ORIF - Compression plate with lag screw
1. Introduction
Goal of treatment
The goal of treatment for a simple two-part fracture of the shaft of the clavicle is direct bone healing. This requires anatomical reduction and absolute stability.
Note: This is the most common pattern. The deforming force on the medial end is the pull of the muscles and the deforming force on the lateral side is the weight of the upper extremity.
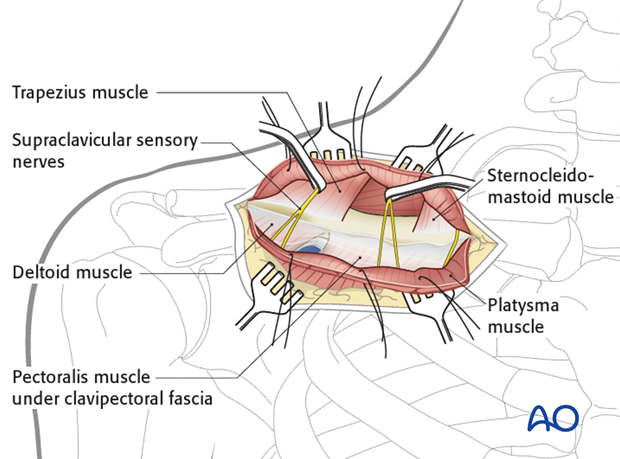
Beware of the major neurovascular bundle (subclavian artery, vein, and brachial plexus) running directly beneath the midshaft of the clavicle.
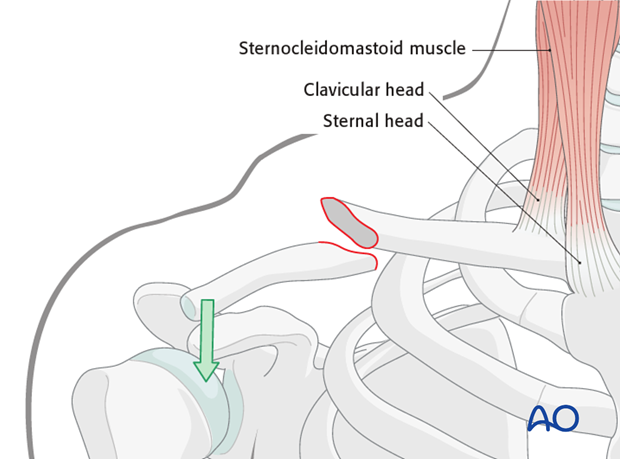
Other types of deformities may occur if the coracoclavicular ligaments are disrupted (eg, superior displacement of the lateral fragment).
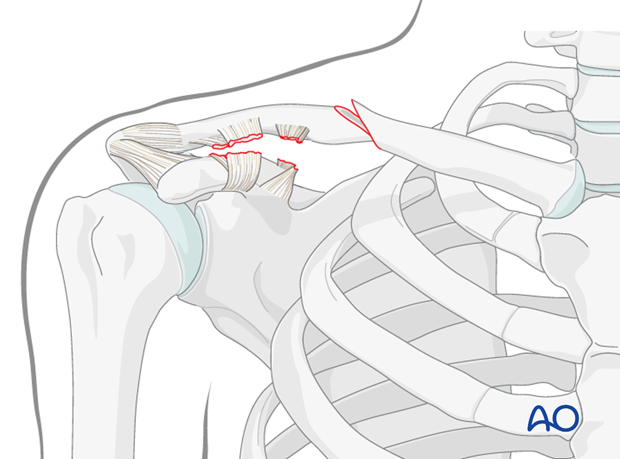
Plate and lag screw
Absolute stability can be optimally achieved by inserting a lag screw through the plate after primary axial compression.
