ORIF - Screw fixation
1. Diagnosis
“Beak” fracture
This unusual displaced calcaneal fracture can be intra- or extraarticular. The most important feature of this fracture is its association with significant soft-tissue injury and potential soft-tissue complications. Because of marked disruption of the posterior soft tissues, if it does not present as an open fracture at the time of admission to hospital, the pressure from within on the posterior skin will soon cause it to break down and convert it into an open fracture.

This fracture occurs as a result of the Achilles tendon, which is extremely strong, avulsing a posterior fragment which may be either intra- or extraarticular. Occasionally, it is completely extraarticular but deserves the same operative treatment and reduction. If it is not reduced accurately, weakness from Achilles tendon dysfunction will occur.
This drawing shows an open intraarticular “beak” fracture, requiring urgent operative reduction for reasons of soft-tissue sparing and joint reduction.
Indications for operative treatment
The surgeon must consider the patient and the fracture when making decisions about treatment.
Operative management is indicated in patients with beak fractures
- with displacement of more than a few millimeters posteriorly
- present or impending posterior soft-tissue compromise
- no medical contraindications to operative care.
If the patient is medically safe for surgery, then immediate operative reduction is indicated to prevent this from becoming an open fracture.

Skin necrosis will occur within 6 h if not reduced.

Patient compliance
Few injuries are more devastating or have more long-term impact on a patient’s life. Patient and family education is crucial for enabling the patient to understand the significance of this injury. Important factors such as limb elevation, limb range of motion, smoking cessation and medical wellness (example: diabetic insulin control) allow patients to complete successfully required care pathways.
Radiology
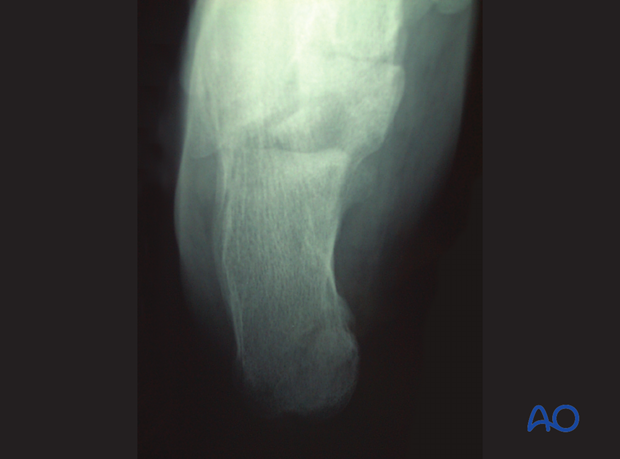
Radiographic views
Lateral ankle x-rays show the dramatic displacement of the posterior tuberosity of the calcaneus. This x-ray will demonstrate also whether or not this fracture extends into the subtalar joint, or is completely extraarticular, leaving the posterior facet uninvolved.

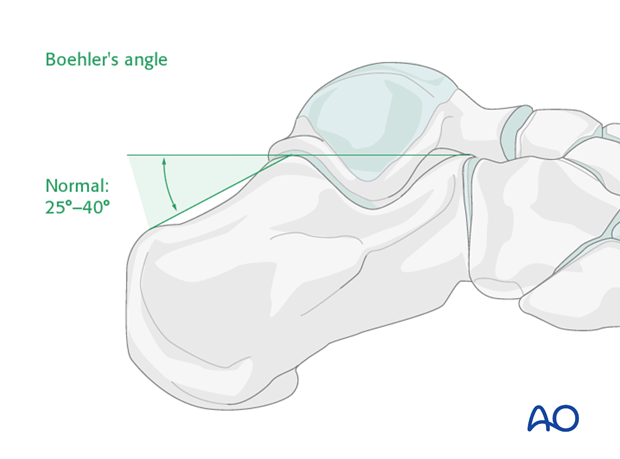
Böhler’s angle
A decrease in Böhler’s angle demonstrates the severity of joint injury and displacement (depression) as measured on the lateral x-ray. The normal angle is 25 degrees to 40 degrees. If this angle remains above 15 degrees, nonoperative care can be suggested.
Axial view
This view is difficult to interpret because the displaced tuberosity hides the injury as it is in the plane of displacement.
Computed tomography
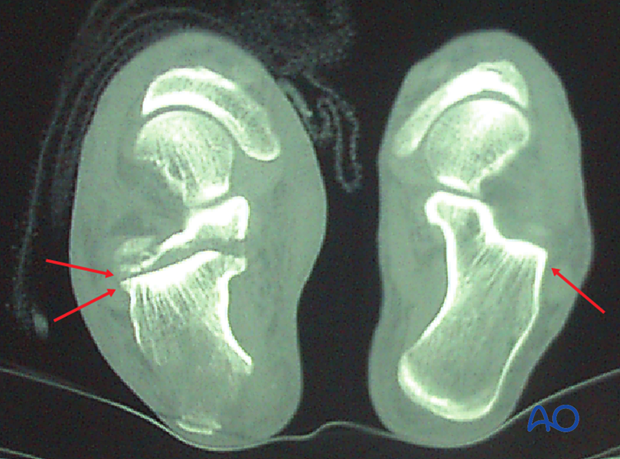
If there is time before skin compromise, a CT will be helpful to discern the exact amount of joint displacement. This CT shows a normal foot and an axial cut of a patient with a beak fracture, showing the double line of the articular surface which demonstrates the articular split.
2. Soft-tissue principles
Soft-tissue injury
All heel fractures have a spectrum of soft-tissue injury. Rest, ice, elevation and compression will help in resolving the soft-tissue injury, and prepare the foot for definitive care regardless of fracture type and treatment type. Non-weightbearing is essential until the final treatment plan has been executed.
Sometimes, delay is not possible because of a bony fragment pressing on the overlying skin and threatening immediate breakdown. When this occurs, one is not only faced with an open fracture, but necrotic soft tissue, which usually leads to a terrible scenario.

