Intradural repair
1. General consideration
A bifrontal basal craniotomy after coronal skin incision offers the possibility of inspection of the whole anterior skull base including the two lateral as well as the central portions. Special care should be taken to perform the craniotomies as far basal as possible, even if the frontal sinus has to be opened. Correct management of the frontal sinus is highly recommended to avoid possible postoperative complications, such as mucoceles. This can be accomplished in two ways:
- Complete cranialization of the frontal sinus followed by a careful reliable separation of the paranasal sinus and nasal cavity from the cranial fossa.
- Reconstruction of the frontal sinus can be considered in selected cases. This requires that the nasofrontal duct can drain.
Note: To achieve a real reliable closure of dural defects on the anterior skull base a microscopic intradural inspection as well as microsurgical repair is highly recommended.
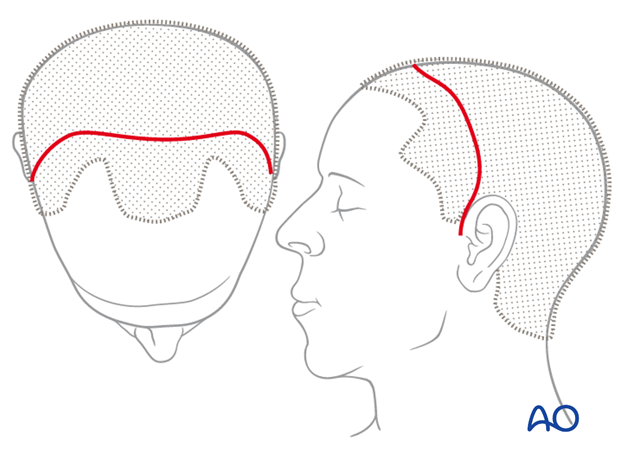
2. Approach
For this procedure the coronal approach is used.
3. Frontobasal repair using pedicled periosteal flap
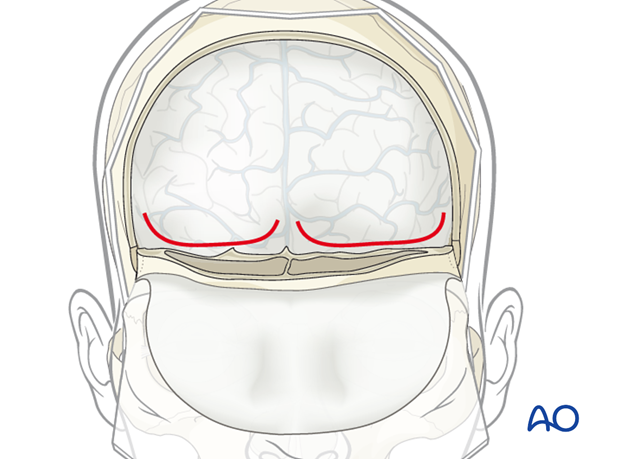
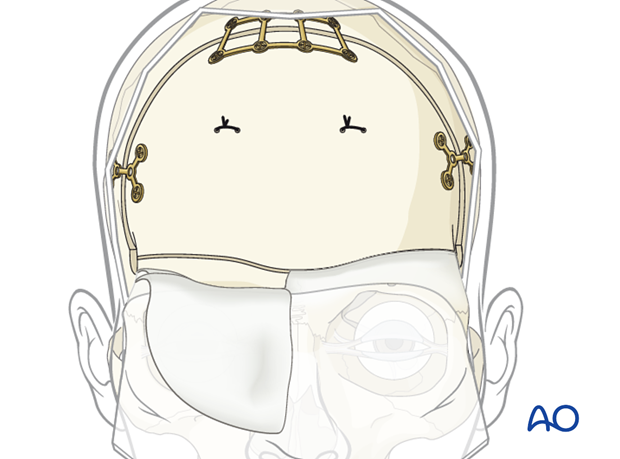
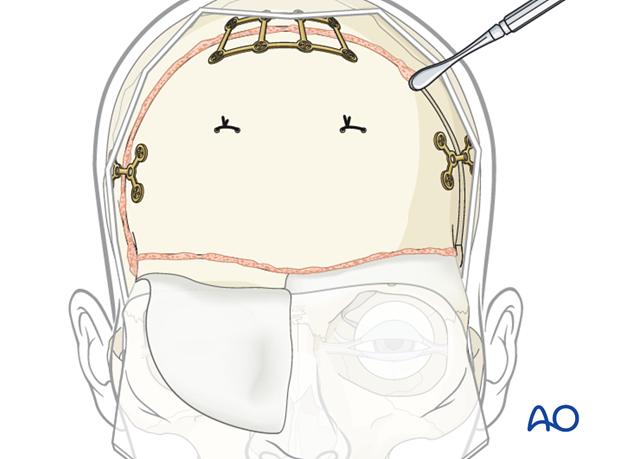
Open the dura by making a curvilinear incision on one or both sides of the superior sagittal sinus (SSS) starting from SSS going laterally at the level of the skull base.
