Introduction
1. General consideration
Current standards of care for trauma patients, whether polytraumaor only with craniomaxillofacial injuries, follow the Advanced Trauma Life Support (ATLS) protocol relating to Airway, Breathing, Circulation, Disability, and Environment in that sequence. In the polytrauma patient, on admission a number of lesions take higher priority than the craniomaxillofacial lesions. Craniomaxillofacial injuries need to be diagnosed, a treatment plan has to be established, and a sequence fitted into the total treatment plan for the patient at an early stage.
The patient’s general medical condition and age may be reason for deviation from the principles suggested in this module of the AO Surgery Reference.
The spectrum of midfacial fractures has significantly changed over the last decades. Depending on the socio-economic, geographical and environmental specifics, the attention towards occupational health and safety, education and prevention, protection measures (eg, in automotive vehicles and sports, etc.) and awareness of the individuals to prevent injuries have been increased. A good example is that the frequency of the classical dish face lesion has been drastically reduced in car accidents by the use of safety belts, air bags, and shock absorbing materials used for steering wheels and dashboards.
Particularly in midfacial fracture repair Paul Manson’s quote: “you never get a second chance” has to be kept in mind, ie, the time frame regarded appropriate for primary fracture treatment is limited to 2 weeks (not including accompanying complications requiring immediate treatment, such as dentoalveolar trauma or post-traumatic visual loss). As soon as the general condition of the patient allows, definitive treatment should be undertaken. After 2 weeks, the treatment is regarded as delayed and thus has to follow the protocol of secondary post-traumatic reconstruction. Secondary reconstruction is not a current focus of the AO CMF Surgery Reference.
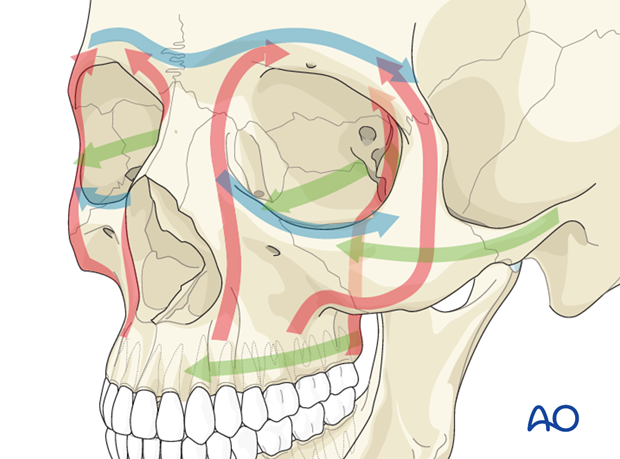
It is not so much the fracture morphology in the midfacial area that limits the intended treatment but mainly the preexisting general health status and the severity of associated accompanying injuries or in the vicinity of the midface (optic nerve trauma, CSF leakage, bleeding, etc) or in independent locations. Regardless the severity and possible variety of fracture types in the midfacial area the guideline for a successful restoration is reconstruction of facial buttresses and prominences, recontouring of bony cavities (eg orbit), and reestablishing occlusion.
2. Fracture classification
The Le Fort classification is a historic classification still widely used to classify midfacial fractures. The Le Fort classification (René Le Fort, 1869-1951, France) is based upon experiments where cadavers were exposed to frontal impacts. This was one of the first experimental trials on maxillofacial trauma. The cadavers were dissected and analyzed after their injury and the Le Fort I, II and III fracture patterns derived. Apart from the Le Fort classification, the Markowitz classification is used to describe injury patterns in NOE fractures.
