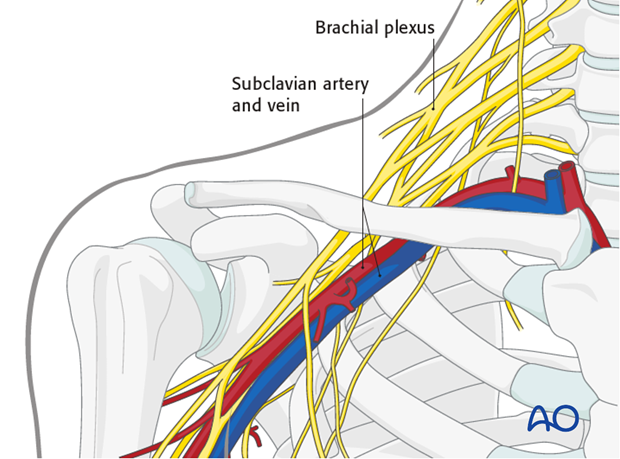
Implant migration and damage to nearby neurovascular structures are potential complications that can be encountered. However, it is a minimally invasive approach that requires less soft tissue dissection, preserves blood supply and biology to improve healing.
Selection of pin
Stiff pins or thick K-wires should be avoided as the limited diameter of the intramedullary canal of the clavicle and its curved anatomy presents inherent difficulties during insertion and stabilization of the fracture. Thus, the procedure described will be with a flexible titanium intramedullary nail.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient either in a beach chair or a supine position.
Approach
For this procedure a nailing approach is used.
3. Reduction and fixation
For intramedullary nailing of clavicular fractures, the following reduction techniques are useful:
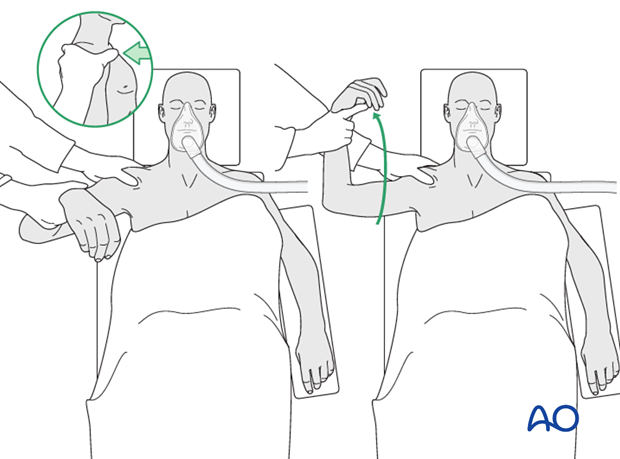
Shoulder manipulation with inline traction and an external rotation moment often helps to reduce the fracture. (The shoulder should be draped free.)
Pointed reduction clamps can be used either percutaneously or through small stab incisions.
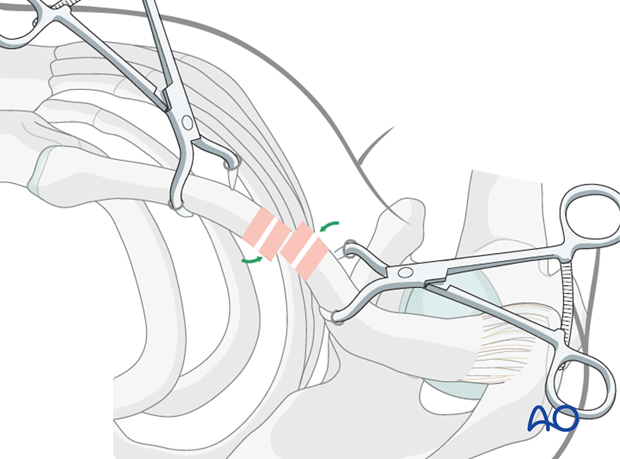
If a closed reduction cannot be achieved, a small incision directly over the fracture site to perform a limited open reduction is helpful and often necessary.
