Extended lateral approach to the calcaneus
1. Indications
The extended lateral approach to the calcaneus is the most common approach used for displaced intraarticular calcaneal fractures. Over 90% of calcaneal fractures with displaced joint fragments can be serviced by this approach.
The calcaneus can present with an enormous variety of fracture configurations. However, this approach, used with care, is the safest and most utilitarian.
2. Anatomy
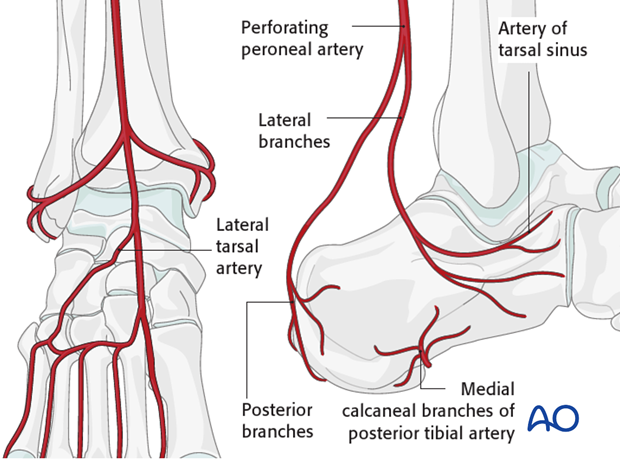
Vascular supply
It is essential to understand the vascular supply to the subcutaneous tissues of the lateral hindfoot as wound-healing complications are common after using this approach. The perforating branches of the peroneal artery contribute to the vascularity of the lateral skin and soft tissue of the foot. The undermining of skin edges runs the risk of skin edge necrosis and therefore full-thickness flaps have to be developed to prevent this complication.
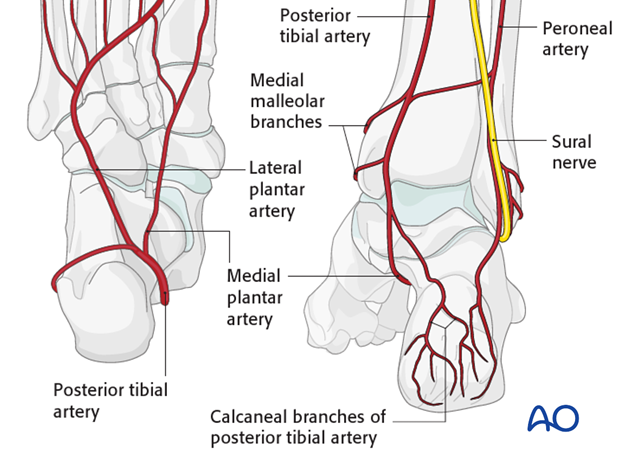
The lateral calcaneal artery is responsible for the majority of the blood supply to the corner of the L-shaped flap of this approach.
The heel pad is mostly supplied from the posterior tibial artery branches medially.
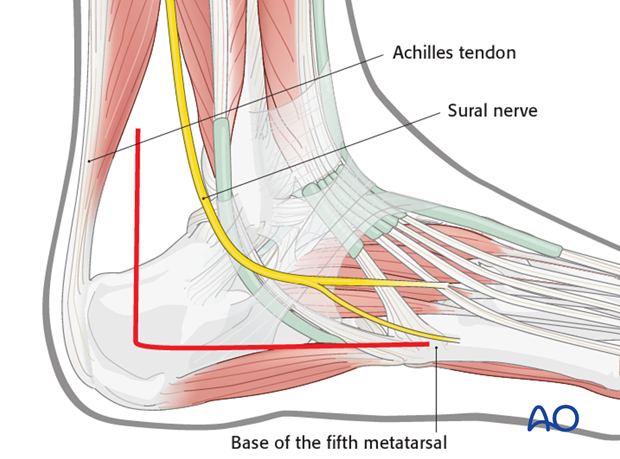
The sural nerve needs to be protected in the horizontal part of the approach.
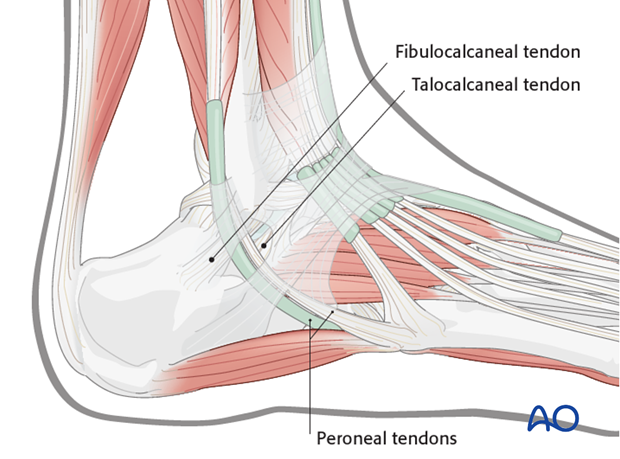
Ligaments and tendons
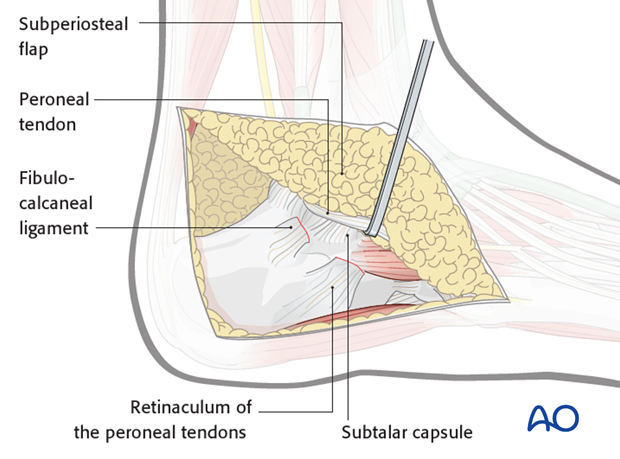
The peroneal tendons are on the lateral side of the calcaneus. Note the position of the retinaculum and of the fibulocalcaneal and talocalcaneal ligaments.
In raising the full-thickness L-shaped flap, one detaches the retinacular attachment as well as that of the fibulocalcaneal and talocalcaneal ligaments from bone.
3. Timing of surgery
Correct timing of surgery is the most important factor in preventing local wound complication. Early surgery leads to wound edge necrosis. Therefore, great patience is required to optimize the local surgical environment.
Skin blisters should be observed and carefully protected.
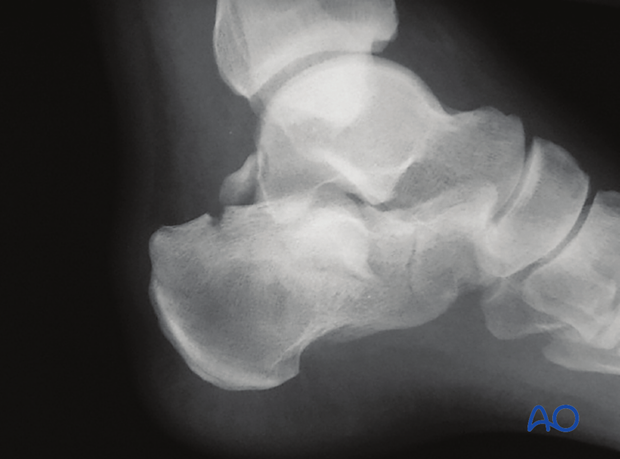
The image shows a foot 3 days after serious trauma, which is inappropriate for surgery.

