Nonoperative treatment
1. Diagnosis
Decision making for nonoperative management
Patient considerations are extremely important when considering the diagnosis of calcaneal fractures. The surgeon must consider the patient and the fracture when making decisions about treatment.
Nonoperative management may be indicated in patients
- with minimal articular involvement
- with adequate maintenance of heel anatomy
- with medical contraindications to operative care.
Patient considerations
Patient considerations for nonoperative care include
- patients > 60 years old
- patients with medical diseases such as coronary artery disease or diabetes
- heavy smokers
It has been noted that patients who have secondary gain from impairment fail to achieve good outcomes after any form of treatment for calcaneal fractures.

Patient compliance
Few injuries are more devastating or have more long-term impact on a patient’s life. Patient and family education is crucial for enabling the patient to understand the significance of this injury. Important factors such as limb elevation, limb range of motion, smoking cessation and medical wellness (example: diabetic insulin control) allow patients to complete successfully required care pathways.
Fracture considerations
Indications for nonoperative treatment are:
- Less than 2 mm displacement of articular surface
- No gross varus or valgus malalignment of the hindfoot
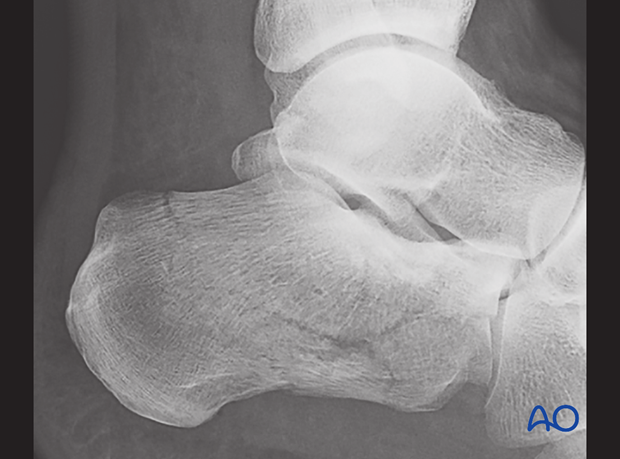
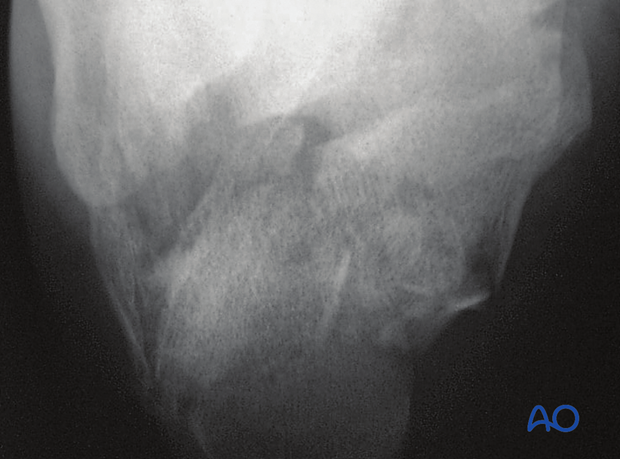
This image shows an extraarticular fracture with mild displacement in an older patient, appropriate for nonoperative care.
Undisplaced fractures have generally a very good outcome.
Radiology
Radiographic views
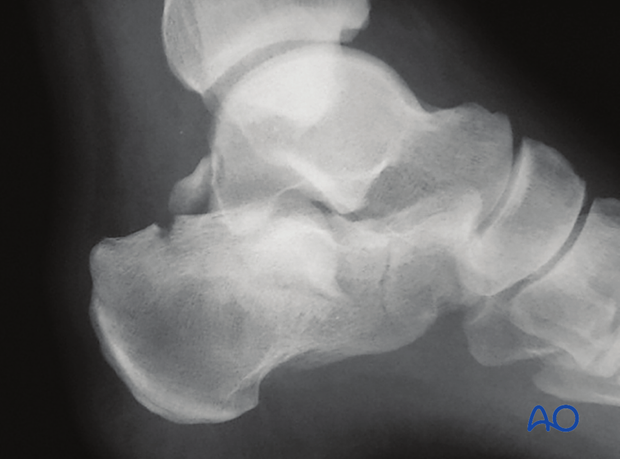
The radiographic assessment begins with 3 views of the foot as well as an axial (Harris) view. The basic fracture types, i.e. tongue-type vs joint-depression type, are best demonstrated in the lateral view (as in this image).