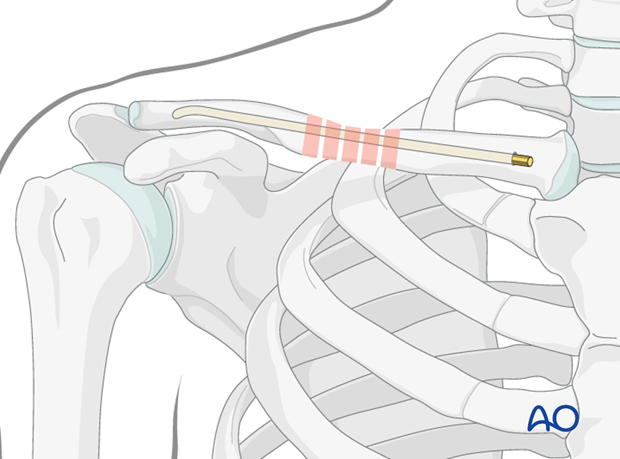
Nail insertion
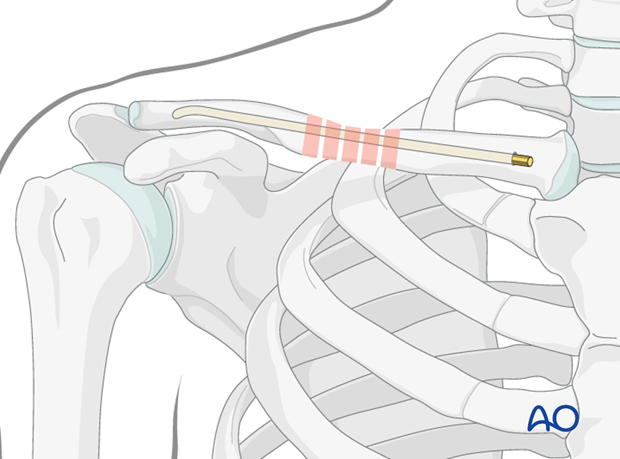
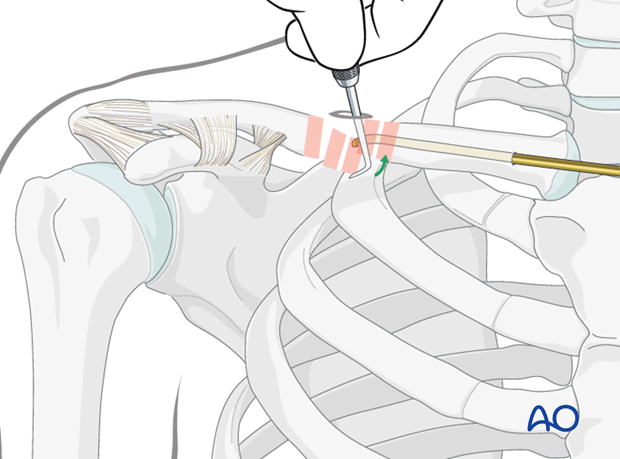
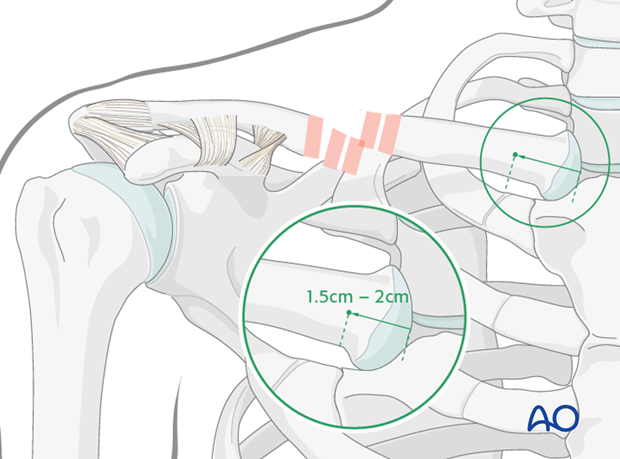
Using image intensifier, the entry point is obtained using a 2.5 mm drill bit in the anterior cortex of the medial clavicle 1.5-2.0 cm lateral to the sternoclavicular joint.
The entry point is enlarged with a small awl in a lateral direction to allow for ease of insertion.