The return of skin wrinkles to the lateral side of the foot should be used as a guide for the timing of surgery. Generally, 8-14 days is the optimal time for surgery. Longer delays may be associated with increasing difficulty in obtaining a reduction and closing the surgical incision.
The image shows a foot 14 days after injury appropriate for surgery, with the “wrinkle sign” present.

4. Incision
Skin incision
The vascular supply to the planned flap is a “watershed” area. More than in any other incision used for surgical exposures in trauma, the corner of the soft-tissue flap at the juncture of the longitudinal and vertical posterior incisions must be treated with infinite care.
The posterior arm of the incision is placed midway between the fibula and Achilles tendon. The horizontal arm is placed in line with the base of the fifth metatarsal.
They meet at a corner where skin handling must be optimized.
Development of flap
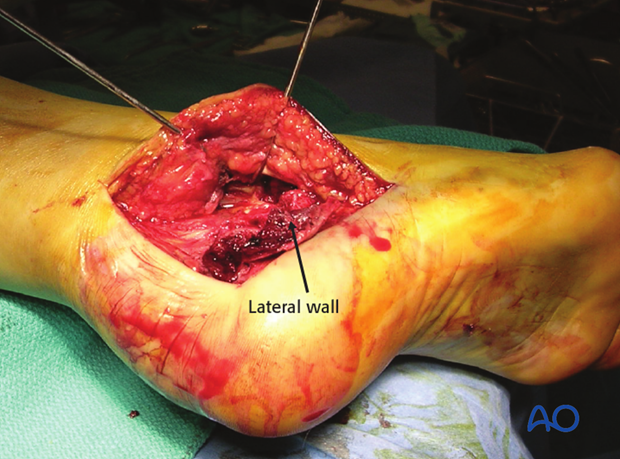
At the corner, the incision is made directly to bone to ensure that one raises a full-thickness flap. The undermining of the edges must be avoided. One creates a full-thickness flap and, as the flap is developed, one divides the retinaculum and detaches the fibulocalcaneal and talocalcaneal ligaments from bone. The peroneal tendons and the sural nerve are within the flap and are not exposed. As the flap is developed upwards, one exposes the subtalar joint and the sinus tarsi.
Capsulotomy
The subtalar joint capsule is opened.
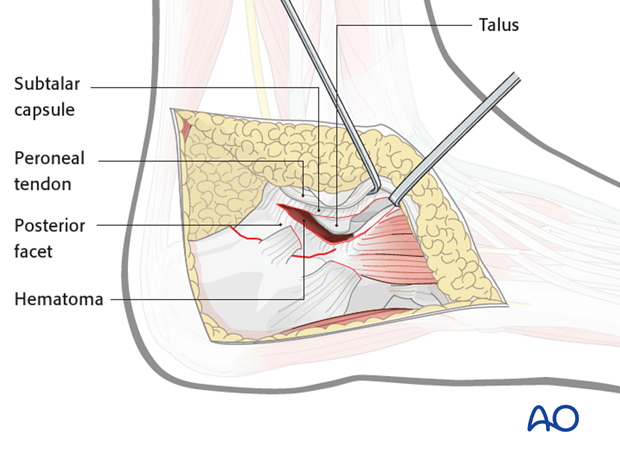
Hematoma is removed and retraction K-wires are placed into the lateral process of talus and fibula.
5. Wound closure
Soft-tissue closure should be carefully performed. Two-level closure over a hemovac drain is standard. An absorbable stitch is used for apposition of subcutaneous tissue. One must make certain that there is no excessive tension on the distal corner of the incision and advancement of the flap may be necessary. An interrupted Allgöwer-Donati stitch is used to close the skin.
The skin edges should be apposed and not strangulated.

Healing complications
Wound healing problems occur roughly 15% of the time with the apex of the wound being the most common area affected. This can present as wound necrosis, or minor soft-tissue infection, but can progress to wound slough or deep-bone infection. Careful observation, antibiotics, wound care and debridement will manage most of these incision concerns.