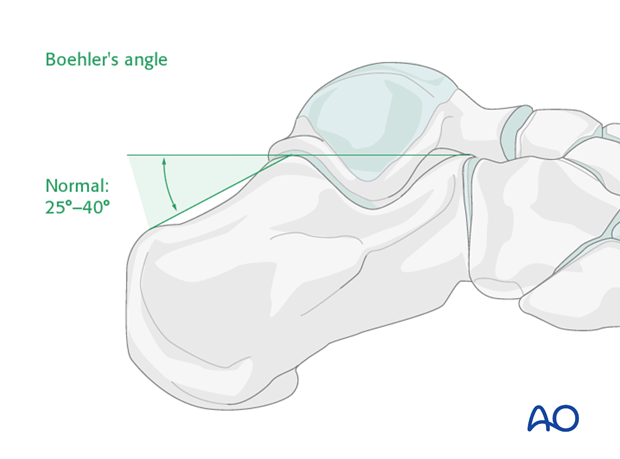
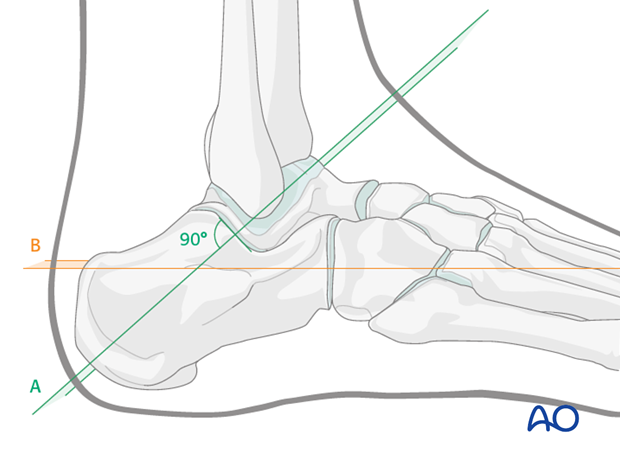
Böhler’s angle
A decrease in Böhler’s angle demonstrates the severity of joint injury and displacement (depression) as measured on the lateral x-ray. The normal angle is 25 degrees to 40 degrees. If this angle remains above 15 degrees, nonoperative care can be suggested.
Axial view
The axial view shows the primary joint displacement and angulation of the tuberosity as well as any increase in heel width.
This view is important intra-operatively to ensure that there is no varus in any calcaneal reconstructive procedure.
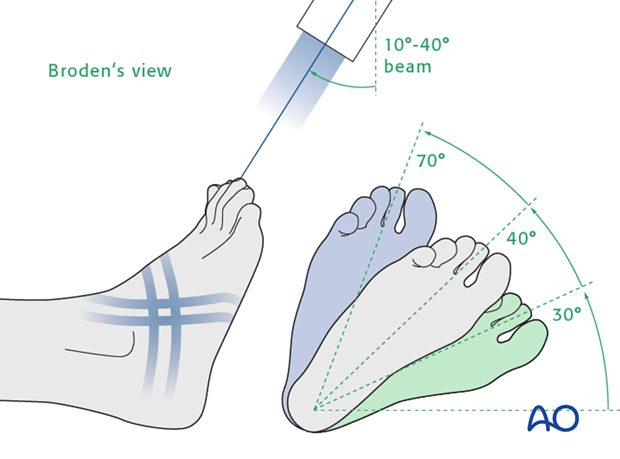
Broden's views
Broden's views are special calcaneal radiographhic projections to show the congruence of the subtalar joint.
They are taken at 30°, 50°and 70° to the horizontal.
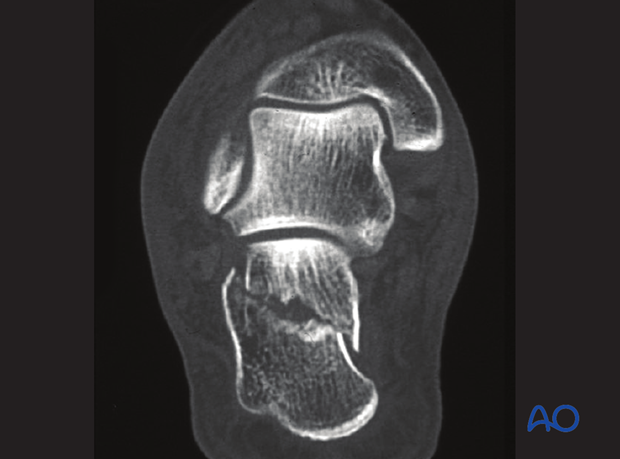
Computer-assisted tomography
Computer-assisted tomography is essential for accurate diagnosis and for surgical planning.