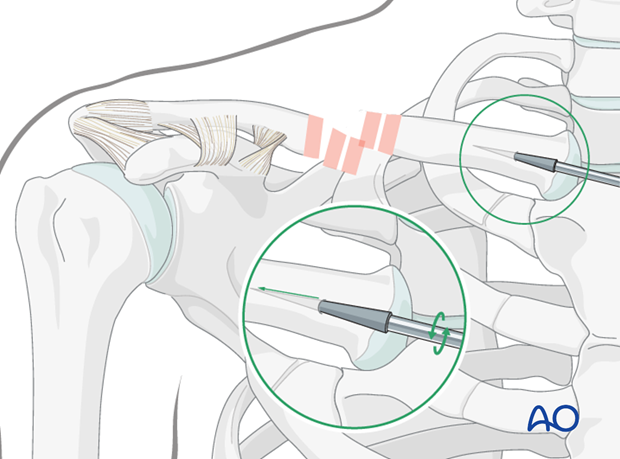
A 2.0 - 3.5 mm titanium elastic nail designed for intramedullary nailing, used for this or other applications, is inserted then with the aid of the universal T-handle chuck. The nail is manually inserted with oscillating movements under image intensifier control and advanced to the fracture site. If significant resistance is encountered, reassess the position of the nail to redirect and complete the passage of the nail.
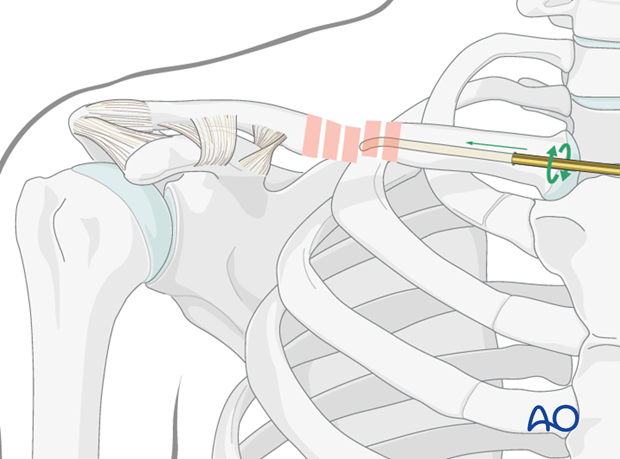
The tip of the nail has a slight curve, which will assist its passage into the lateral fragment.
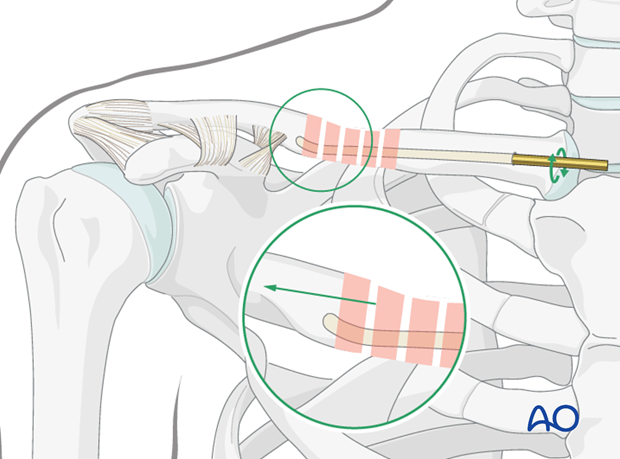
The tip of the nail is advanced as far lateral as possible without perforating the cortex.
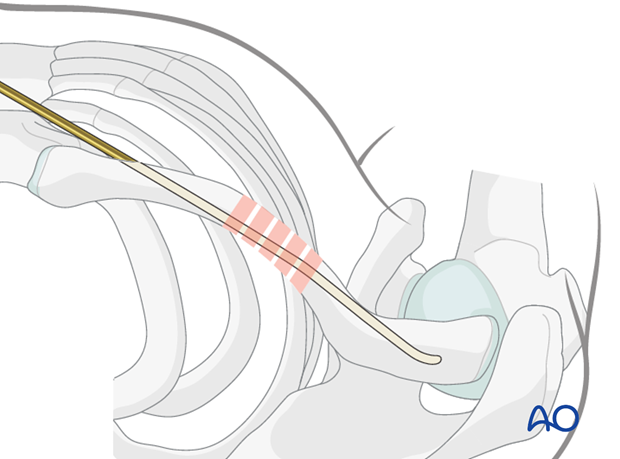
The medial end of the nail is then cut and buried subcutaneously or slightly proud depending on surgeon preference.
A threaded end cap may be used and inserted over the medial end of the nail to prevent backing out of the nail.
Hardware removal is only indicated if the nail is prominent and threatening or irritating the overlaying soft tissue at the entry point or perforating the far cortex.
4. Aftercare
The aftercare can be divided into 4 phases:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