Without urgent debridement and reduction, this fracture soon penetrates soft tissues by skin necrosis. The photograph demonstrates a case with skin incision and the immediate exposure of the “beak” fracture. With careful immediate open reduction, the skin is salvaged.

3. Approach
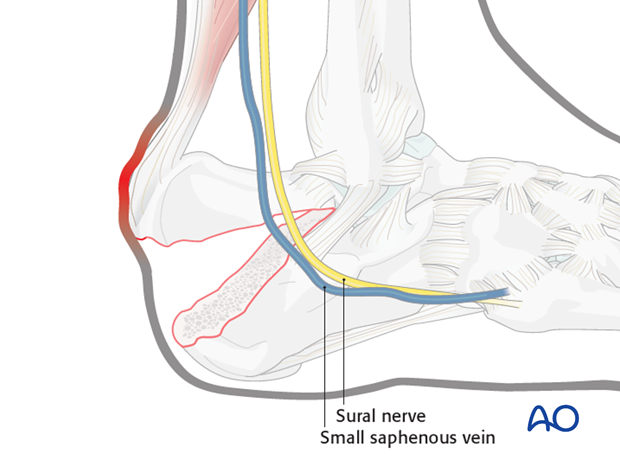
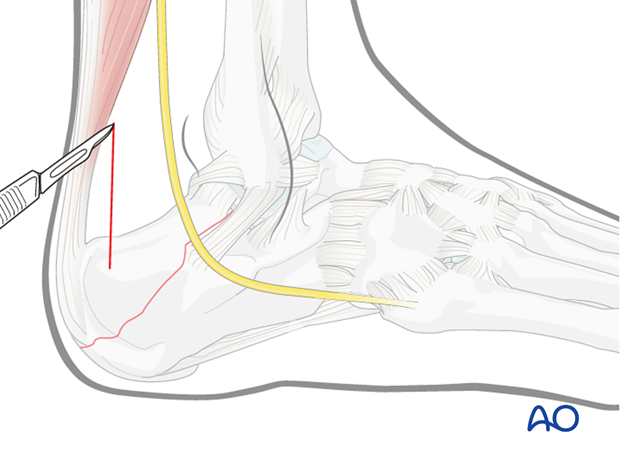
For this procedure a minimally invasive posterior approach may be used.
4. Reduction and Fixation
Reduction
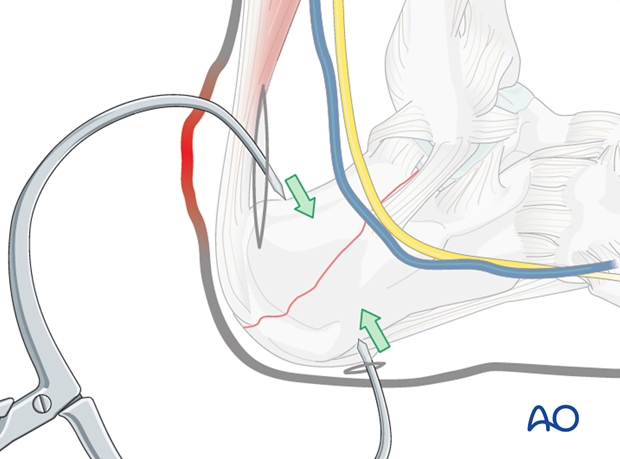
With the small posterior incision, the dorsal tuberosity can be seen and the fracture visualized. A large clamp is placed through the incision with one arm on the top of the tuber, and the other sharp tong through the heel pad.
By carefully closing the clamp, the fracture is reapproximated and reduced. The quality of the reduction is confirmed under the image intensifier.
In reducing the fracture, one must make certain that when the fragments are reapproximated, the subtalar joint is reduced anatomically. This must be checked carefully with the image intensifier.
Cortical lag screw placement
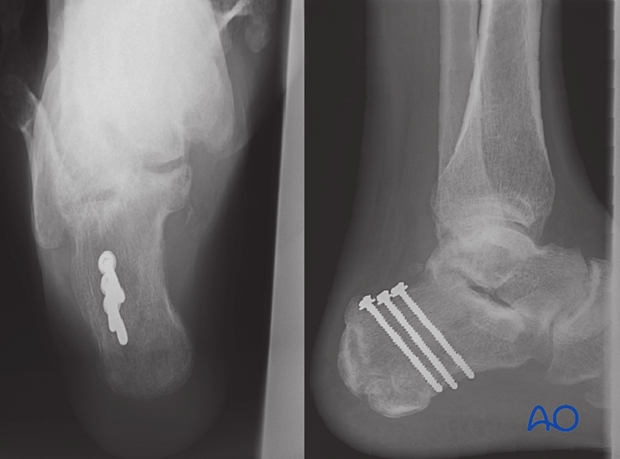
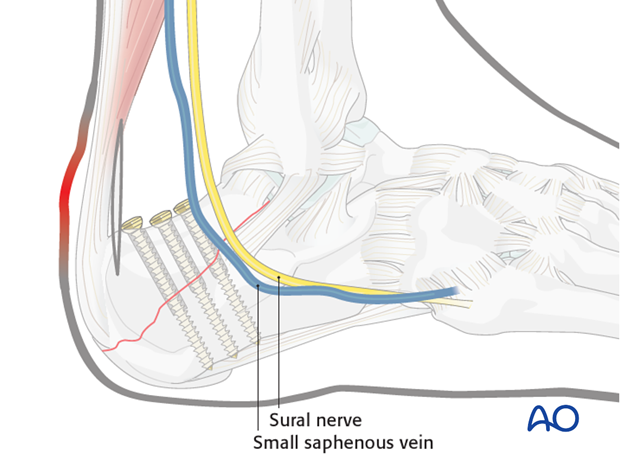
With image intensification and the fracture reduced, lag screws are placed perpendicular to the fracture line in standard fashion.