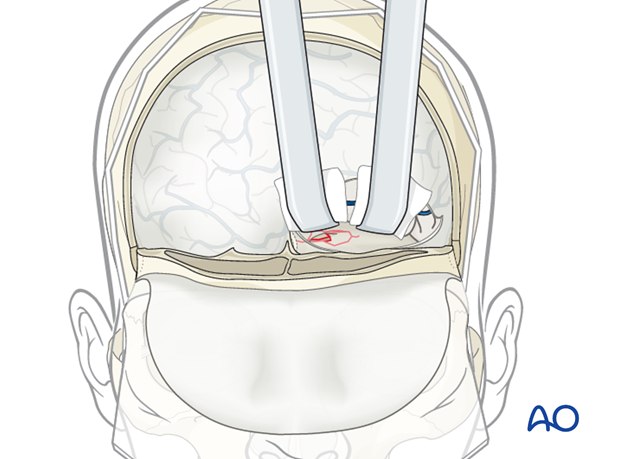
Elevate the frontal lobes using one or more retractors. The surface of the brain is protected by neurosurgical cottonoids. The use of magnification is recommended.
Inspect the dura of the whole anterior fossa and locate the exact location of the defect. Inspect carefully for evidence of brain or vascular injury and, of course, take great care to avoid creating such injuries.
In case there is any perforation by bone fragments either remove them or smooth them using cutting forceps or special instrumentation.
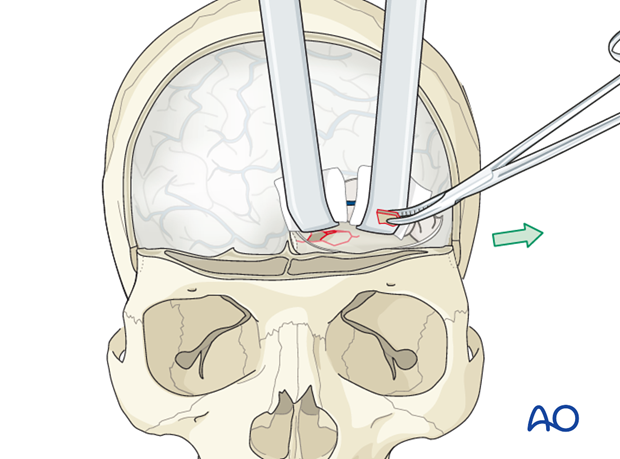
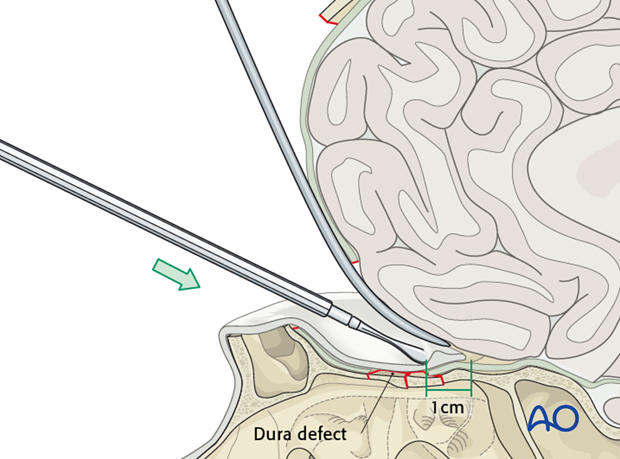
Inset the pericranial flap in that way that the defect is covered by the flap including a margin of at least 1 cm, when possible.