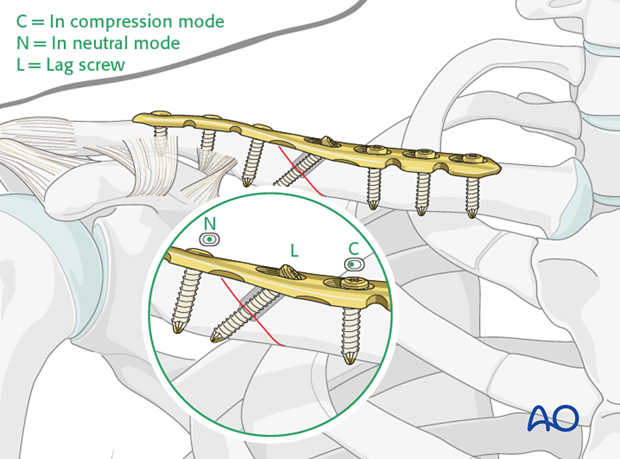
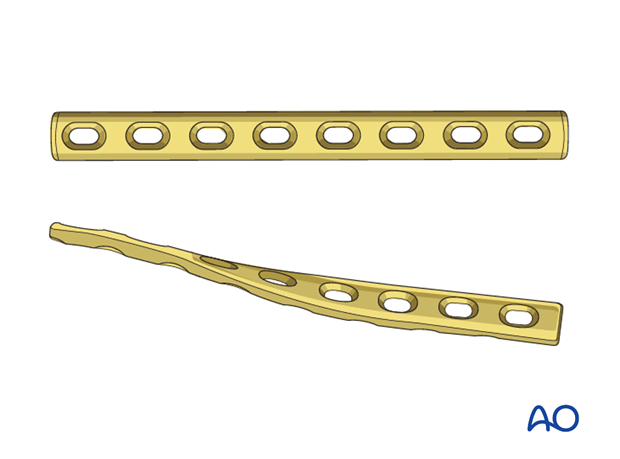
Plate alternatives
We will here show the procedure with a precontoured clavicular plate which has both a bend and a twist built into it.
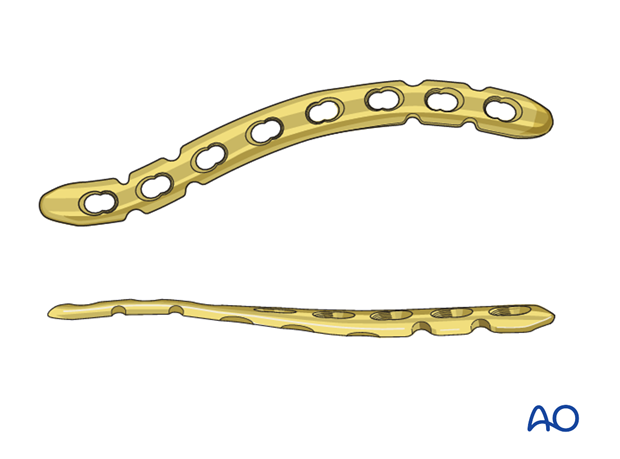
However, if a precontoured clavicular plate is not available, there are other options.
A straight plate may be used if it fits the clavicle (conventional or angle stable). If it does not, then it needs to be contoured.
This is best achieved with a slight twist at the midportion of the plate. This results in the lateral plate being applied superiorly and the medial portion anteriosuperiorly. A reconstruction plate which is easier contour may be used in smaller patients where the forces working on the plate are not as great.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient either in a beach chair or a supine position.
Approach
For this procedure an anterior approach is normally used.
3. Reduction and fixation
Reduction
Using the fracture interdigitations as a gauge for the reduction, obtain control over the proximal and distal fragments using reduction clamps. Apply gentle traction using a lobster clamp on the lateral fragment or the free draped arm and a derotation force, typically to the lateral fragment, to anatomically reduce the fracture.
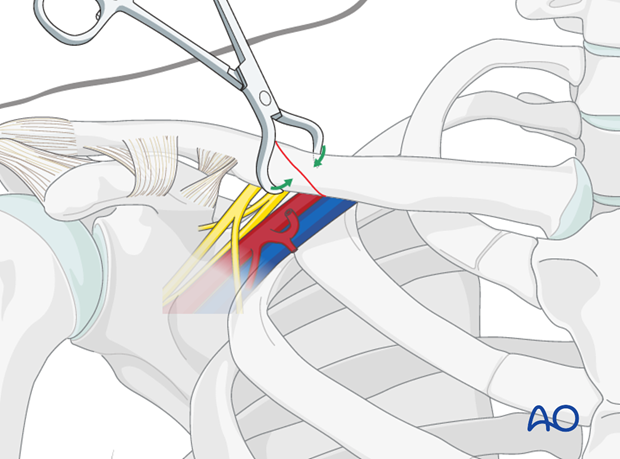
Maintaining provisional stability with an additional pointed clamp is helpful prior to the plate application. The clamp is ideally placed away from any eventual screw and plate placement.
The use of K-wires to assist in reduction and temporary stability prior to plate application has been described. However, this is not recommended as the surrounding vital neurovascular structures are in close proximity and would be at risk for injury.