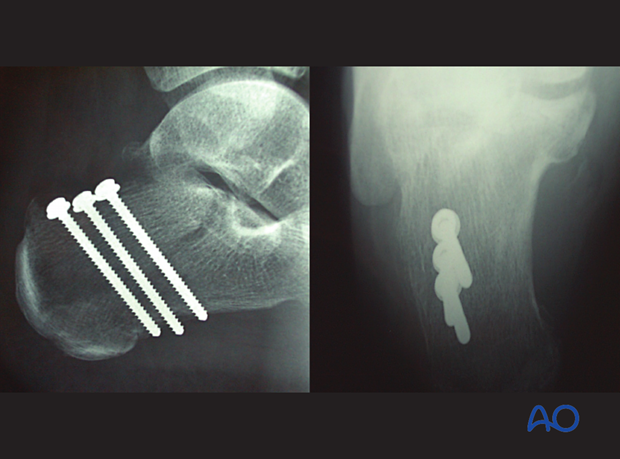
Two or three cortical lag screws are preferred and must be bicortical, using the thick plantar surface of the calcaneal tuberosity for effective purchase. These screws should be just anterior to the weight-bearing portion of the tuberosity with their plantar purchase.
Addition of washers may assist in weaker porotic bone, if necessary.
5. Aftertreatment
Initially, the patient’s foot and ankle are kept in a well-padded cast that maintains the foot in a neutral position. The cast neutralizes distracting forces to protect the lag screws holding the tuberosity. If these lag screws are not protected by the cast, they are likely to fail. A cast is mandatory.
The leg should be elevated through the first number of weeks.
Weight bearing is delayed until 6-12 weeks, depending upon the degree of comminution and the adequacy of the fixation.
Radiography including lateral and axial views is obtained at 6,12 and 26 weeks.
Follow-up
With immobilization for 8 weeks, these x-rays demonstrate successful healing and loss of the fracture line. As this is an injury that occurs with tension, the screws should be protected with a cast for a minimum of 8-12 weeks, and activity restricted for at least 16-24 weeks.