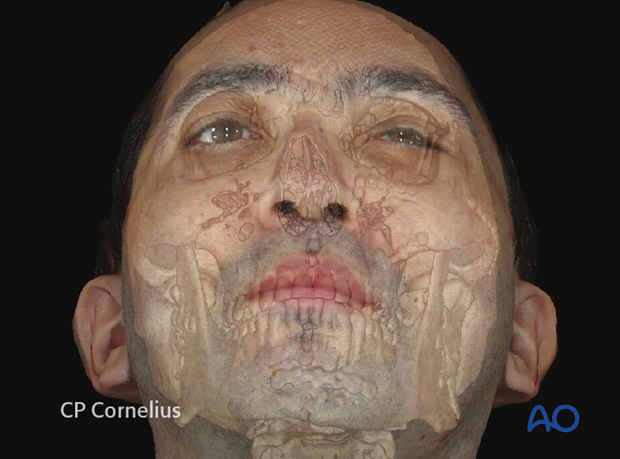
The unique situation of the midface is its complexity of interaction of hard with soft tissue. Out of twelve cranial nerves, six address the orbital area (CN II, III, IV, V, VI, and VII). Furthermore, in the midface, form, function, and esthetics are interdependent; even minor dislocations may be obvious to everyone.
The complexity or simplicity of a fracture in the midface is not only based on the fracture morphology (ie, fragment size, number, dislocation) but on the degree of injury to the soft-tissue envelope.
The range of combined midfacial/panfacial fractures is enormous. This is due to the variety in possible mechanisms which occur during impact leading to the midfacial injury. In general, low velocity trauma less often leads to severe midfacial fractures than high velocity trauma.
3. Imaging
With the availability of modern imaging technologies, the imaging analysis of the individual fracture pattern shows a variety and complexity that does not always conform to the above mentioned historical classifications. The gold standard for assessment of an individual fracture pattern today is voxel-based 3-D data sets (CT and cone beam). It is strongly advised to obtain postoperative CT scans to assess the surgical result. Because of the enormous benefit of CT documentation and the further development of cone beam technology, more and more surgeons are now recommending intraoperative imaging to assess proper reduction and implant positioning.
Examination of the craniofacial skeleton vastly benefits from 3-D imaging and interactive image analysis. The modern surgeon should be trained to use the DICOM voxel data set for multiplanar and 3-D image analysis. As well as professional software, a variety of DICOM viewers can be freely downloaded from the internet to start using radiological information. (Click here for a listing of freely available healthcare software including DICOM viewers). This is the only way to unlock the barrier interface of filtered information between radiologist and surgeons. The modern surgeon should be able to use full radiological information and not a limited selection of print outs or digitized views.
The surgeon thus changes his or her former role as a consumer of radiological information to interpreter of this data set. Having implemented computer assisted fracture assessment, much more detailed preoperative information is available to the surgical team. Radiological information acquired intraoperatively can be compared with different data sets (obtained pre- and postoperatively) via image fusion.
If no adequate visualization software for the DICOM datasets is available, then CT axial, coronal, and oblique parasagittal views of the midface for simple fractures, with 3-D views for more complex fractures are recommended.
Plain x-rays should only be considered appropriate if CT is unavailable or if distinct information for hard-tissue structures involved such as dentition (dental x-ray, orthopantomogram (OPG)) is required. MRI or ultrasound can be helpful in some specific questions related to soft tissues but is in most cases not included in standard diagnostic workup (one exception is optic nerve sheath hematoma detection).
4. Biomechanics of the midface
Introduction
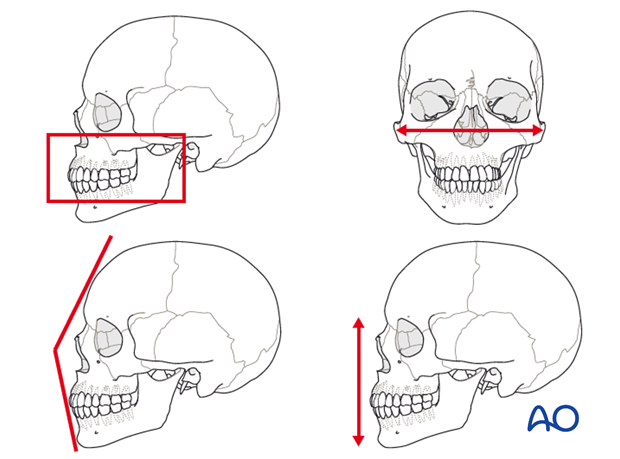
Basically, the midface equates to a tent, where the tent poles represent the bony midface and the tarpaulin represents the overlying soft tissues. However, the vectors of the midface address all three dimensions ie, vertical, sagittal, and transverse, which makes it much more demanding than the construction plan of a tent.