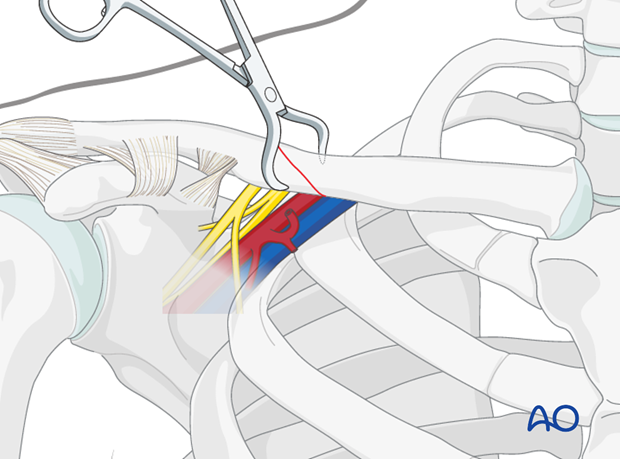
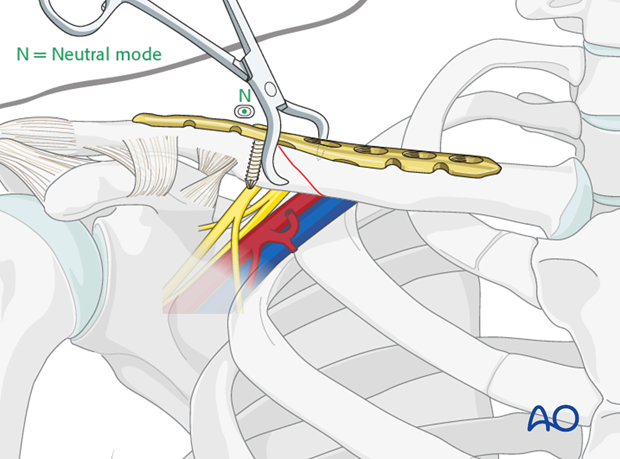
Plate application
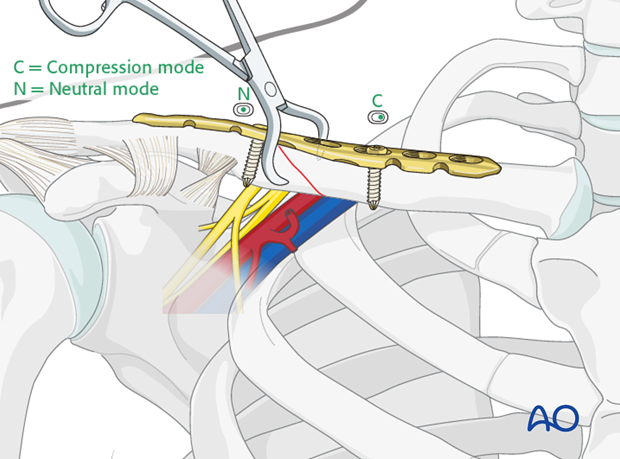
The plate is then fixed with a single bicortical position screw medially or laterally depending on the fracture pattern. The plate alignment and fracture reduction is confirmed.
A second eccentrically positioned screw is then applied on the opposite fragment in compression mode.
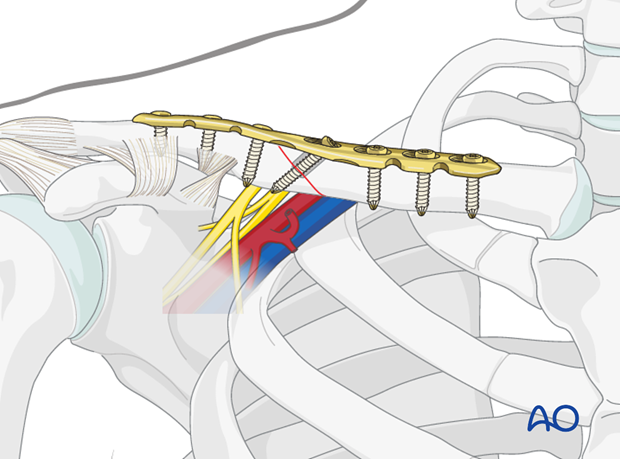
Lag screw insertion through the plate
If the fracture line is amenable to lag screw fixation through the plate, then further compression can be achieved. Inserting the screw through the plate adds torsional stability.
Before fully tightening the lag screw, the axial compression has to be released slightly to allow additional interfragmentary compression.
The loosened screw is then retightened.

Insertion of remaining screws
The remaining screws are then inserted in neutral position. Typically, a minimum of three bicortical screws in each segment is sufficient.
Note: Occasionally when the fracture location is more lateral or more medial, the bone quality near the metaphysis may not offer sufficient screw purchase. In these instances, a plate offering additional screw fixation may be required (eg, longer plate, periarticular plate, locking screws).
4. Aftercare
The aftercare can be divided into 4 phases:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