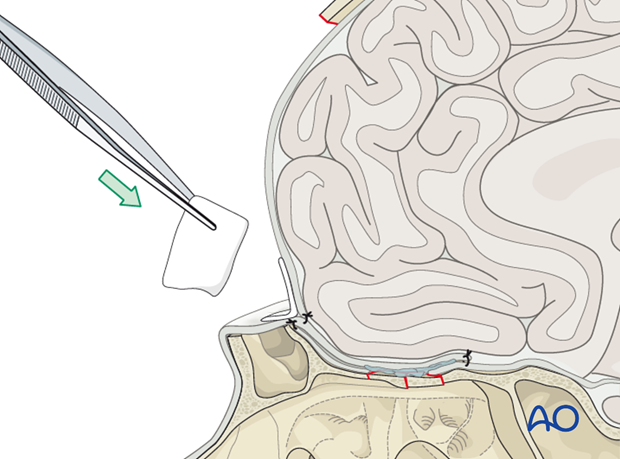
The intradural positioned flap is fixed by primary suture to hold it in place.
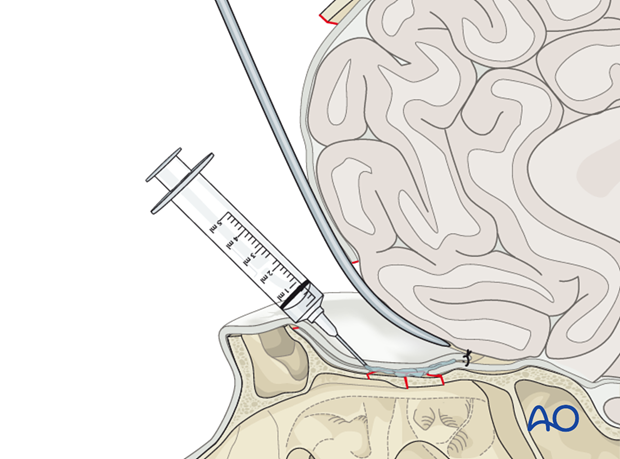
In addition the use of fibrin glue and collagen-based tissue sealant techniques under the pericranial flap is highly recommended in order to achieve a watertight closure.
The pericranium is also sutured to the upper free margin of the dural incision.
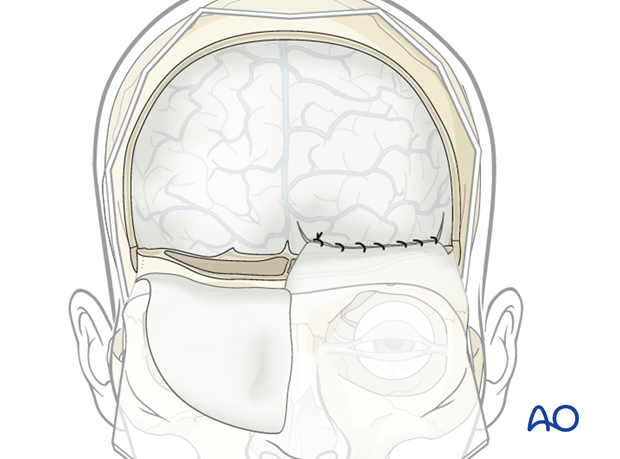
Whenever possible, the flap should also be sutured to the outer dura margin.
To achieve a watertight closure, the use of collagen-based sealants applied to the anterior suture line is highly recommended.
Tacking the dura to the bone flap is highly recommended to avoid possible postoperative epidural hematoma.

Replace the bone flap using internal fixation in a stable three point fixation technique.
Pearl: reconstruction of the bone defect
Bone substitute putty can be used to fill in the residual bone defects in order to avoid a cosmetic deformity.
4. Aftercare following open management of skull base fractures
General postoperative care
- Intensive care 24 hours
- Hospitalization 5-8 days (to rule out reoccurrence of CSF leak)
- The use of broad-spectrum antibiotics during and after the procedure for the next 5-7 days is recommended.
- Radiologic control examinations are performed routinely the next day after leaving the intensive care unit.
- Patient follow-up after discharge. The patient is seen 4 weeks after, and if necessary, for the long-term follow-up a year postoperatively.