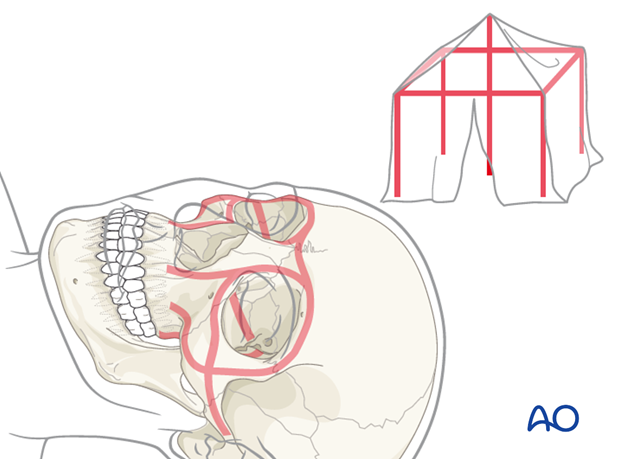
The reconstruction sequence to reestablish midfacial pillars and dimensions begins with establishing the most reliable reference structures. This can be occlusion, an outside-to-inside (“Joe’s outer frame”, Gruss 1986) or an up-to-down procedure as a first step.
Every under- or overcontouring of the bony midface in primary fracture repair results very likely in unfavorable projection of the soft-tissue mask and this again results in an esthetic compromise. In addition, functional disorders may follow such as malocclusion or orbital dysfunction.
5. Principles
Airway
Intraoperative MMF necessitates nasotracheal intubation. If nasotracheal intubation is not feasible, submental/submandibular intubation and/or tracheostomy should be considered.
Surgical principles
Dental occlusion is the most important parameter in reestablishing facial contour, reduction of fracture, and obtaining postoperative chewing function. The most common means of placing the patient into maxillomandibular fixation (MMF) is the application of arch bars. Click here for further details on applying MMF/IMF. In many cases of Le Fort fracture the maxillary fracture may require reduction by disimpaction. Various instrumentations may be necessary in order to properly achieve the position of the maxilla. The instrumentation that may be used include the following: Rowe’s disimpaction forceps, “Stromeyer” hook, Tessier retromaxillary mobilizers.
A second surgical principle is to achieve anatomical correct repositioning of all midfacial bones. The height, width, and projection must be reestablished. Successful reconstruction of midfacial fractures is obtained by reestablishing the midfacial buttresses. If available, dental casts, stereolithographic models, and/or premorbid photographs may be useful guides for treatment.
As a general principle, all fractures should be exposed and reduced before plating.
The midfacial region is possibly the most demanding region in terms of surgical reconstruction and also one of the most controversial regions in terms of how to provide appropriate reconstruction.
It is up to the individual surgeon to determine the appropriate treatment protocol for each patient, including the selection of appropriate hardware for fracture fixation.
Complexity of fracture fixation is not only determined by fracture morphology, including the number of fracture lines, but also depends on the necessary approach, accessibility, visibility of the area of interest and the stability of the fracture reduction.
The number, size, and position of plates and screws might vary according to the biomechanical needs and individual fracture situation.
The placement of a skull in a sterile plastic bag, or the use of sterile artificial skulls for contouring plates, and technologies such as intraoperative radiologic imaging or navigation can be beneficial in restoring the proper anatomical form.
Pre- and postoperative 3-D imaging allows an objective assessment of the surgical result.