Axial CT images demonstrate fracture extension into the calcaneo-cuboid joint and tuberosity.
Coronal CT images depict the involvement of the posterior facet as well as shortening and position of the tuberosity.
Sagittal CT reconstructions can further elucidate the injury.
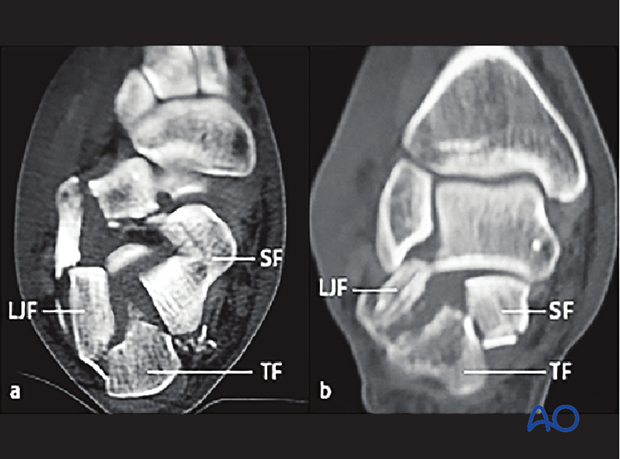
For best CT imaging careful foot position is mandatory.
As shown in the illustration the planes of reconstruction are A perpendicular to the post facet (semi-coronal) and B parallel to the sole of the foot (not metatarsal).
2. Soft-tissue principles
Soft-tissue injury
All heel fractures have a spectrum of soft-tissue injury. Rest, ice, elevation and compression will help in resolving the soft-tissue injury, and prepare the foot for definitive care regardless of fracture type and treatment type. Non-weightbearing is essential until the final treatment plan has been executed. Compartment syndromes occur. Their incidence and indications for treatment are currently not clear. If missed, late reconstruction is successful.

The amount of swelling is a good indicator of the degree of soft-tissue injury. As the swelling recedes, the skin begins to wrinkle both on the lateral and medial side. The wrinkling of the skin is a good indicator when surgery can be undertaken. Usually, one has to delay between 8-14 days before surgery can be undertaken without dire consequences. The maximum one can delay is about 3 weeks. After 3 weeks, the fracture becomes increasingly more difficult because of fracture healing.

Open fractures
These injuries are surgical emergencies requiring urgent debridement and reduction of bony fragments. The soft-tissue injury for the open wound is usually on the medial side. Often, temporizing percutaneous wire fixation is used to hold reductions while the soft tissues are healing before definitive bony reconstruction.
This image shows a severe medial soft-tissue wound which could be closed at 3 days.

3. Nonoperative care
Nonoperative treatment consists of continued patient compliance with smoking cessation, elevation and limb range of motion.
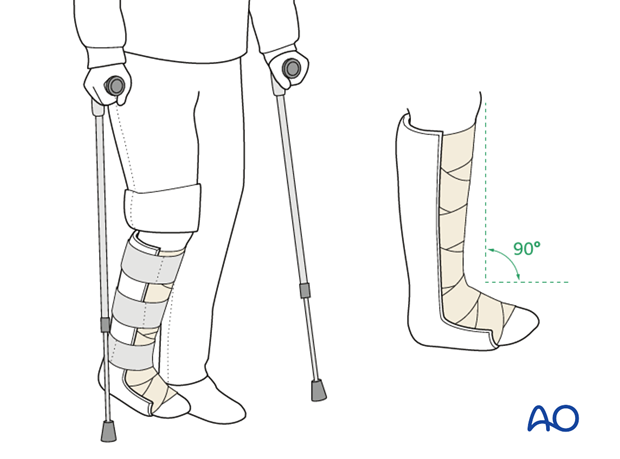
A posterior splint that allows for ankle and subtalar joint range of motion is advised at 2-5 days.
Weight-bearing is not allowed except toe touch for 6 weeks. After that, fracture healing is assured and progression to full weight bearing is allowed.
Radiographic follow-up at 6 weeks and 12 weeks is advised.
4. Aftertreatment
For aftercare and rehabilitation following nonoperative treatment please refer to your local protocol.













